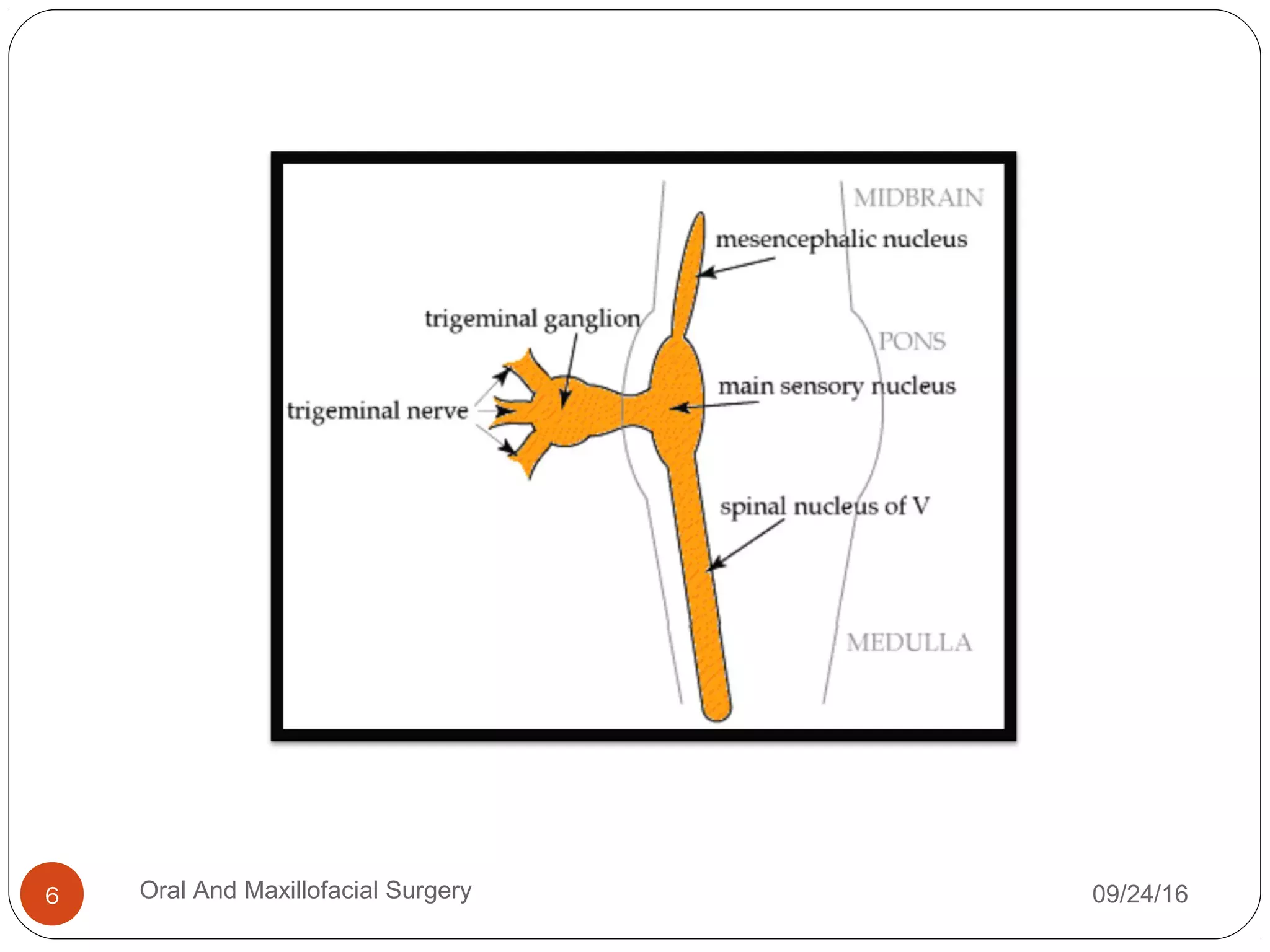
