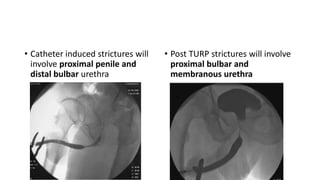
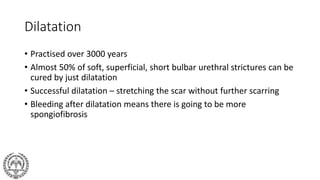
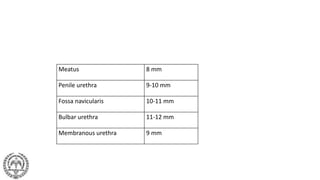
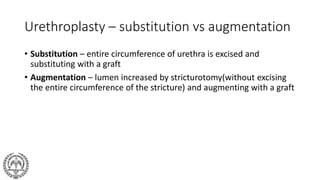
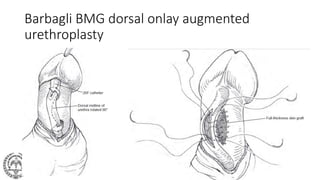
The document reviews male urethral stricture disease, detailing its definition, aetiology, pathology, natural history, diagnostic methods, and treatment options. It categorizes stricture causes, explores management techniques, and elaborates on surgical interventions like dilation, urethrotomy, and urethroplasty. The text emphasizes the importance of precise imaging for diagnosing stricture length and discusses various surgical grafts used in treatment.