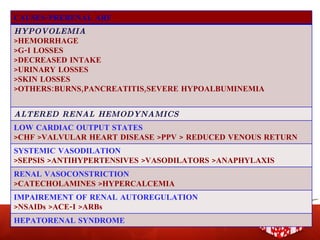
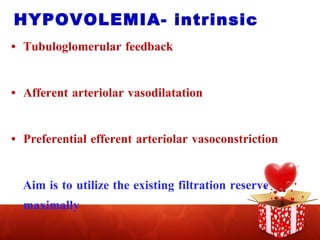
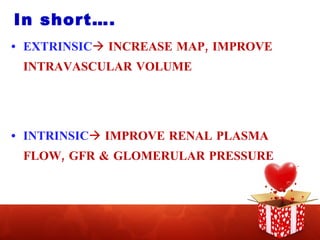
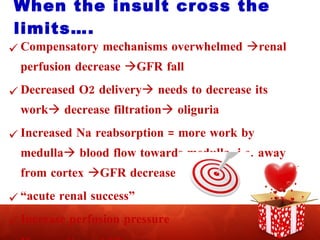
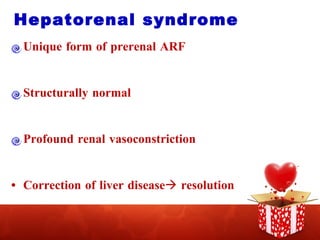
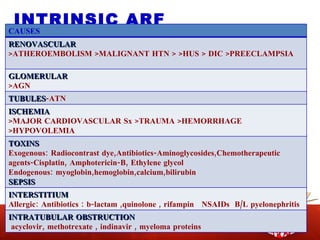
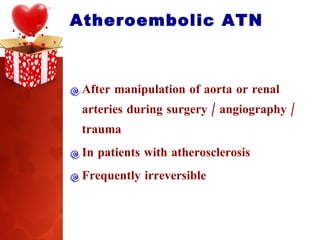
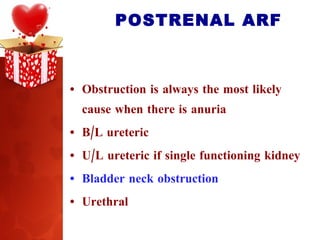
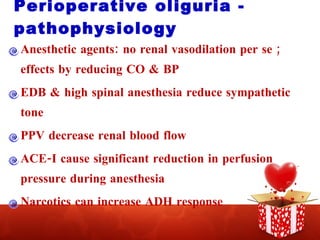
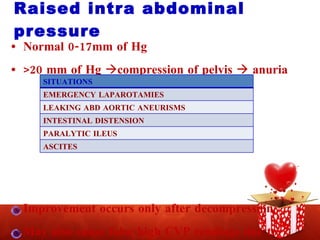
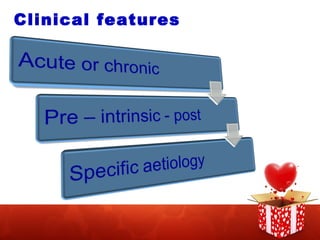
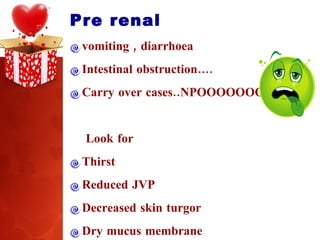
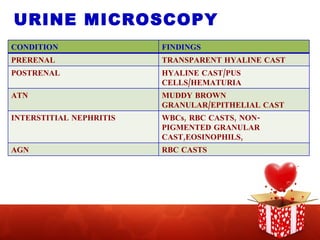
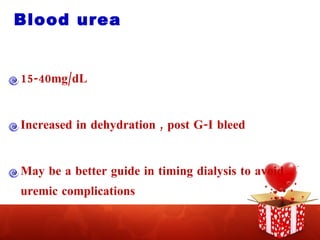
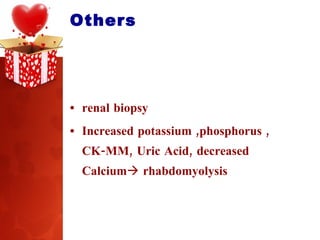
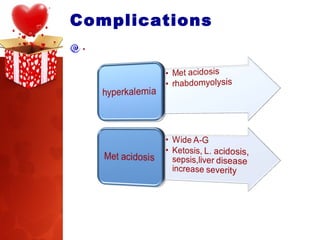
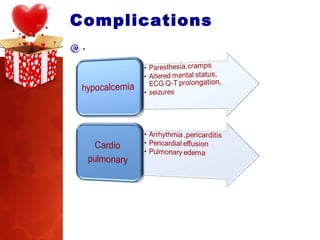
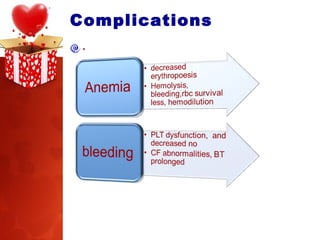
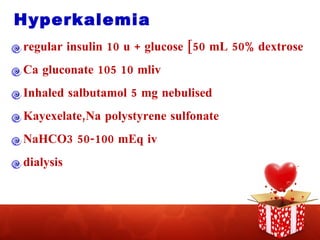
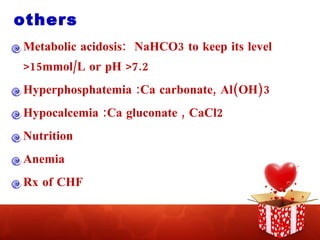
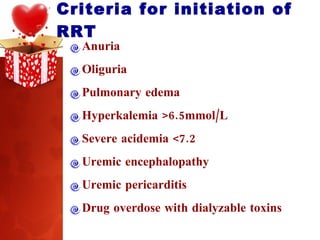
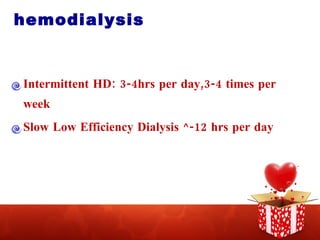
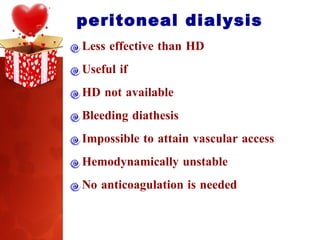
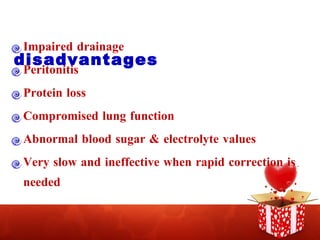
This document summarizes the pathogenesis and management of acute renal failure. It discusses the causes and stages of pre-renal, intrinsic renal, and post-renal acute kidney injury. Key factors in preventing acute renal failure in surgical patients include adequate hydration, maintaining renal perfusion pressure, avoiding nephrotoxins, and aggressive treatment of complications such as hyperkalemia. Treatment may involve renal replacement therapies like hemodialysis when criteria for initiation are met.
![Highlights… FOLLOWING THE TRENDS…. CAPTURE THE KEYS TO OPEN THE DOOR HOW TO PREVENT ARF [Anesthetist Rested during Failure] NEVER ENDING CONTRAVERSIES REPLACING KIDNEY […very difficult]](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-3-320.jpg)
![‘ ACUTE KIDNEY INJURY’ Abrupt reduction [<48 hrs] in kidney function, defined as an absolute increase in S creatinine of ≥0.3 mg/dL A percentage increase in S creatinine of ≥ 50% [1.5 fold from baseline] or a reduction in urine output-- documented oliguria of < 0.5 ml/kg/hr, for more than six hours.](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-4-320.jpg)
![STAGING SYSTEM FOR A.K.I. STAGE S.CREATININE CRITERIA URINE OUTPUT CRITERIA 1 INCREASE IN S.CREATININE ≥0.3mg/dL OR INCREASE TO ≥ 150-200% FROM BASELINE <0.5 ml/kg/hr FOR >6HRS 2 INCREASE IN S.CREATININE TO >200-300%[2-3 FOLD] FROM BASELINE <0.5 ml/kg/hr FOR >12 HRS 3 INCREASE IN S. CREATININE TO >300%[>3 FOLD] FROM BASELINE OR S.CREATININE OF ≥4mg/dL WITH AN ACUTE INCREASE OF ATLEAST 0.5 mg/dL <0.3ml/kg/hr FOR 24 HRS OR ANURIA FOR 12 HRS](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-5-320.jpg)