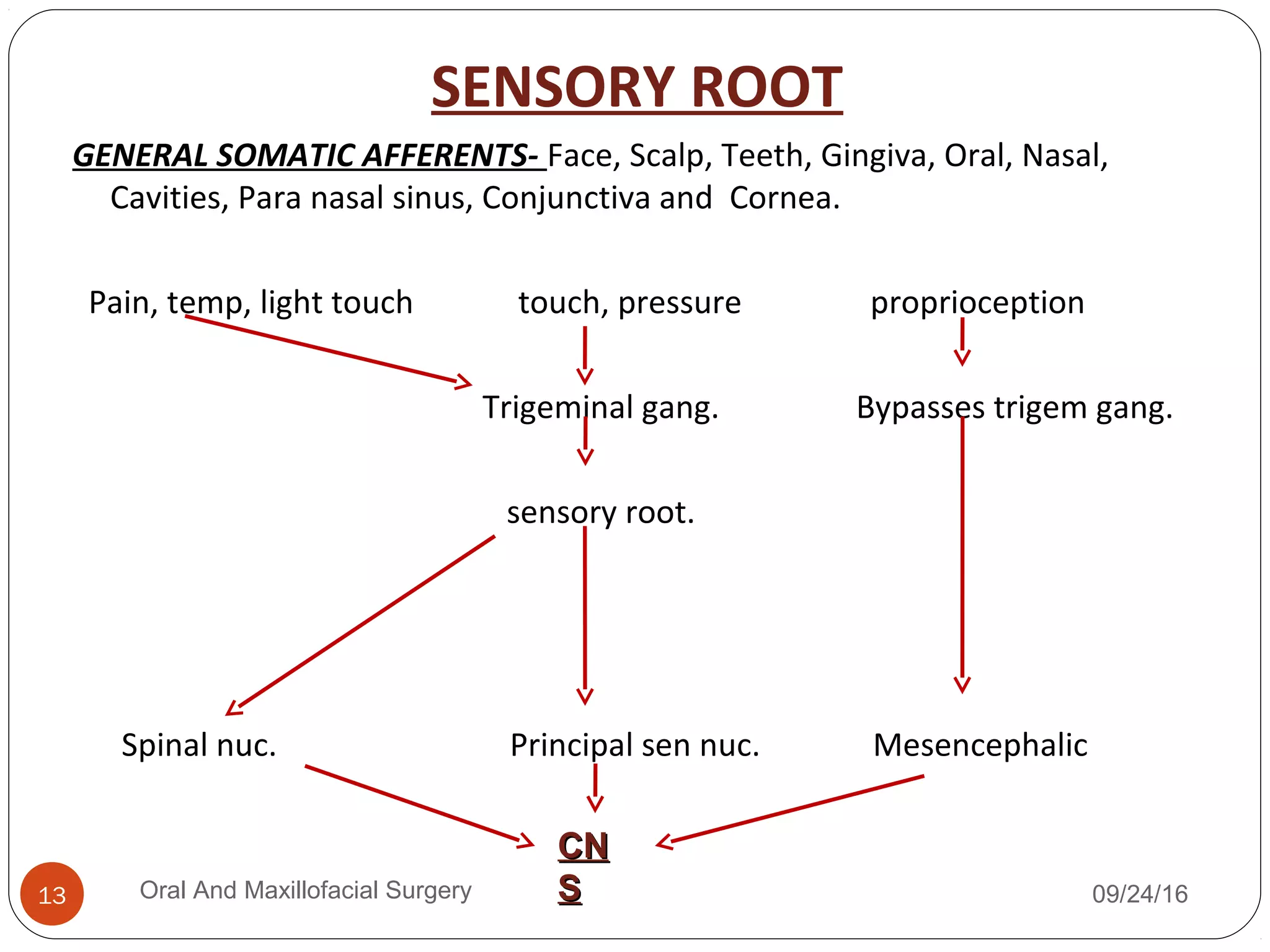
