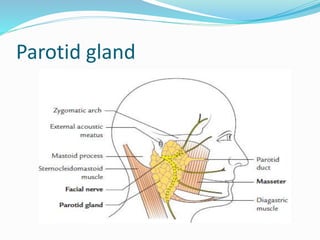
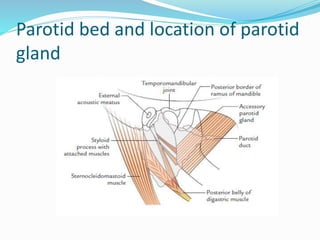
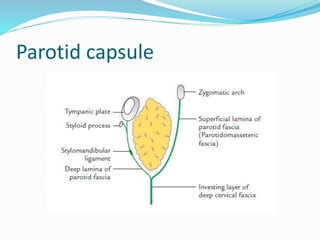
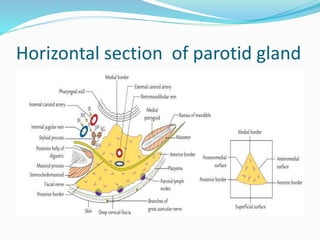
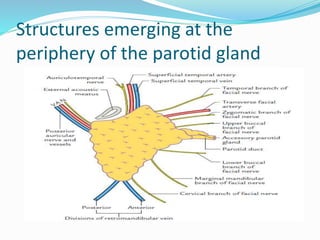
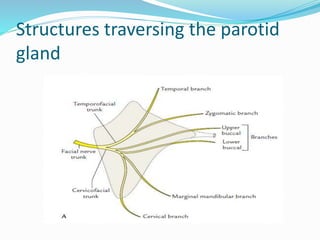
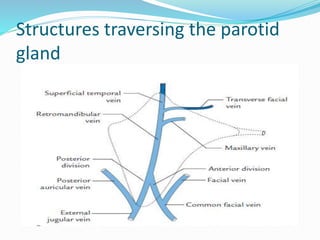
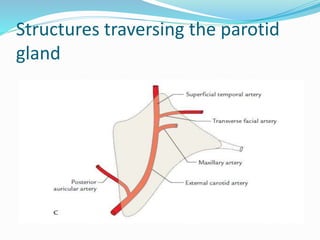
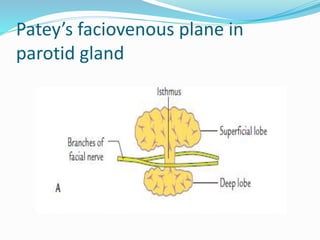
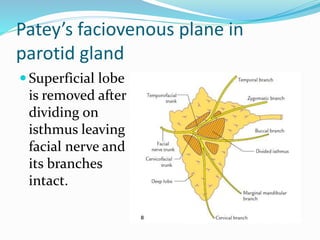
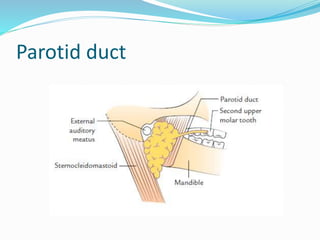
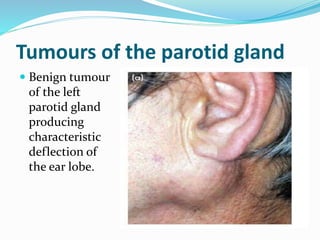
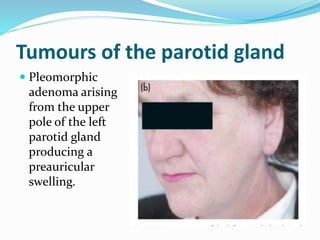
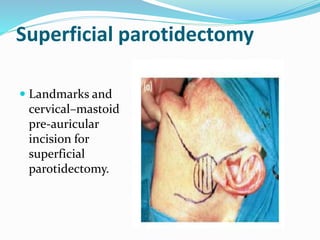
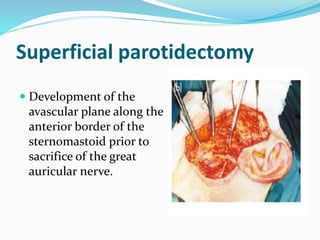
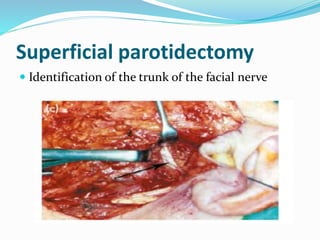
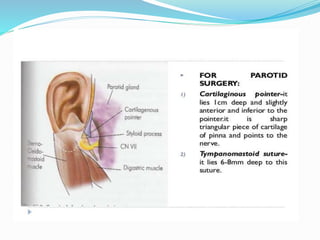
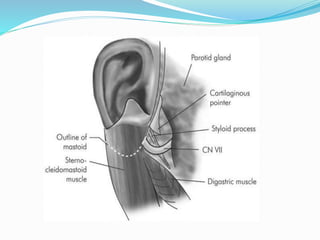
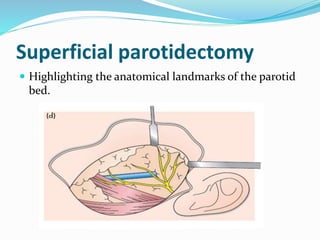
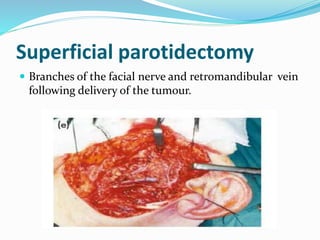
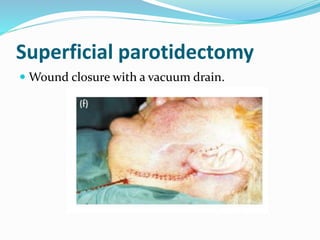
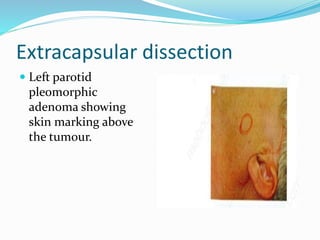
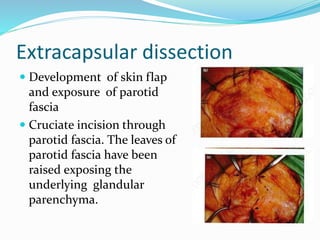
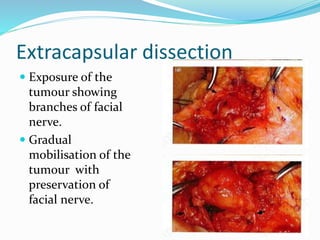
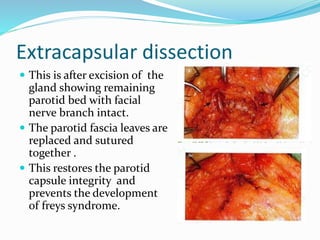
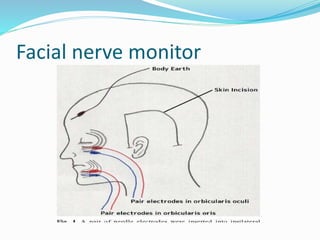
The document discusses the parotid gland, including its location, structures, and tumors. It describes the parotid gland's location in front of and below the ear. It notes that the superficial lobe is the most common site for salivary gland tumors, which usually present as slow-growing, painless swellings. The document outlines surgical procedures for parotid tumors, including superficial parotidectomy and extracapsular dissection. It discusses complications like facial nerve weakness and Frey's syndrome.