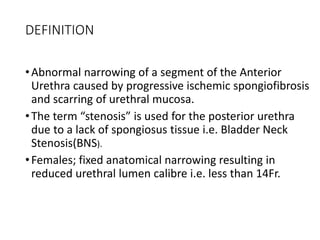
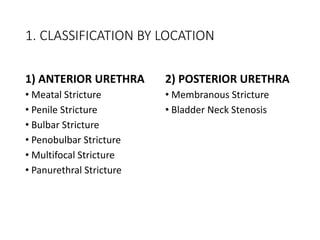
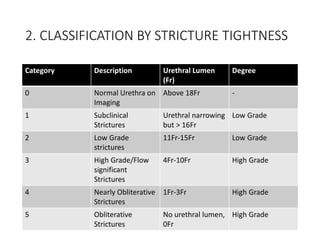
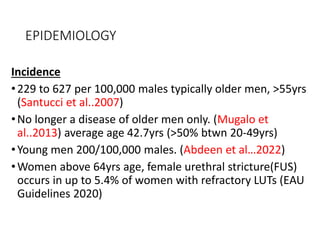
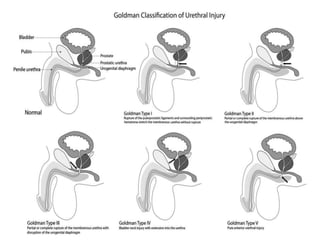
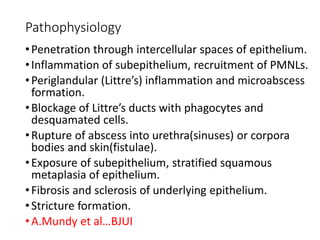
1) Urethral stricture is an abnormal narrowing of the urethra caused by progressive scarring that can result from trauma, infections, medical procedures or other causes.
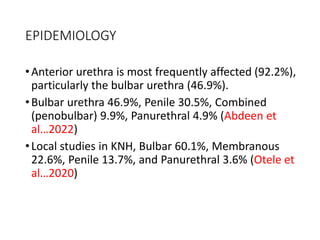
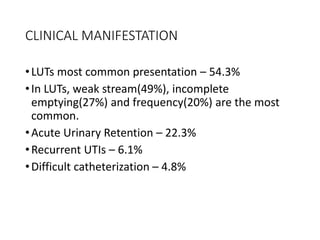
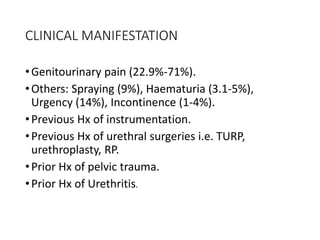
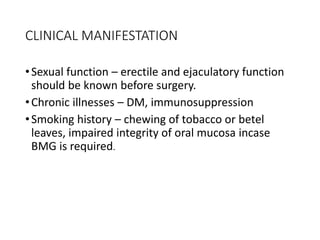
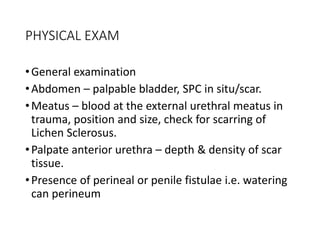
2) The document discusses the definition, anatomy, epidemiology, etiology, pathophysiology, classification and clinical manifestations of urethral stricture.
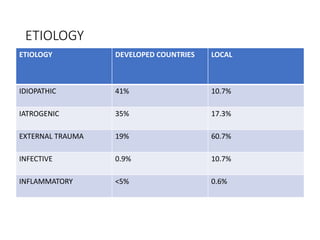
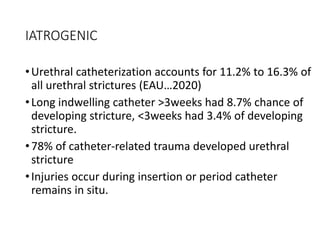
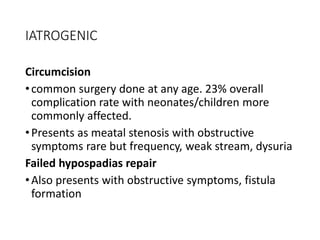
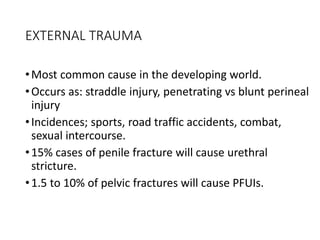
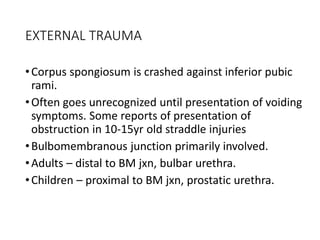
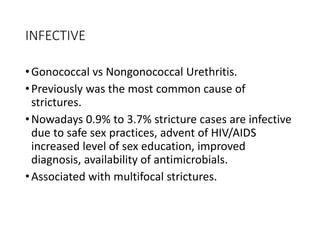
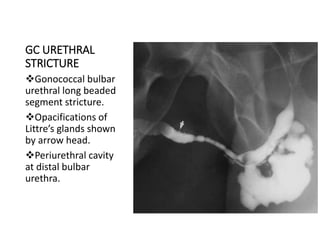
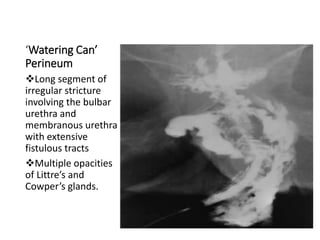
3) The most common causes of stricture vary between developed and developing countries, with iatrogenic factors, external trauma, and infections being the primary causes discussed in the document.