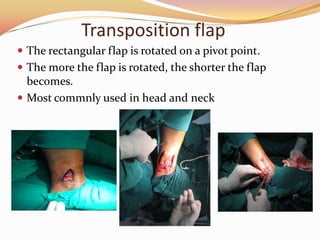
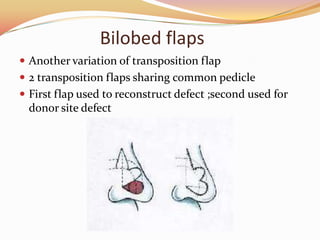
This document discusses different types of flaps used in plastic surgery for tissue reconstruction. It begins by explaining that flaps are vascularized tissue transferred from one part of the body to another to reconstruct areas of tissue loss. The document then categorizes flaps based on their components, configuration, congruity, circulation, and conditioning. It provides examples of various local, regional, pedicled, and free flaps. Key advantages and disadvantages of different flap types are highlighted. Monitoring techniques and potential complications of flap surgery are also summarized.