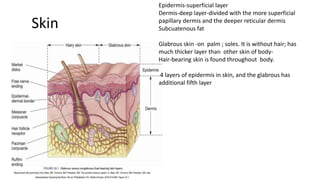
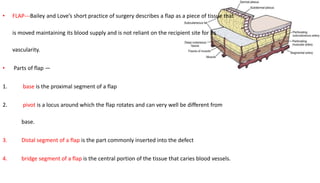
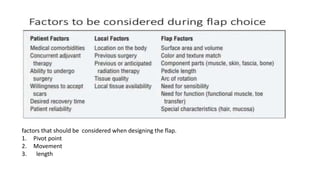
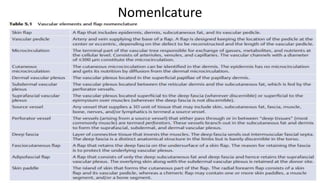
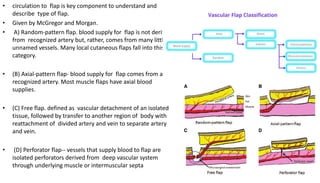
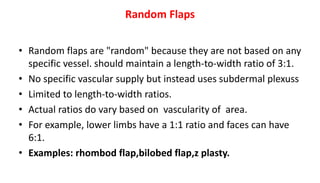
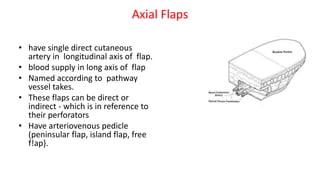
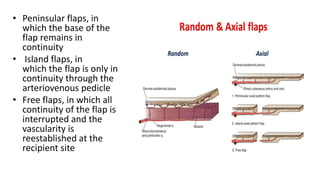
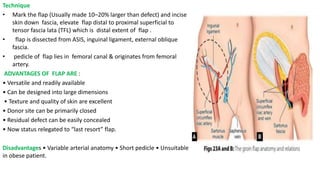
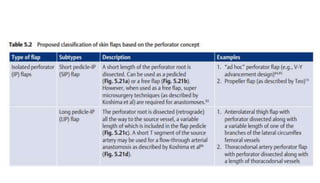
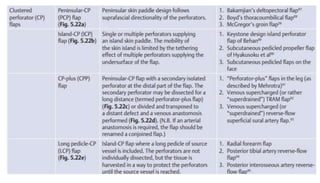
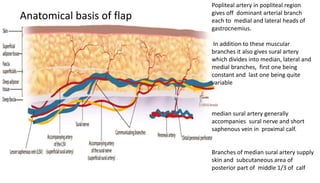
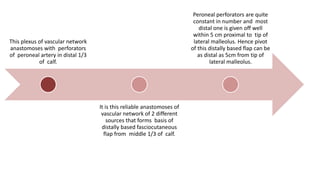
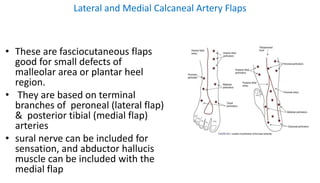
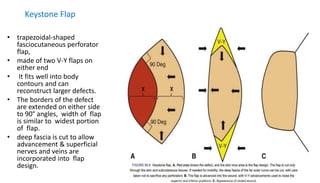
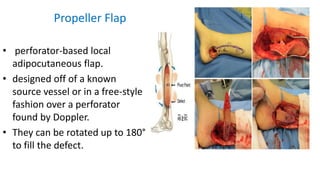
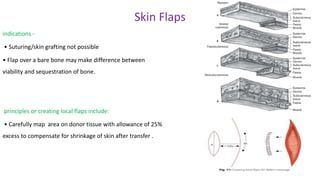
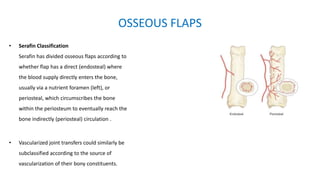
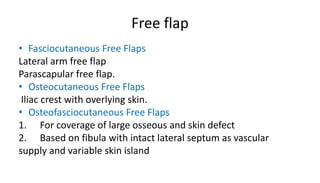
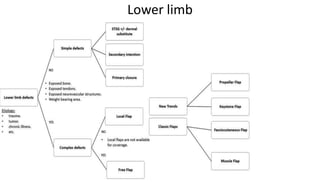
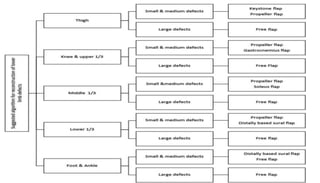
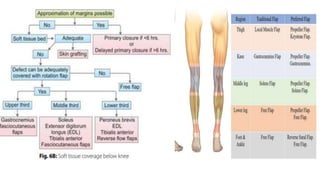
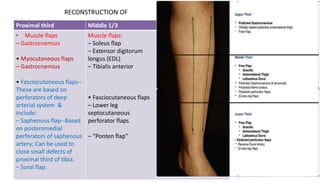
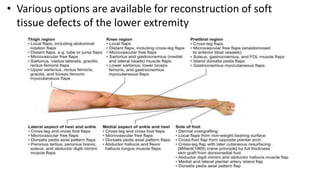
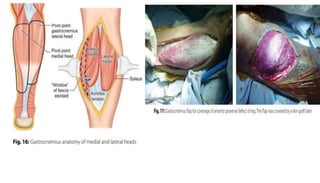
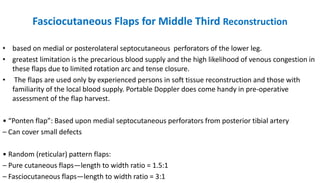
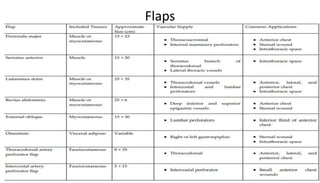
