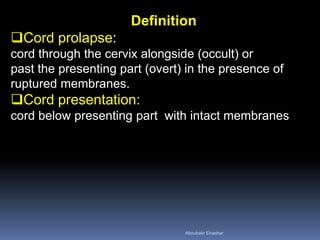
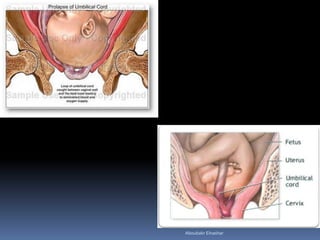
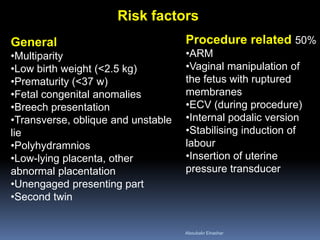
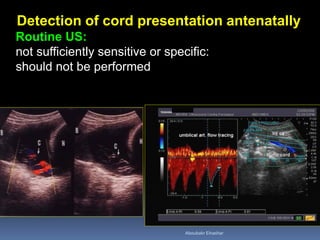
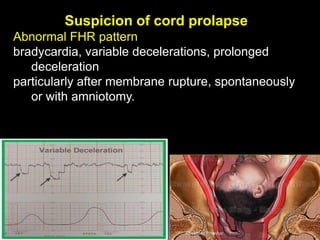
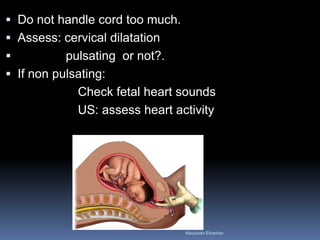
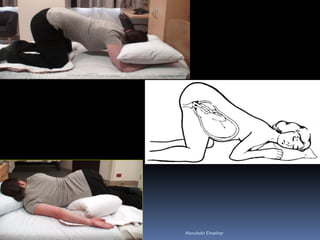
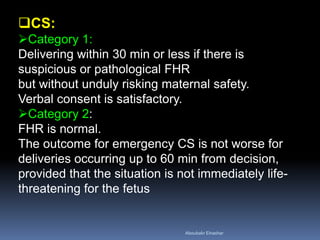
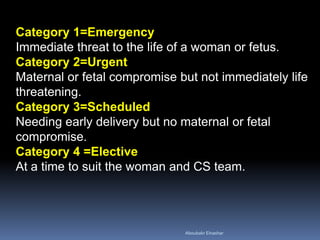
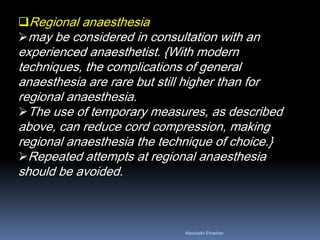
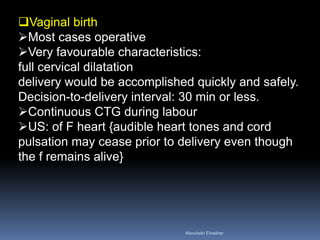
Umbilical cord prolapse occurs when the umbilical cord delivers before or alongside the fetus. It has an incidence of 0.1-0.6% and can lead to perinatal mortality in 91 per 1000 cases due to asphyxia from cord compression. Risk factors include multiparity, prematurity, and breech presentation. Management involves preventing cord compression through elevating the presenting part, filling the bladder, or tocolysis. Delivery is typically by emergency caesarean section if not imminent vaginally. Vaginal delivery may be attempted if full dilation and can be accomplished quickly. Neonatal outcomes are improved by measures to prevent cord compression and asphyxia.