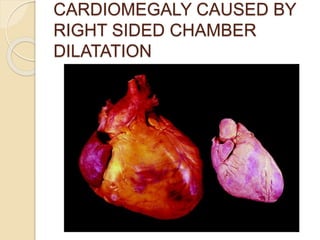
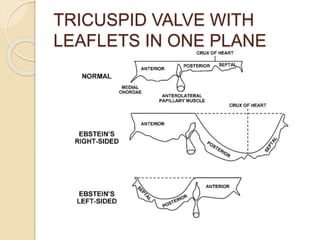
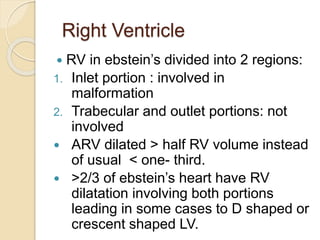
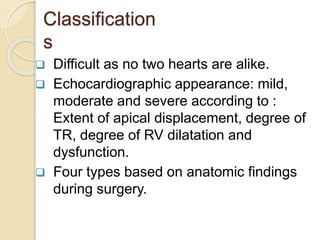
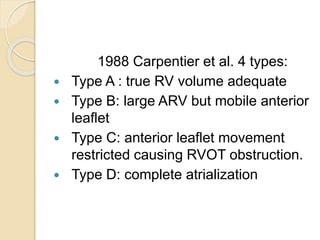
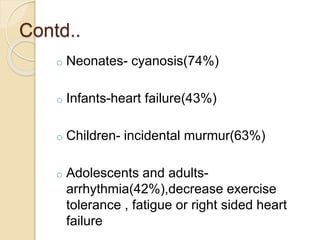
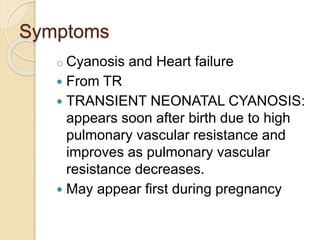
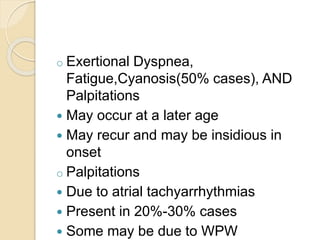
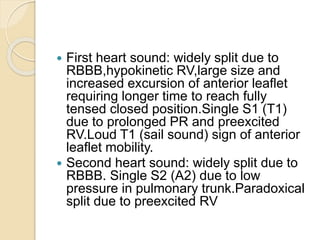
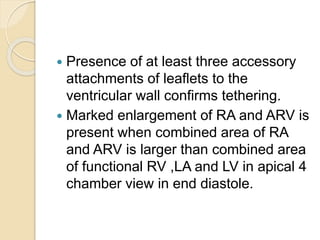
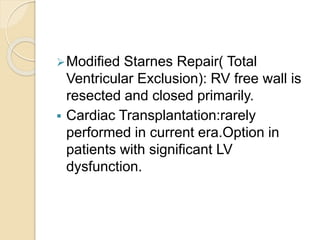
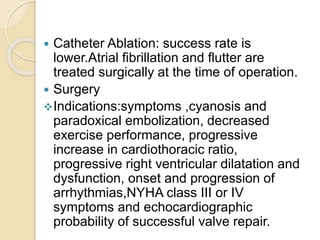
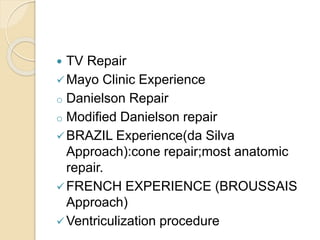
Wilhelm Ebstein first described Ebstein's anomaly in 1866. It is a rare congenital heart defect where the tricuspid valve is displaced downward into the right ventricle. Echocardiography is the primary diagnostic tool and shows apical displacement of the tricuspid valve leaflets. Treatment depends on severity but may include surgical repair of the tricuspid valve or exclusion of the dysfunctional right ventricle. Prognosis varies from critical in severe neonatal cases to relatively mild in some adults.