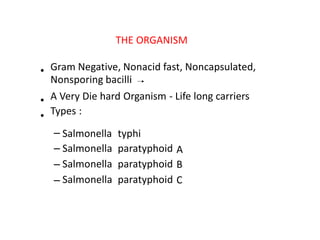
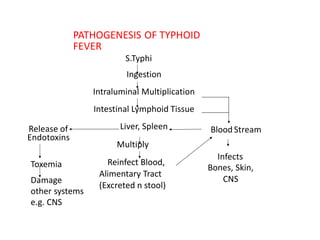
1) Enterific fever is caused by infection of the intestine and gallbladder tissues, most commonly by Salmonella typhi bacteria which causes typhoid.
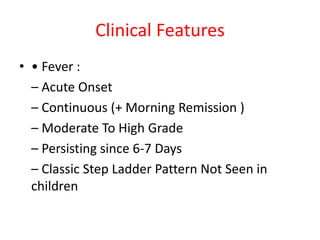
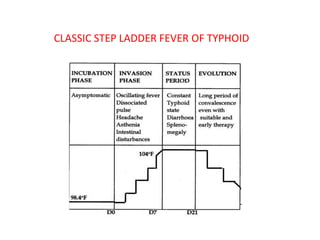
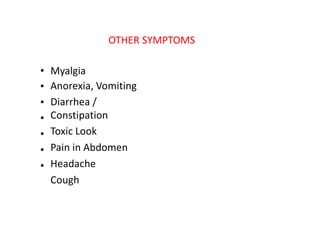
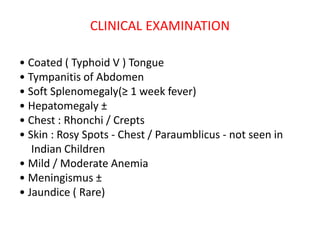
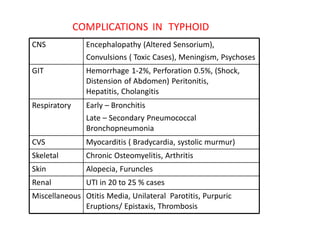
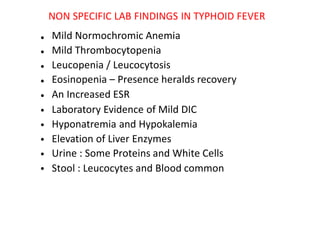
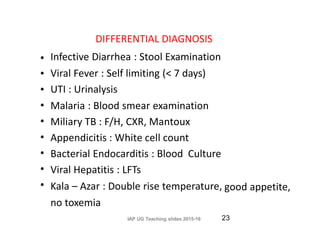
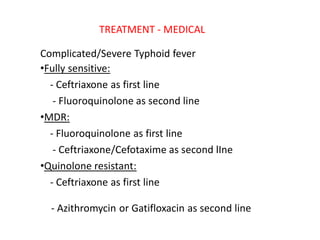
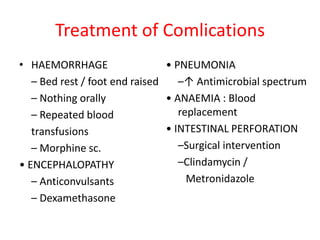
2) Symptoms include sustained high fever, abdominal pain, headache, and toxic appearance. Complications can involve multiple organ systems.
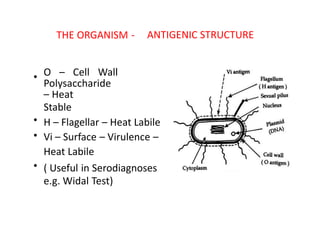
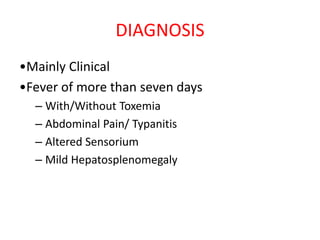
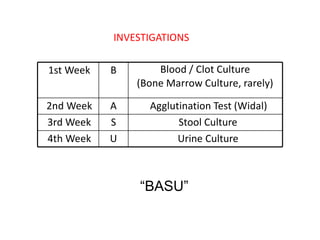
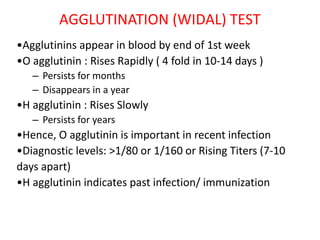
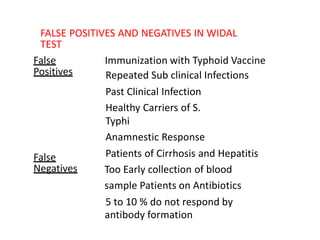
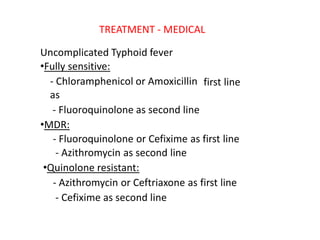
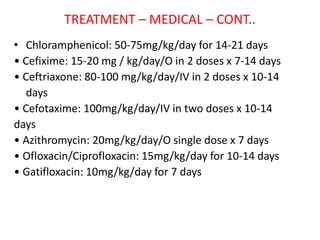
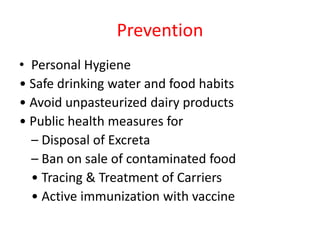
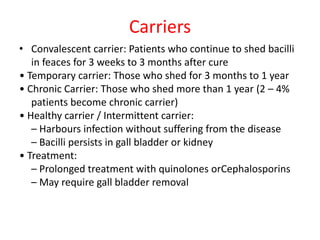
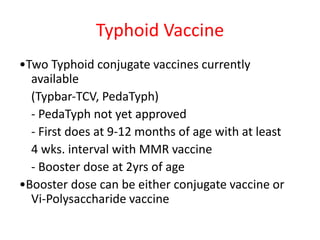
3) Diagnosis is usually clinical but may include blood cultures early and serological tests later. Treatment involves antibiotics like fluoroquinolones. Prevention focuses on hygiene, sanitation and vaccination.