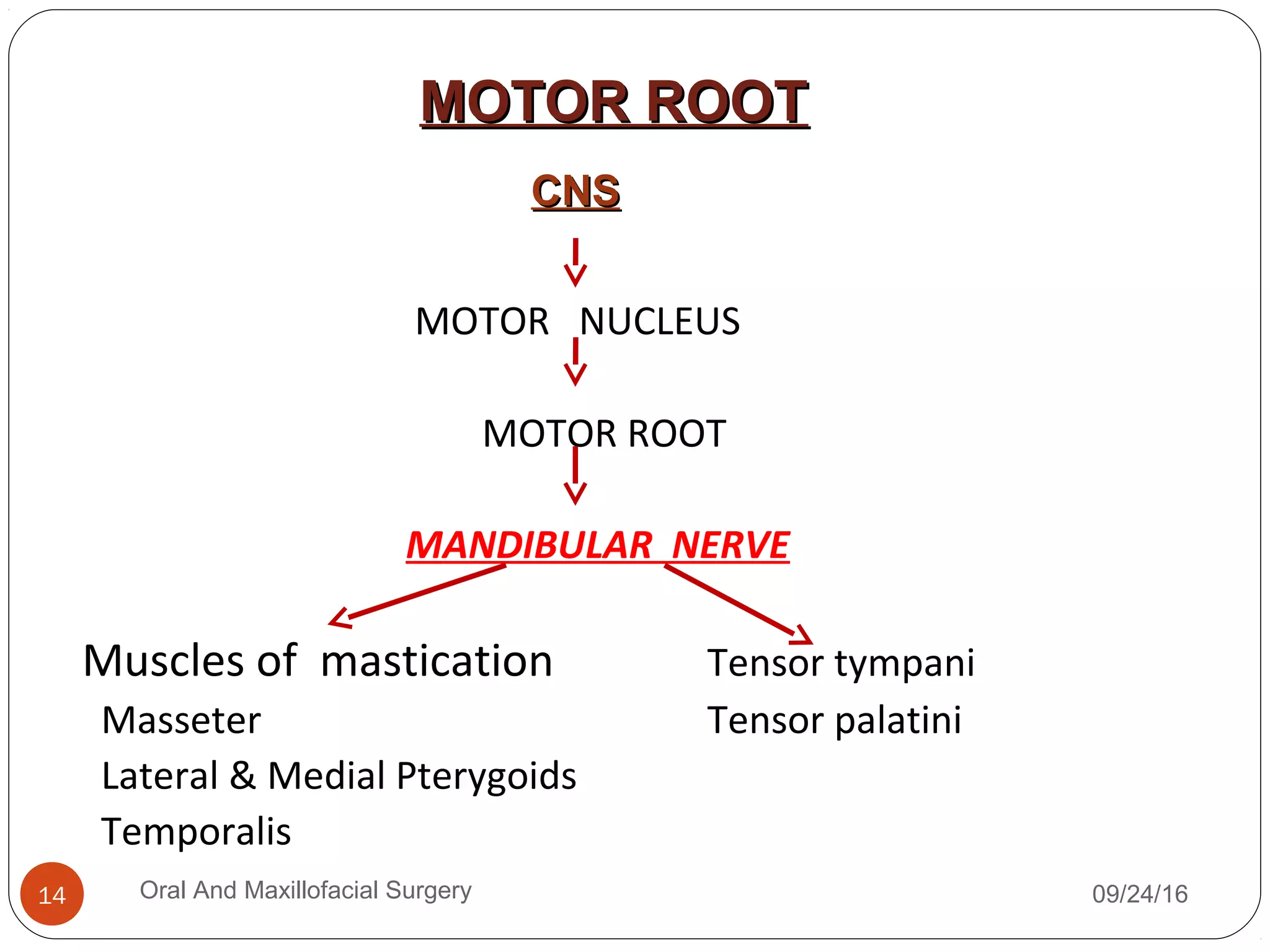
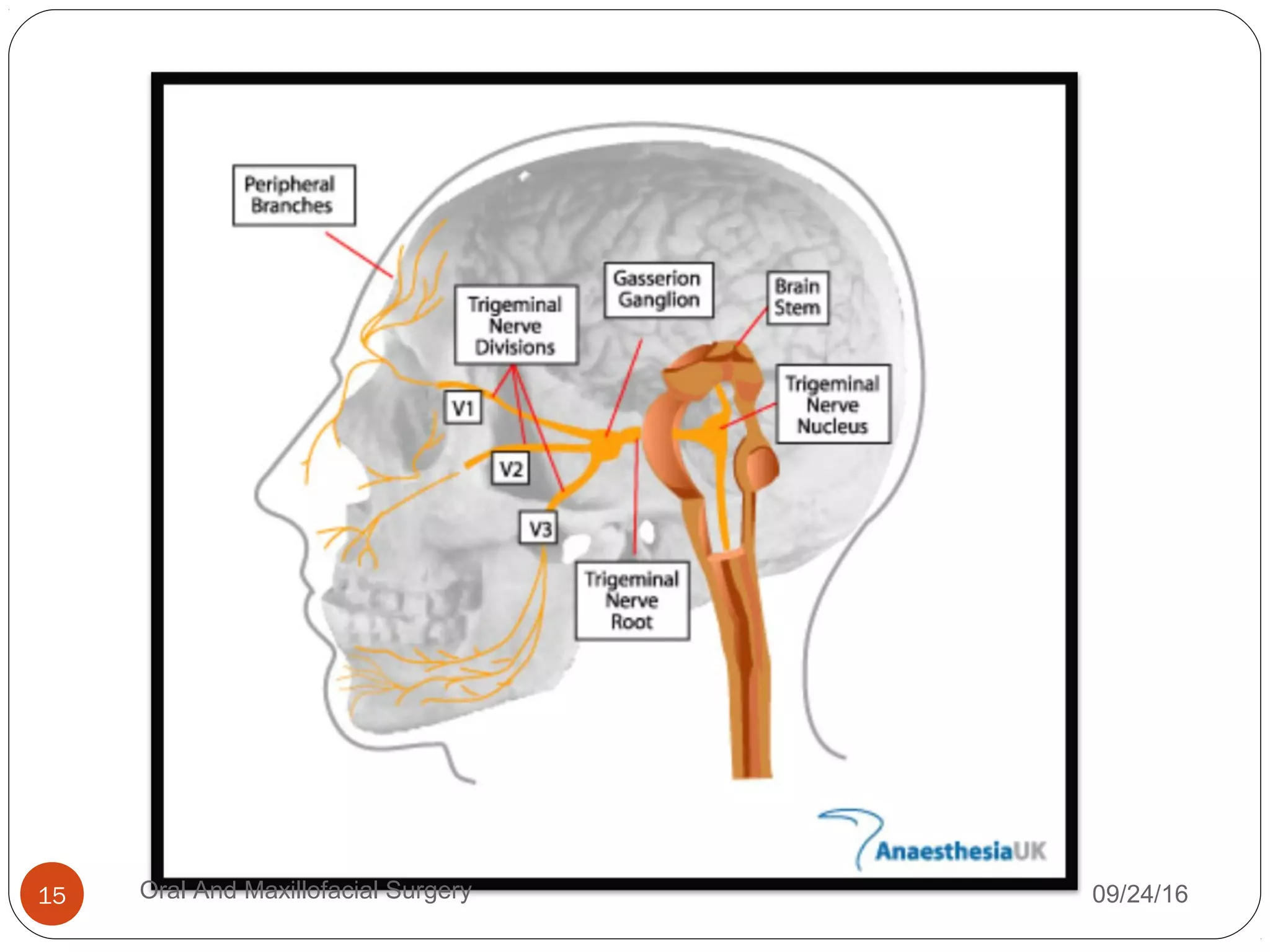
