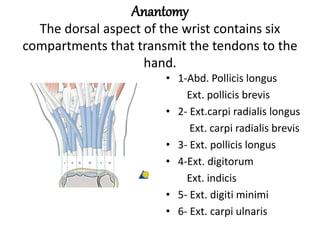
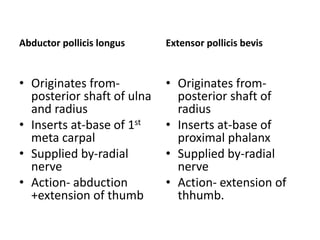
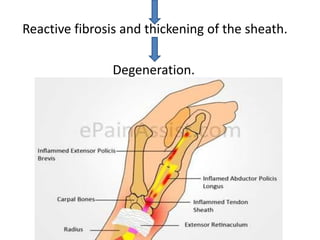
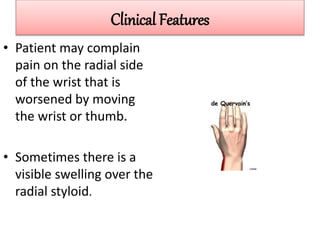
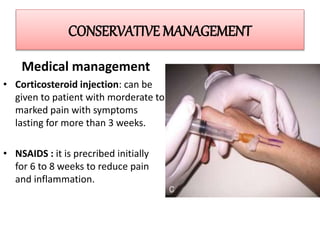
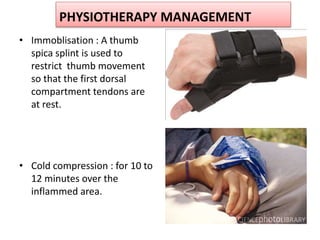
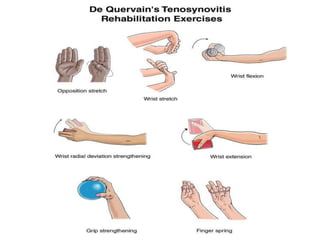
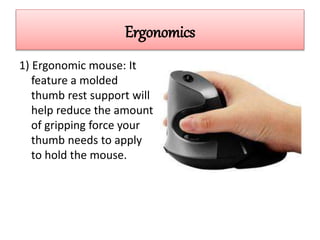
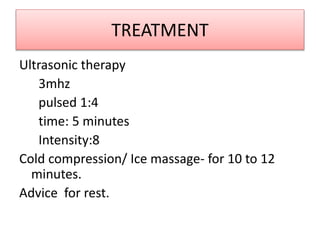
De Quervain's tenosynovitis is an inflammation of the tendon sheaths of the abductor pollicis longus and extensor pollicis brevis muscles in the wrist. It commonly affects women ages 30-50 and is caused by repetitive motions like knitting or computer use that strain the thumb and wrist. Symptoms include pain on the radial side of the wrist worsened by thumb movement. Conservative treatment involves splinting, anti-inflammatories, corticosteroid injections, and physical therapy exercises. Surgery may be considered if symptoms persist after several weeks of conservative care.