Dr. Gavinash Rao presented on the history and techniques of perforator flaps. Key points include:
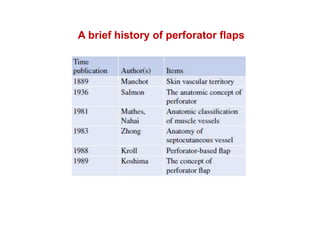
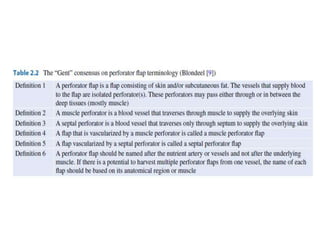
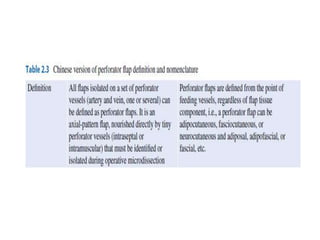
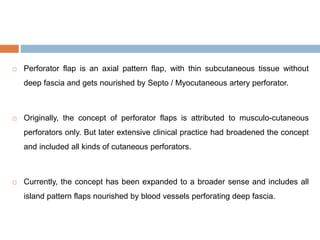
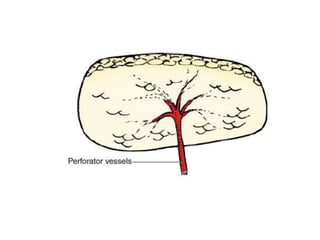
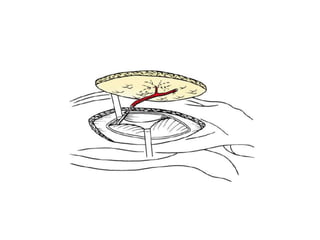
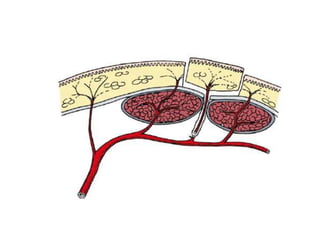
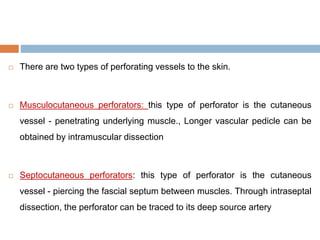
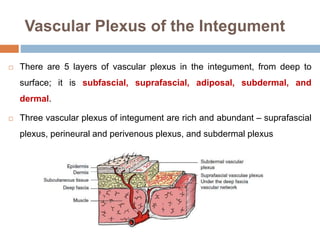
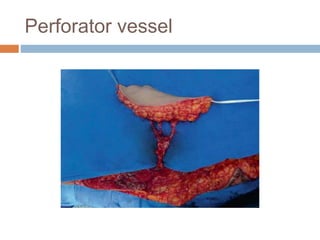
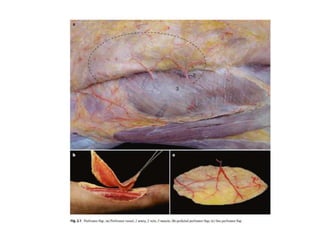
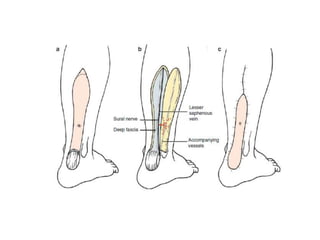
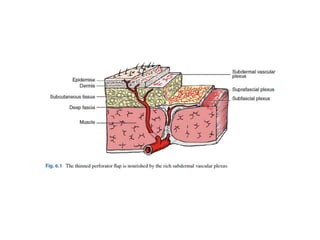
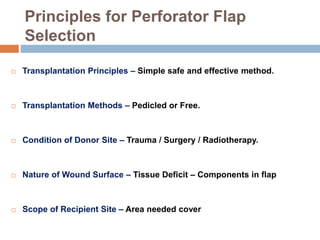
- Perforator flaps rely on perforating vessels that pass through deep fascia to supply skin and soft tissue. They were first described in 1989 and gained popularity after conferences in 2001 and 2005.