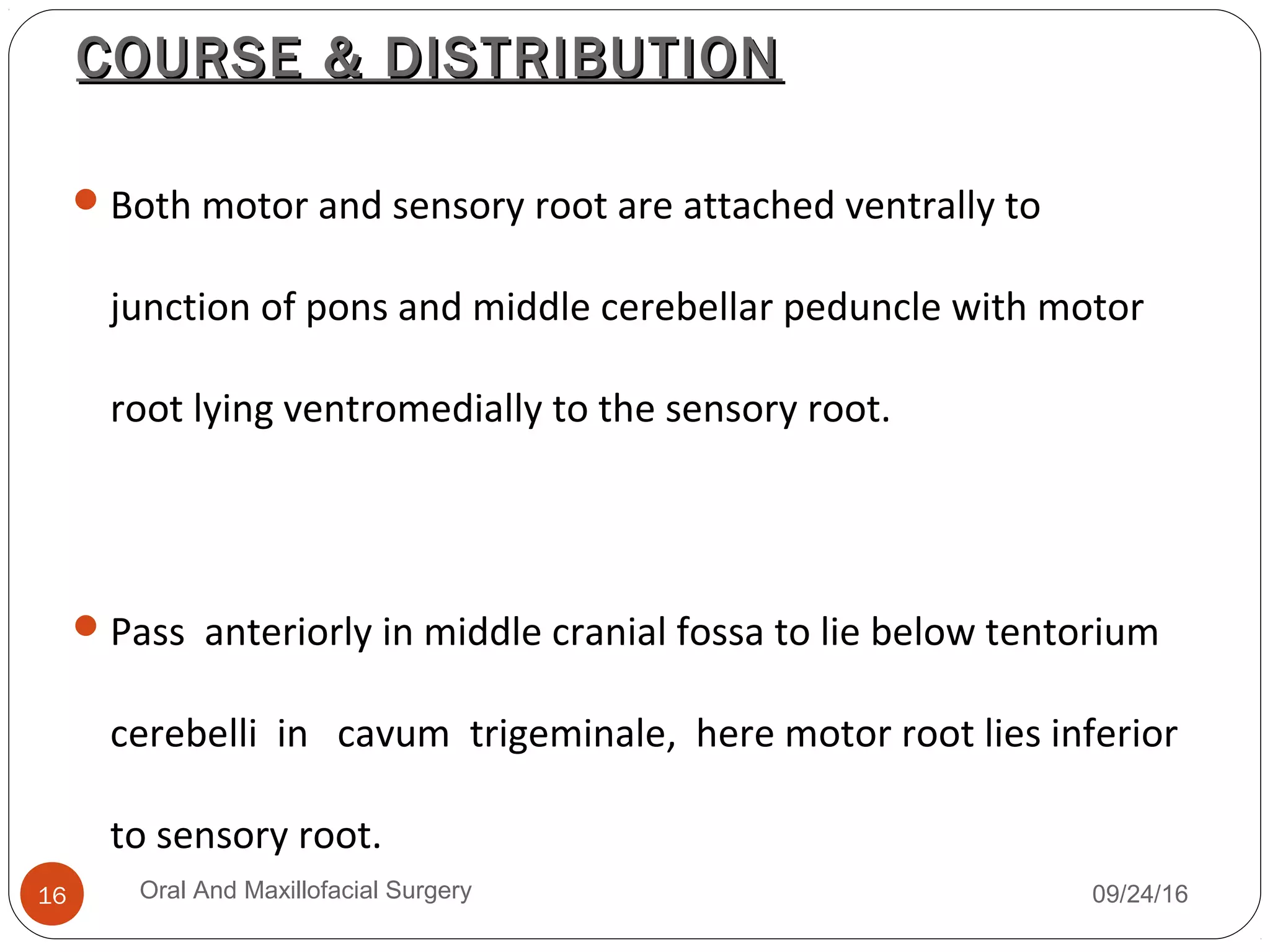