![Contrast nephropathy FEATURES REVERSIBLE ACUTE ONSET [24-48 HRS] PEAK 3-5 DAYS RESOLUTION IN ONE WEEK B UREA & S CREATININE INCREASE](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-21-320.jpg)




![Creatinine clearance Volume of plasma cleared off creatinine per unit time Earlier warnings, 2hr samples [140-age] x body wt / S.Creatinine x 72 91-130 ml / min CrCl = U. Creatinine [mg/dL] x volume [mL/min] P Creatinine[mg/dL] S cystatin C](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-35-320.jpg)

![Adequate pre-intra & post op hydration Large bore cannula Calculate for deficit correction ,maintenance,3 rd space losses Fluid challenge:250-500mL of NS over 10-15 mins If CVP monitoring established: small elevation[1-2mm]= need more large increase[5mm] = be slow Colloid Controversies over use in sepsis](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-46-320.jpg)



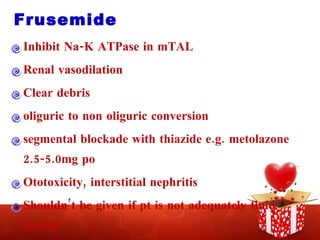
![Frusemide Pigment nephropathy[ 2-3 times the normal dose with aggressive hydration] Contrast nephropathy [with saline] May reverse medullary hypoxia induced by toxins 2-10 mg/kg for converting oliguric to non oliguric renal failure Continuous infusion 1-10mg/hr after a LD of 10-20mg](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-56-320.jpg)

![ALSO NOTE… FORCED ALKALINE DIURESIS IN RHABDOMYOLYSIS N-ACETYL CYSTINE IN ACETAMINOPHEN INDUCED INJURY CONTRAST NEPHROPATHY hydration , n-acetyl cystiene , theophylline/aminophyllin, bicarbonate containing IVFs[rather than saline]](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-59-320.jpg)







![Peritoneal dialysis Access via a peritoneal catheter 1.5-3L of a dextrose containing solution infused Allowed to dwell for a short period of time[2-4hrs] Convective + diffusive clearance](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-77-320.jpg)
![. “ Recent evidence suggest that more intensive hemodialysis [e.g. daily rather than alternative day intermittent dialysis] may be clinically superior and confers improved survival in ARF , once dialysis is required.”](https://image.slidesharecdn.com/aetiopathogenesismanagementofacuterenalfailure1-091017052703-phpapp02/85/ACUTE-RENAL-FAILURE-78-320.jpg)