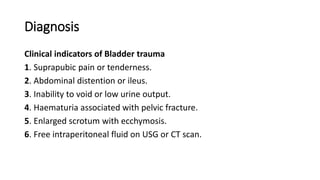
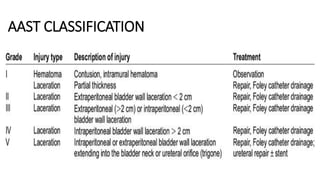
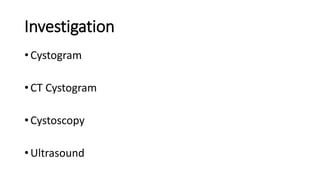
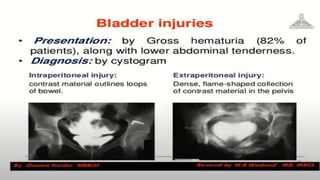
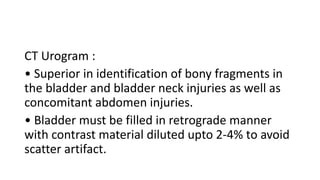
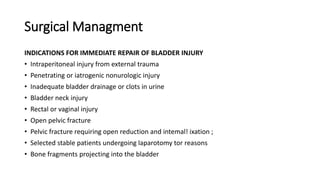
The document provides a comprehensive overview of bladder trauma, detailing its anatomy, mechanisms of injury, clinical presentation, diagnosis, and management strategies. It emphasizes the importance of timely identification and intervention, distinguishing between conservative and surgical approaches based on the nature and severity of the injury. Key diagnostic tools include cystography and CT scans, which help guide treatment decisions to prevent complications such as infection and peritonitis.