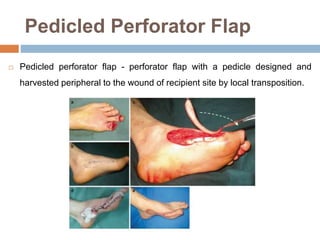
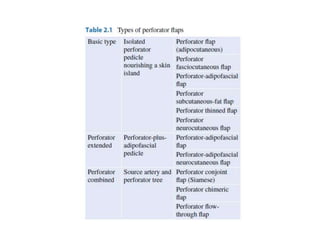
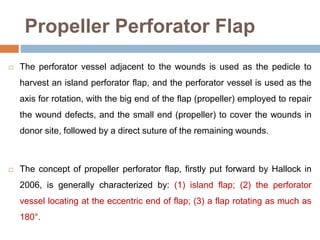
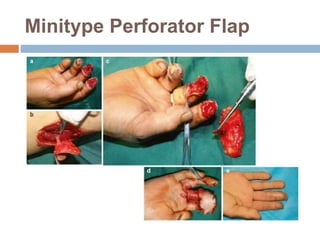
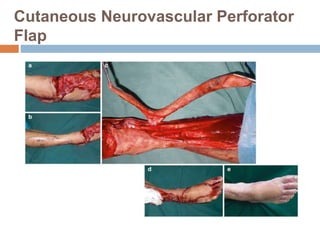
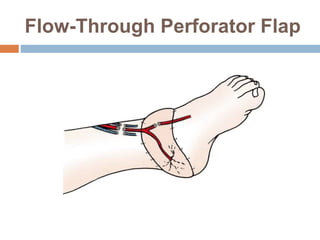
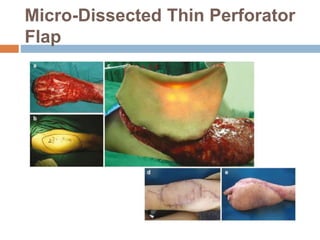
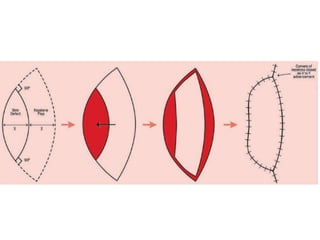
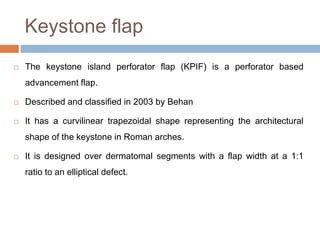
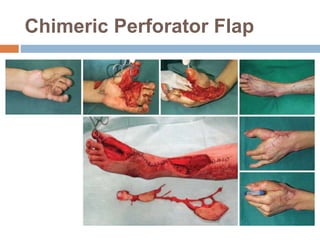
- Advantages over traditional flaps include reduced donor site morbidity and more tailored reconstruction to match defects. Various types of perforator flaps have been developed like propeller flaps.