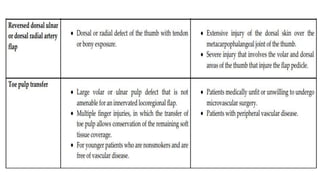
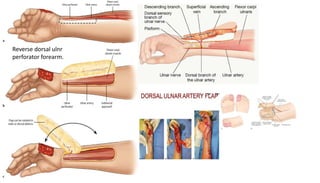
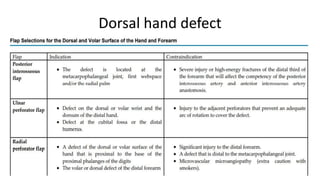
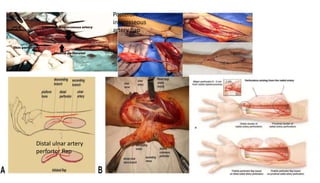
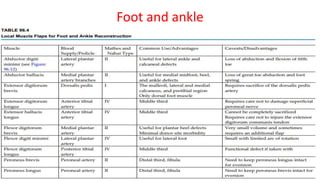
1. The document discusses different types of flaps used in surgery, including their anatomy and uses. Random flaps rely on subdermal plexuses for blood supply and have limited dimensions based on an area's vascularity. Axial flaps are based on a direct artery and can be peninsular, island, or free flaps. Perforator flaps are based on named perforating arteries.
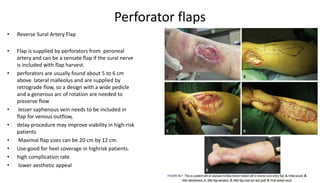
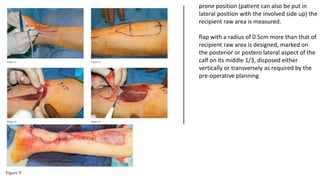
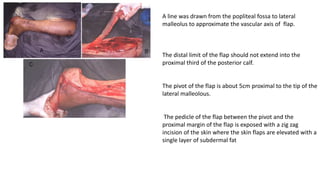
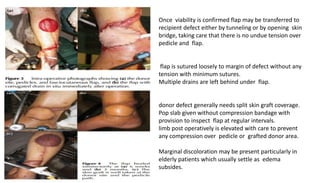
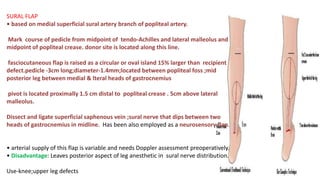
2. The reverse sural artery flap is highlighted, which uses perforators from the peroneal artery to cover defects of the lower leg/foot. It spares the sural nerve to prevent sensory deficits while maintaining blood supply, which comes from the lesser saphenous vein and deep adipose tissue rather