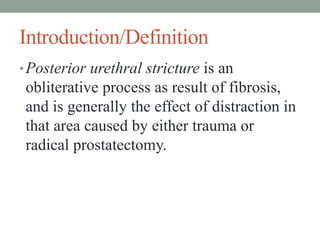
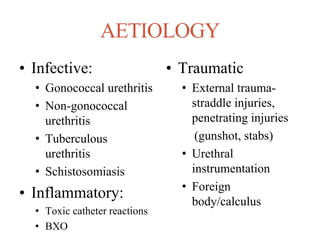
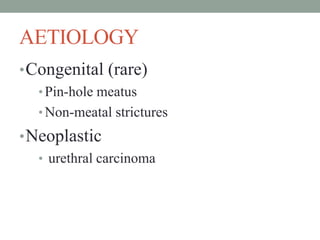
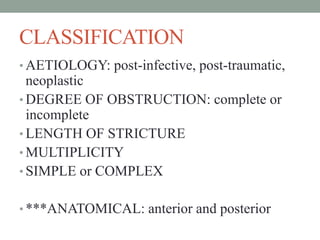
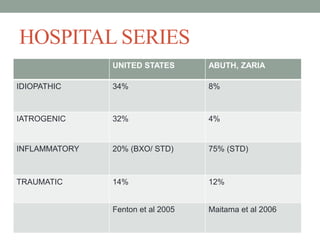
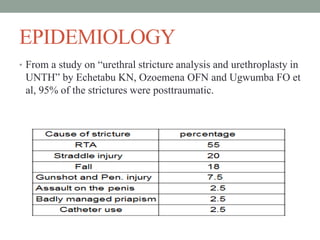
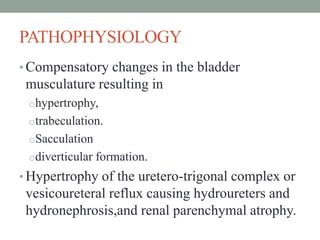
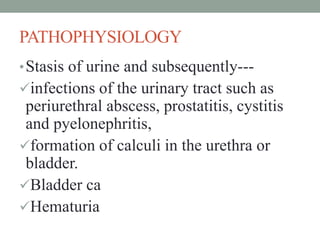
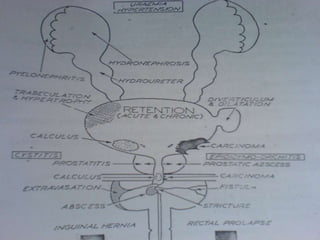
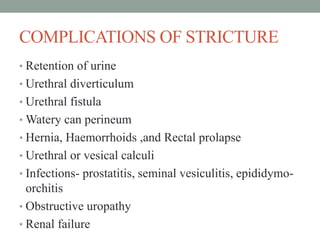
This document discusses urethral strictures, which are abnormal narrowings of the urethra caused by scarring that replaces the normal tissue. It outlines the main causes of strictures as infections, inflammation, trauma, and rarely congenital abnormalities or cancer. The pathogenesis involves any injury or inflammation that damages the urethral lining, triggering fibrosis and scar formation that narrows the urethral lumen over time. Left untreated, strictures can lead to complications like urinary retention, infections, kidney damage, and rarely fistulas or cancer. The document provides classifications and epidemiological data on urethral strictures.