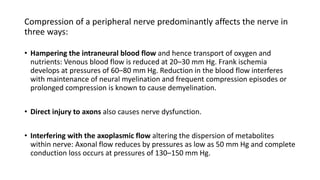
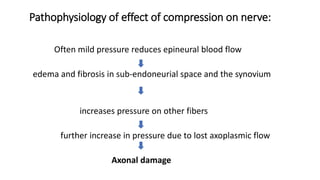
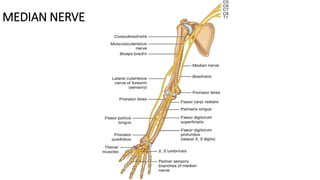
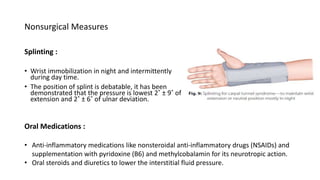
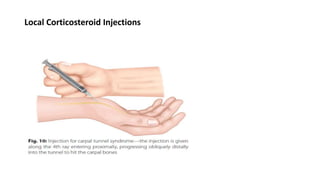
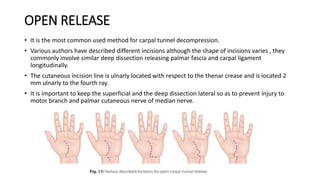
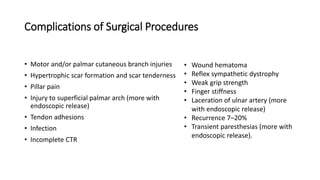
Entrapment Neuropathies document discusses various peripheral nerve entrapment syndromes, focusing on carpal tunnel syndrome and anterior interosseous nerve syndrome. It provides details on the anatomy, pathophysiology, clinical presentation, diagnostic studies including electrodiagnostic testing, differential diagnosis, and treatment options including splinting, injections, and surgical decompression for relieving nerve compression in these conditions. Surgical techniques for carpal tunnel release including open, limited open, and endoscopic methods are outlined, as well as potential complications.
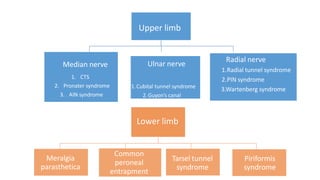



![ULNAR TUNNEL SYNDROME
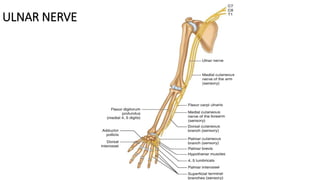
• Direct compression of the ulnar nerve in the Guyon’s canal. It is also known as handlebar
palsy (seen in long distance cyclists who rest their hand on the cycle handle bar).
• The ulnar nerve in forearm lies deep to the FCU. Distally it becomes more superficial as it
crosses the myotendinous junction of FCU. Radially it is accompanied by the ulnar artery and
FCU lies on the ulnar aspect as it progresses further and enters the ulnar canal/tunnel
(Guyon’s canal).
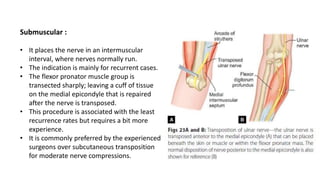
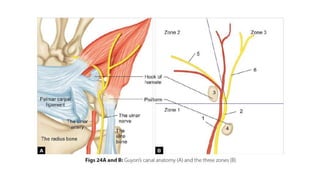
• Guyon’s canal: It is a 4 cm long structure starting at the proximal extent of the volar carpal
ligament and ends at the arch of the hypothenar muscles.
The ulnar canal contains :
• Bifurcation of ulnar nerve: The ulnar nerve divides into the superficial sensory and deep
motor branches (Fig. 25). The deep branch supplies all the interosseous muscles and the
third and fourth lumbricals, the hypothenar muscles and some thenar muscles [the adductor
pollicis and the medial head (deep) of the FPB].
• Ulnar artery.](https://image.slidesharecdn.com/entrapmentneuropathy-220215163450/85/Entrapment-neuropathy-75-320.jpg)

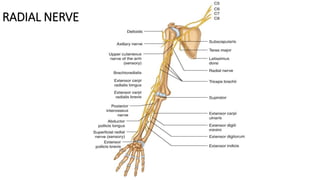
![RADIAL TUNNEL SYNDROME (RTS, SUPINATOR SYNDROME)
• It is a compressive neuropathy of the radial nerve main trunk in the proximal forearm
before/at/just after it splits into main trunk posterior interosseous neuropathy (PIN) and
the minor trunk (sensory branch) which results in refractory lateral elbow and forearm
symptoms (both sensory and motor).
• Compression of only sensory nerve [radial sensory nerve, (RSN)] is called Wartenberg
syndrome, while that of only motor component (PIN only is called PIN compression
palsy) and are distinct entities.
• Radial tunnel syndrome is possibly a misnomer and not a true representative of the
compressive neuropathies for following reasons:
-Prominent focal tenderness
-Normal neurologic function
-No confirmatory electrodiagnostic evidence of nerve dysfunction.](https://image.slidesharecdn.com/entrapmentneuropathy-220215163450/85/Entrapment-neuropathy-83-320.jpg)