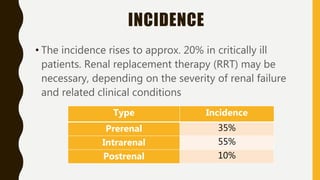
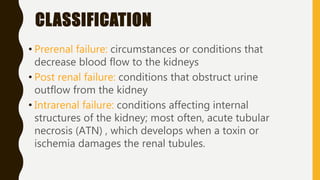
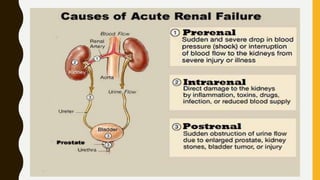
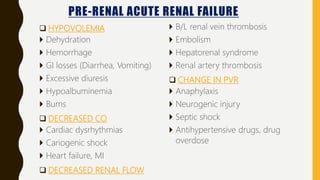
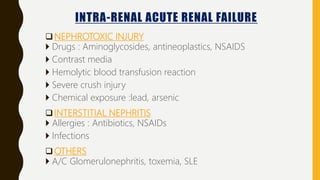
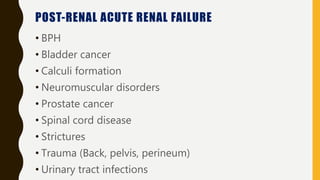
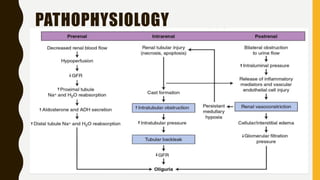
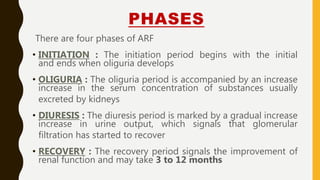
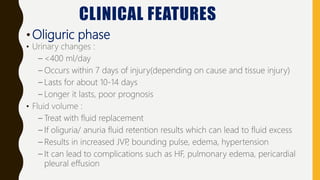
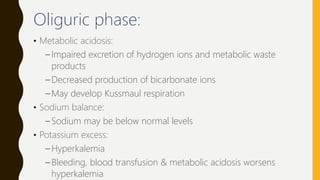
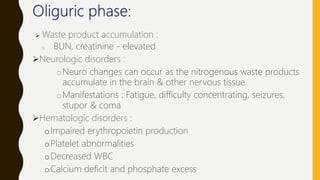
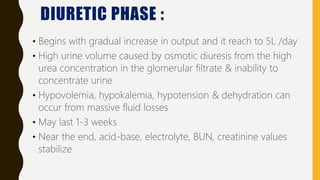
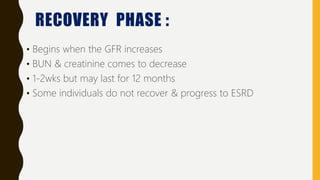
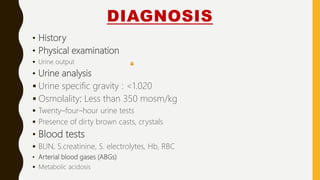
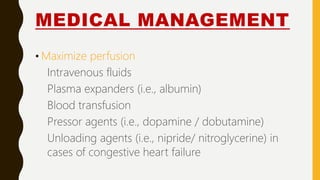
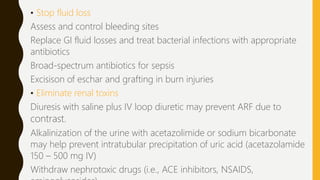
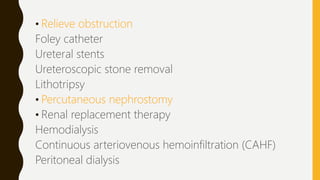
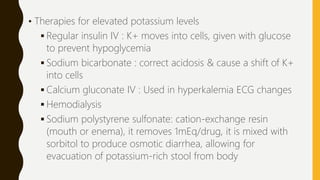
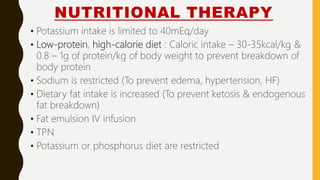
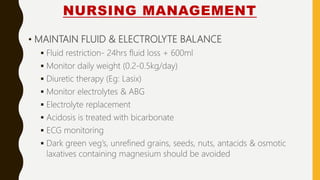
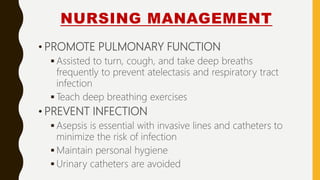
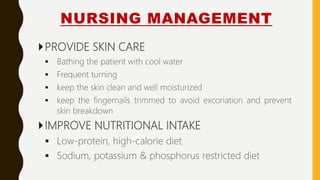
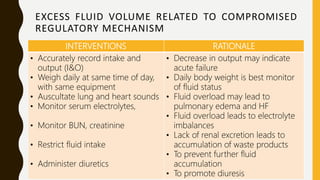
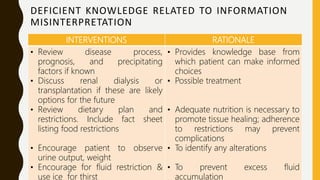
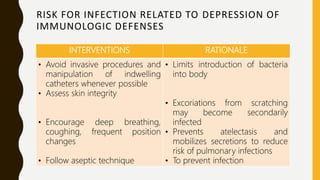
Acute renal failure is a sudden decline in kidney function that results in the buildup of waste products in the blood. It can be caused by decreased blood flow to the kidneys, obstruction of urine outflow, or direct damage to the kidneys. Symptoms include decreased urine output, fluid retention, electrolyte imbalances, and accumulation of waste products. Treatment focuses on restoring fluid and electrolyte balance, preventing complications, and addressing the underlying cause of kidney injury through medical management or renal replacement therapy if needed. Nursing care is aimed at monitoring fluid status, preventing infections, improving nutrition, and managing complications of acute renal failure.