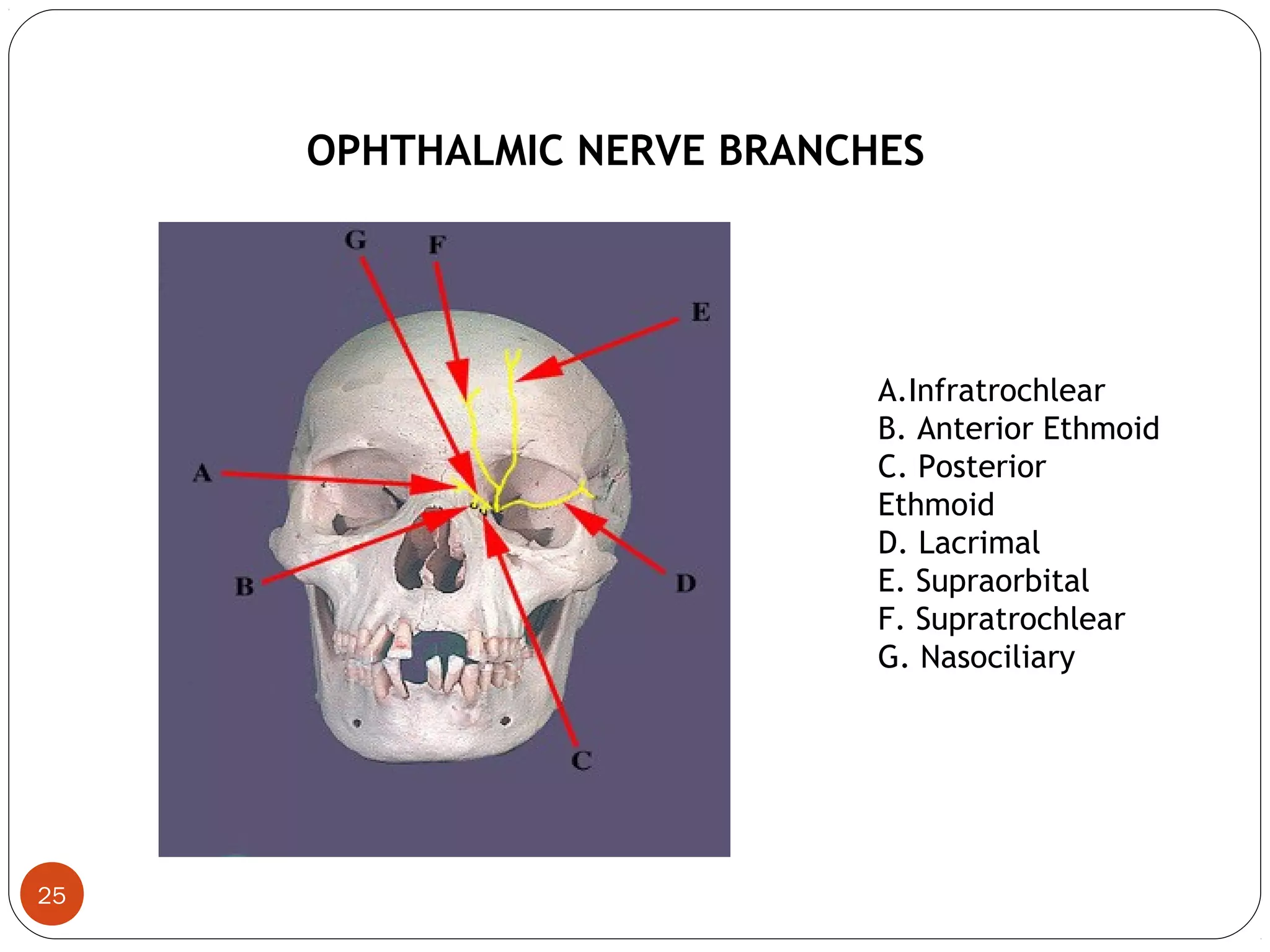
