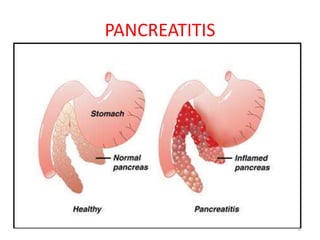
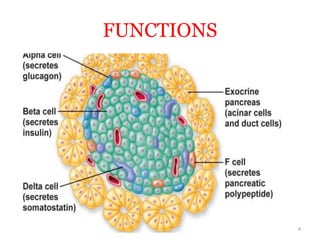
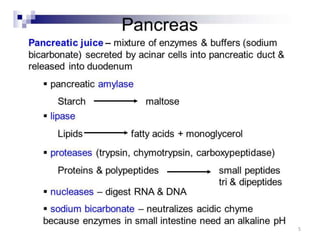
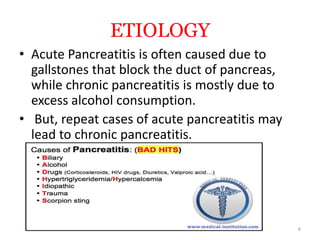
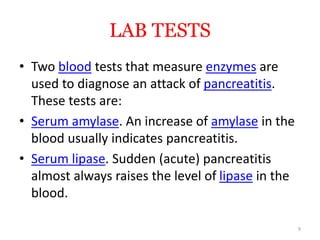
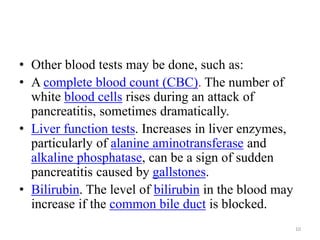
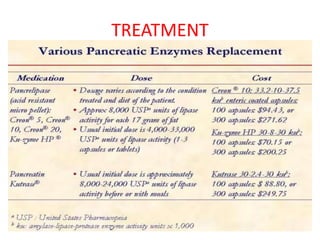
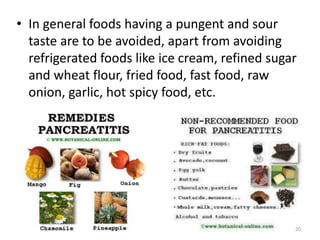
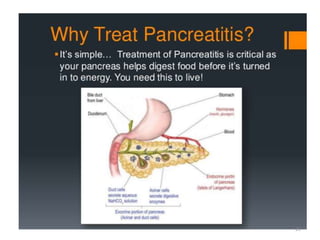
Pancreatitis is an inflammation of the pancreas that can be acute or chronic. Acute pancreatitis is often caused by gallstones blocking the pancreatic duct or heavy alcohol use, while chronic pancreatitis results from repeated acute attacks or long-term alcohol abuse. Symptoms include abdominal pain radiating to the back, tender swollen abdomen, fever, nausea, and increased heart rate. Blood tests measuring amylase and lipase levels indicate pancreatitis. Treatment focuses on pain management, intravenous fluids, dietary changes like a low-fat diet, and potentially surgery to drain fluid or remove diseased tissue. Maintaining a healthy diet and lifestyle through modifications can help manage and prevent pancreatitis.