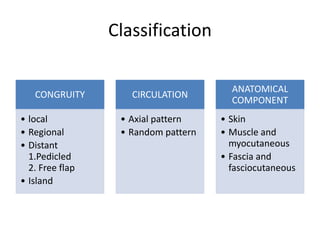
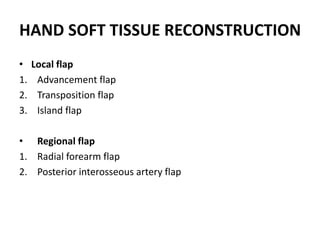
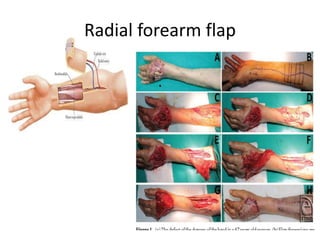
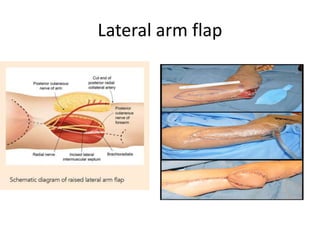
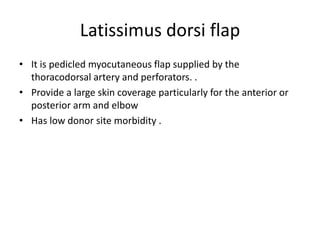
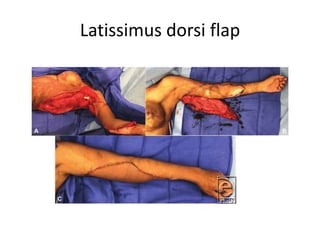
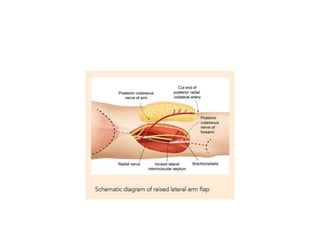
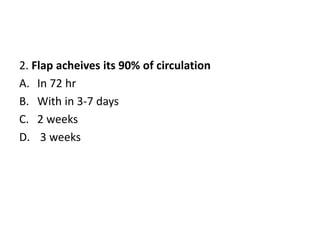
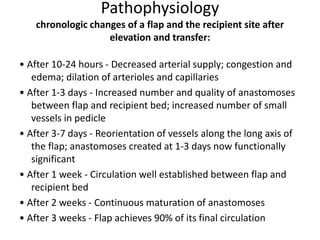
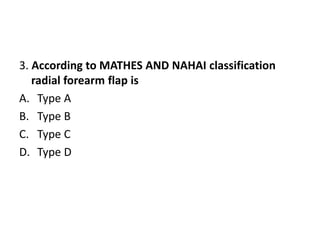
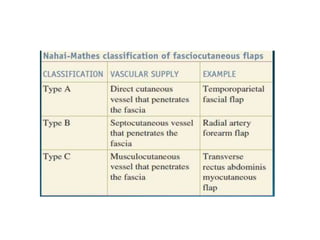
The document discusses flap coverage in upper extremities during trauma, detailing the types of flaps (local, regional, and distant), their classifications, and specific flaps like the radial forearm flap and latissimus dorsi flap for reconstructive surgery. It emphasizes the importance of flap selection based on patient condition, defect size, and surgeon skill, as well as postoperative monitoring to prevent complications. The document also outlines the pathophysiology of flap healing and the criteria for successful flap procedures.