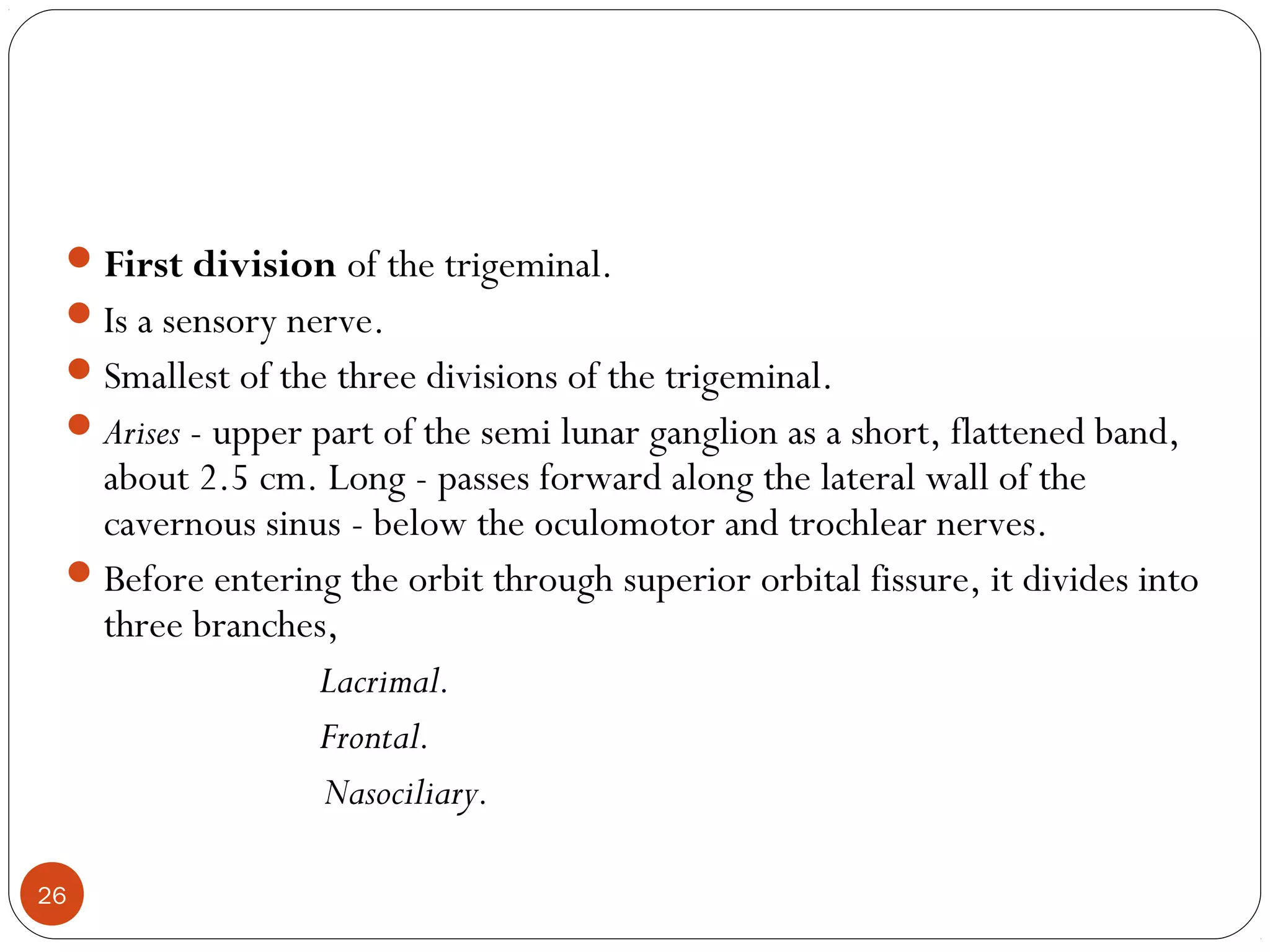
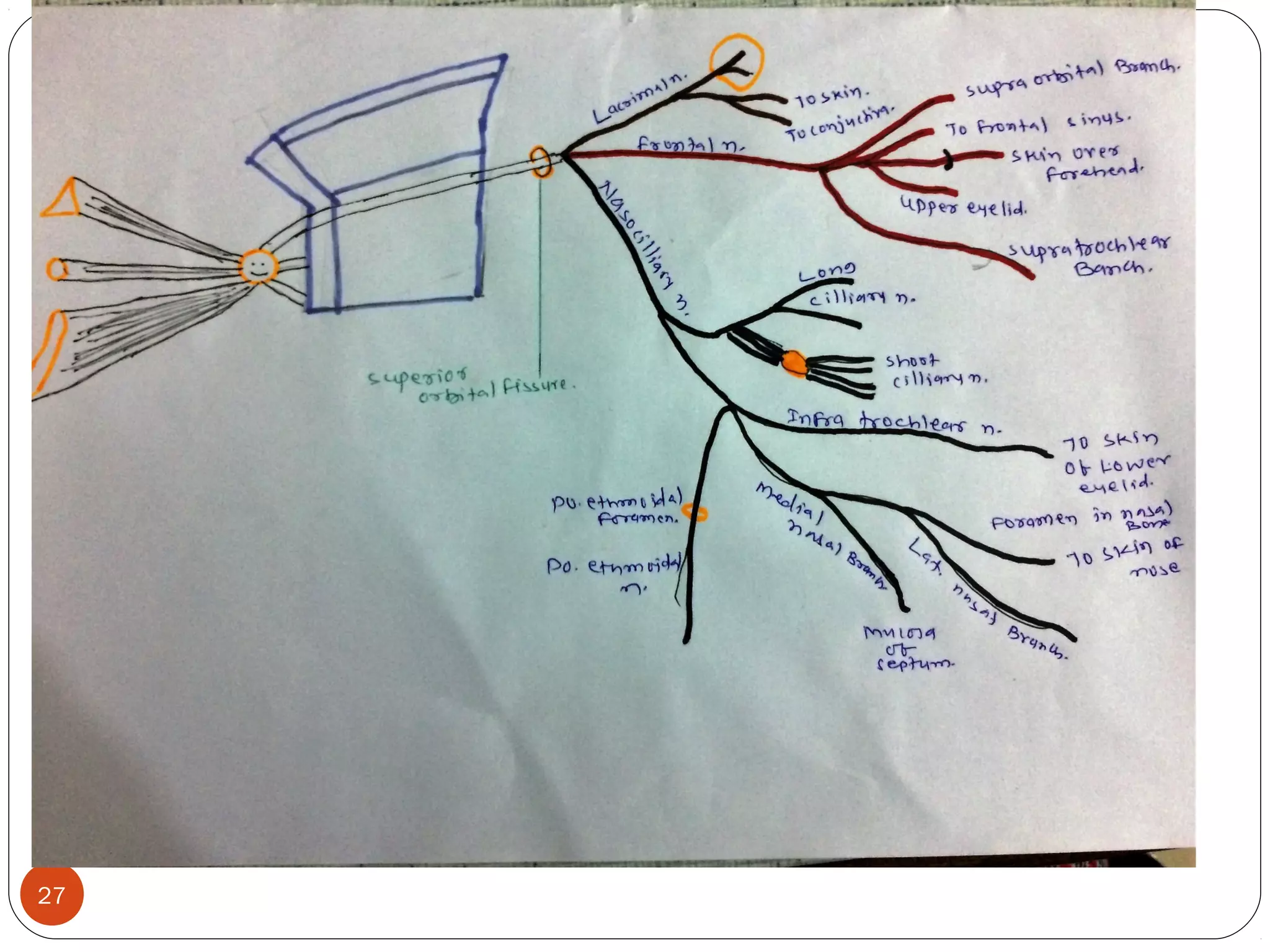
