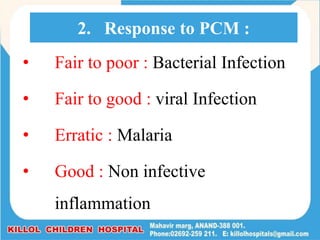
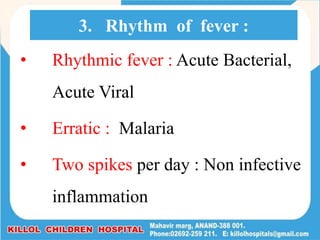
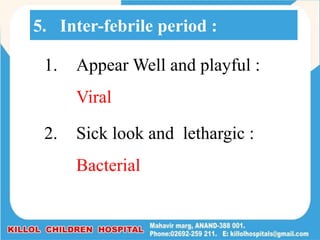
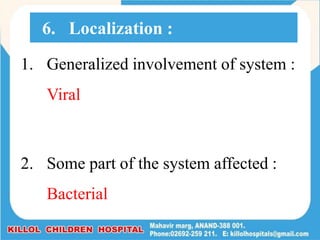
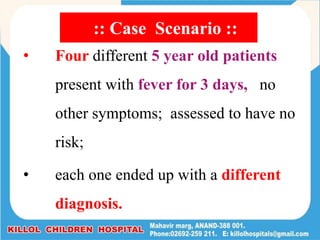
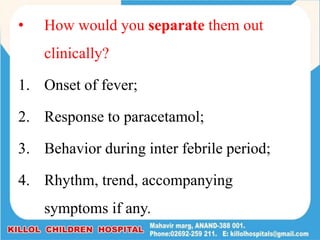
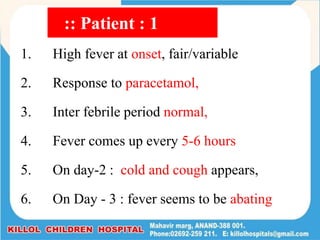
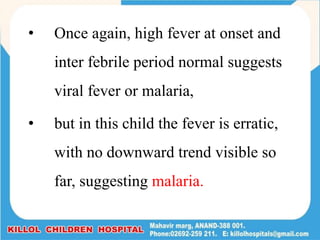
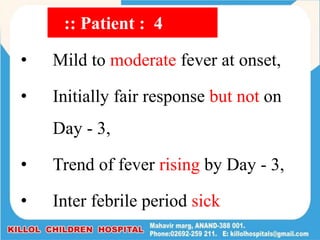
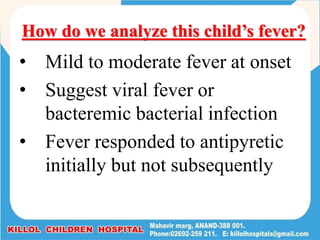
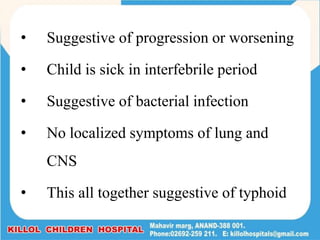
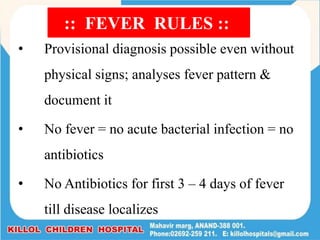
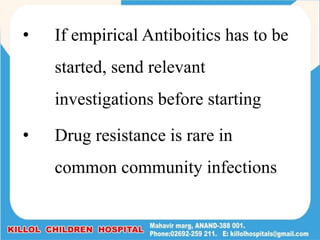
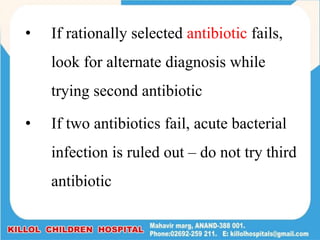
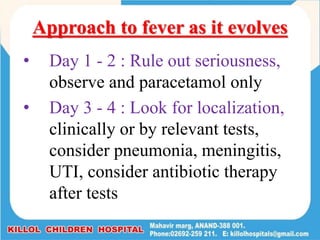
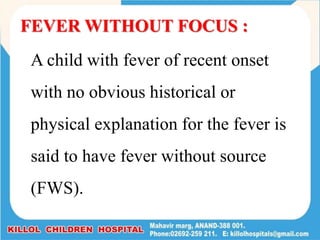
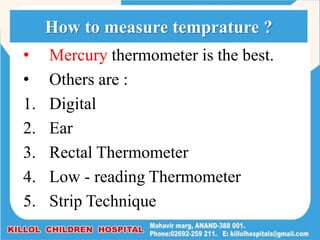
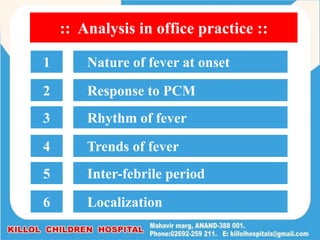
Dr. Rashmin Cecil provides an in-depth approach to pediatric patients presenting with fever, defining fever and discussing its classifications and measurement methods. The document emphasizes the importance of evaluating fever patterns, responses to medications, and inter-febrile behavior to diagnose underlying causes effectively. It highlights the clinical challenges faced by practitioners in managing fever, while stressing the need for careful observation and rational use of antibiotics.

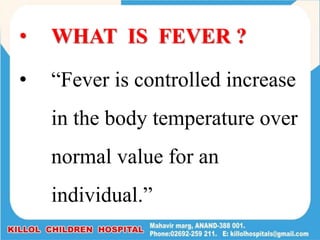
![• Range of normal body temperature:
(36 - 38º C) or (97 - 99 º F)
• PUO : [Pyrexia Unknown Origin]
• Children with a fever documented by
healthcare provider & for which cause could
not be identified after 3 weeks of evaluation
in O.P.D or in hospital admitted cases after
1 week of evaluation are known as PUO.](https://image.slidesharecdn.com/fever17-210624034912/85/Fever-Approach-to-Paediatric-Patient-5-320.jpg)
![STAGES OF FEVER
• [1] The PRODROMAL Stage : (may be Absent)
• [2] The Stage of ONSET or INVASION : (Initial
or pyrogenetic phase)
• [3] The Stage of Fever DEVELOPMENT :
(Fastigium)
• [4] The Stage of DECLINE : ( Defervescence or
Termination)](https://image.slidesharecdn.com/fever17-210624034912/85/Fever-Approach-to-Paediatric-Patient-12-320.jpg)


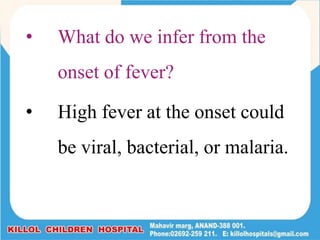
![• [1] High fever :
• Viral Fever
• Bacterial infection
• Acute tonsillitis, Acute Bacillary Dysentery,
UTI
• Malaria
• [2] Moderate Fever :
• Pneumonia, Meningitis, Typhoid
1. Nauure of fever at onset :](https://image.slidesharecdn.com/fever17-210624034912/85/Fever-Approach-to-Paediatric-Patient-21-320.jpg)