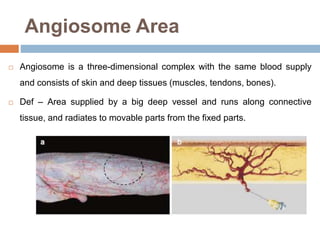
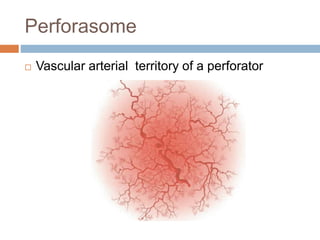
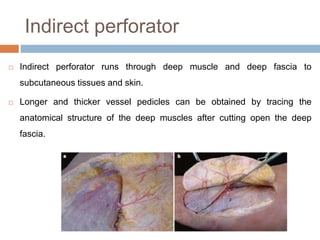
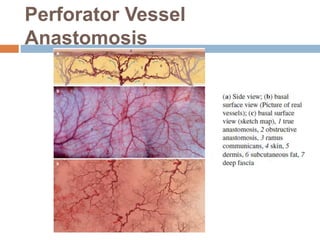
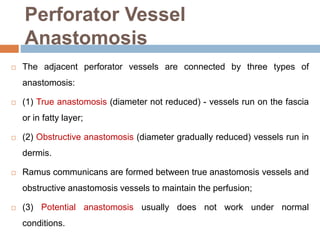
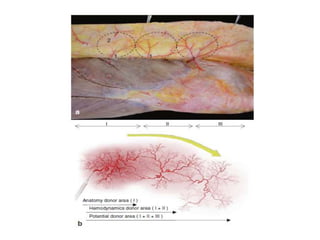
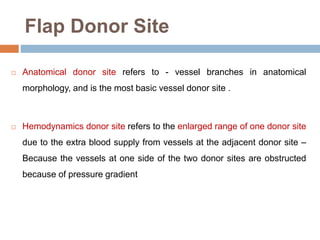
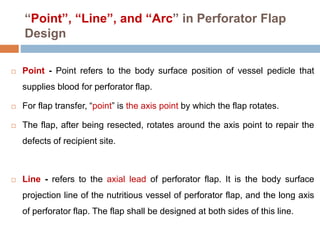
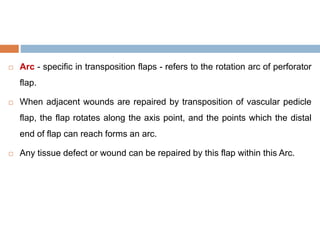
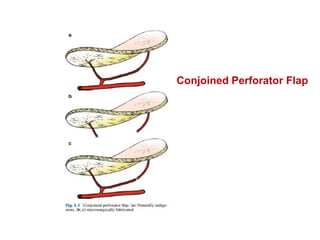
- Angiosomes describe the vascular territories of perforators and helped develop special flap designs. Perforasomes further describe the territory of individual perforators.
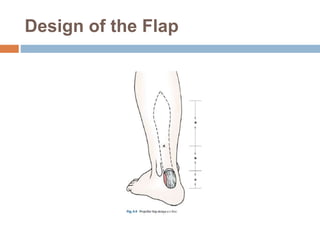
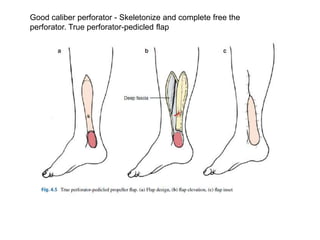
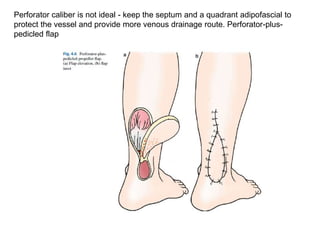
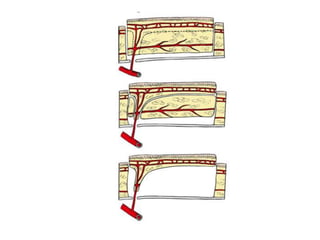
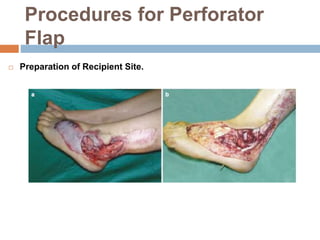
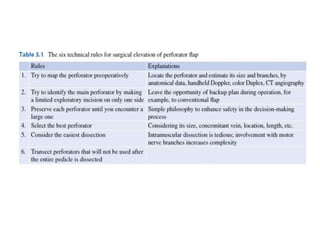
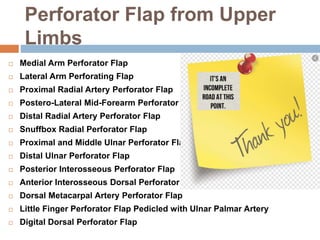
- Techniques include identifying perforators with