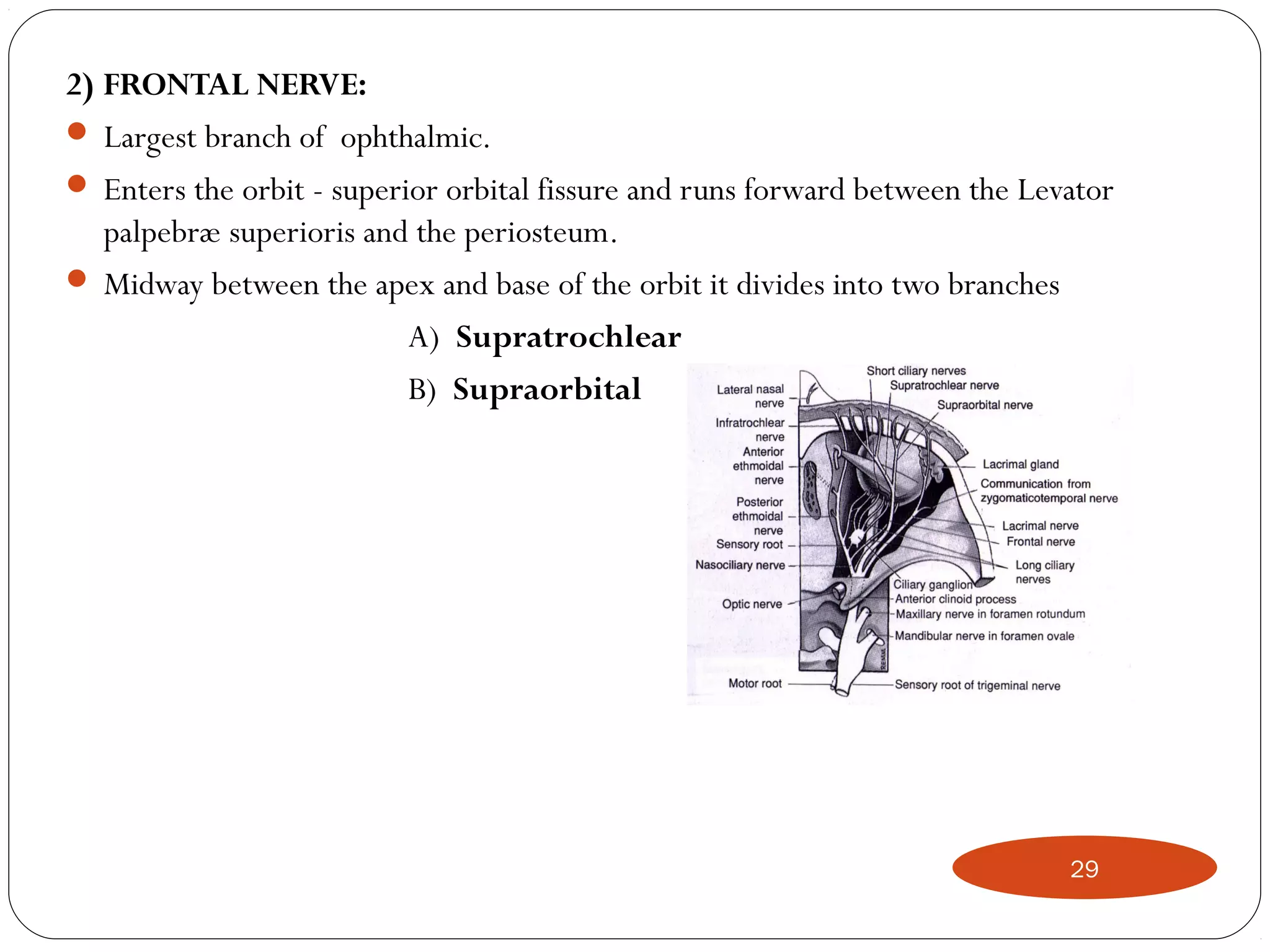
