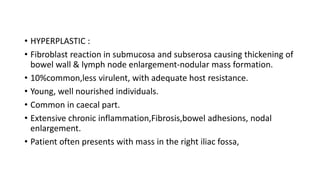
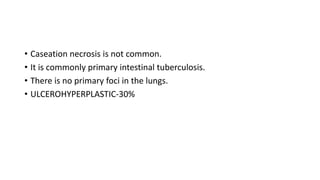
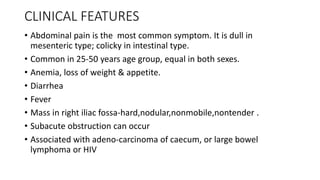
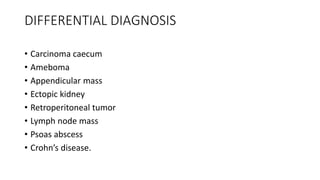
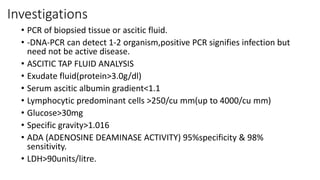
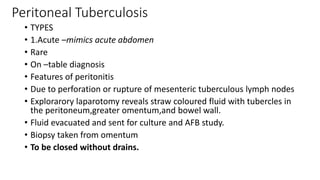
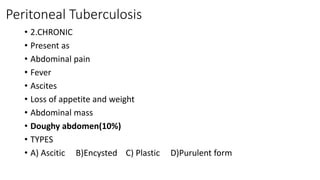
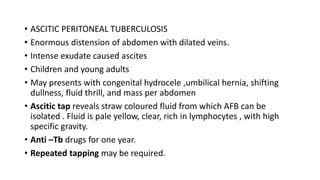
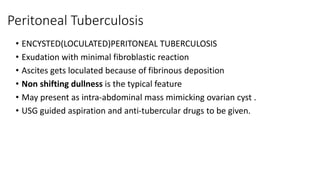
Abdominal tuberculosis is common in India and other developing countries. It can affect the intestines, peritoneum, mesentery and lymph nodes. Symptoms include abdominal pain, diarrhea, weight loss and fever. Diagnosis involves imaging tests like ultrasound and CT scan as well as biopsy of affected tissues. Treatment consists of a combination of anti-tuberculosis drugs for at least 6-12 months as well as possible surgery for complications like obstruction or abscess. Regular follow up is needed to monitor response to treatment.