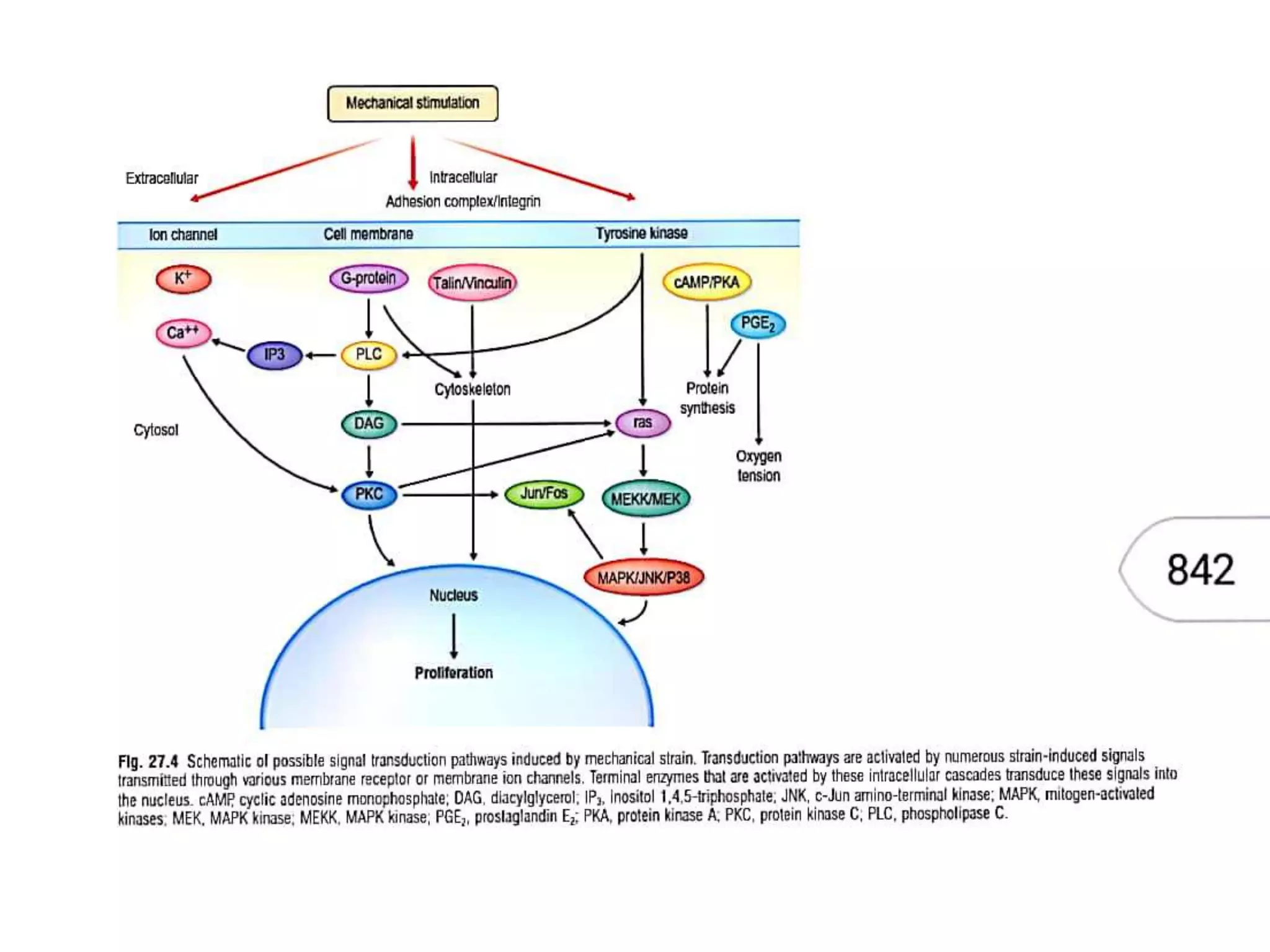
Tissue expansion is a technique used to generate additional soft tissue for reconstruction. It involves surgically placing an implant under the skin that is gradually inflated over time using saline injections, causing the overlying tissue to stretch and grow. The document discusses the history, biology, types of implants, principles and applications of tissue expansion. It can be used to reconstruct defects on the scalp, forehead, face, neck and nose by expanding the surrounding tissue.