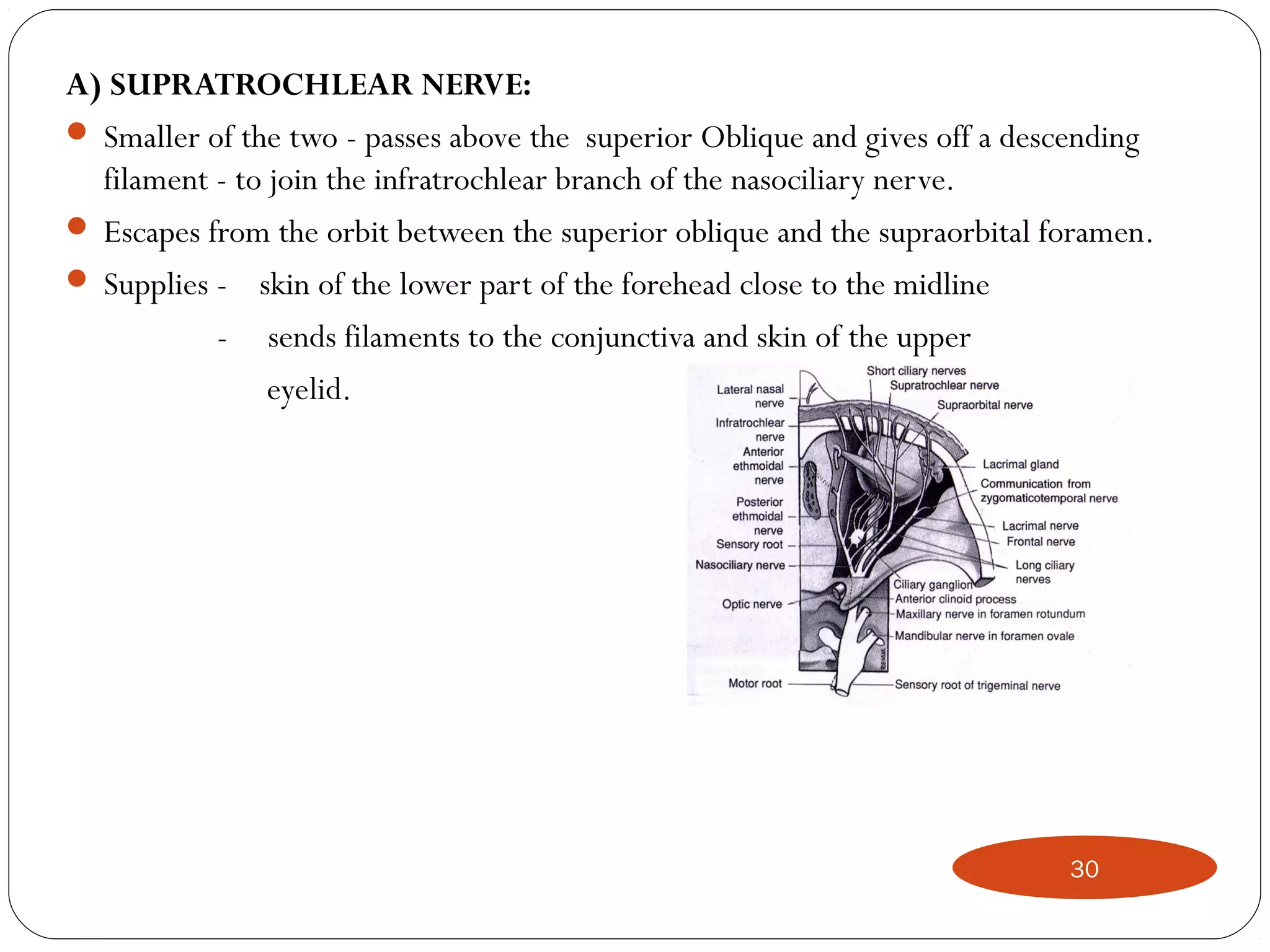
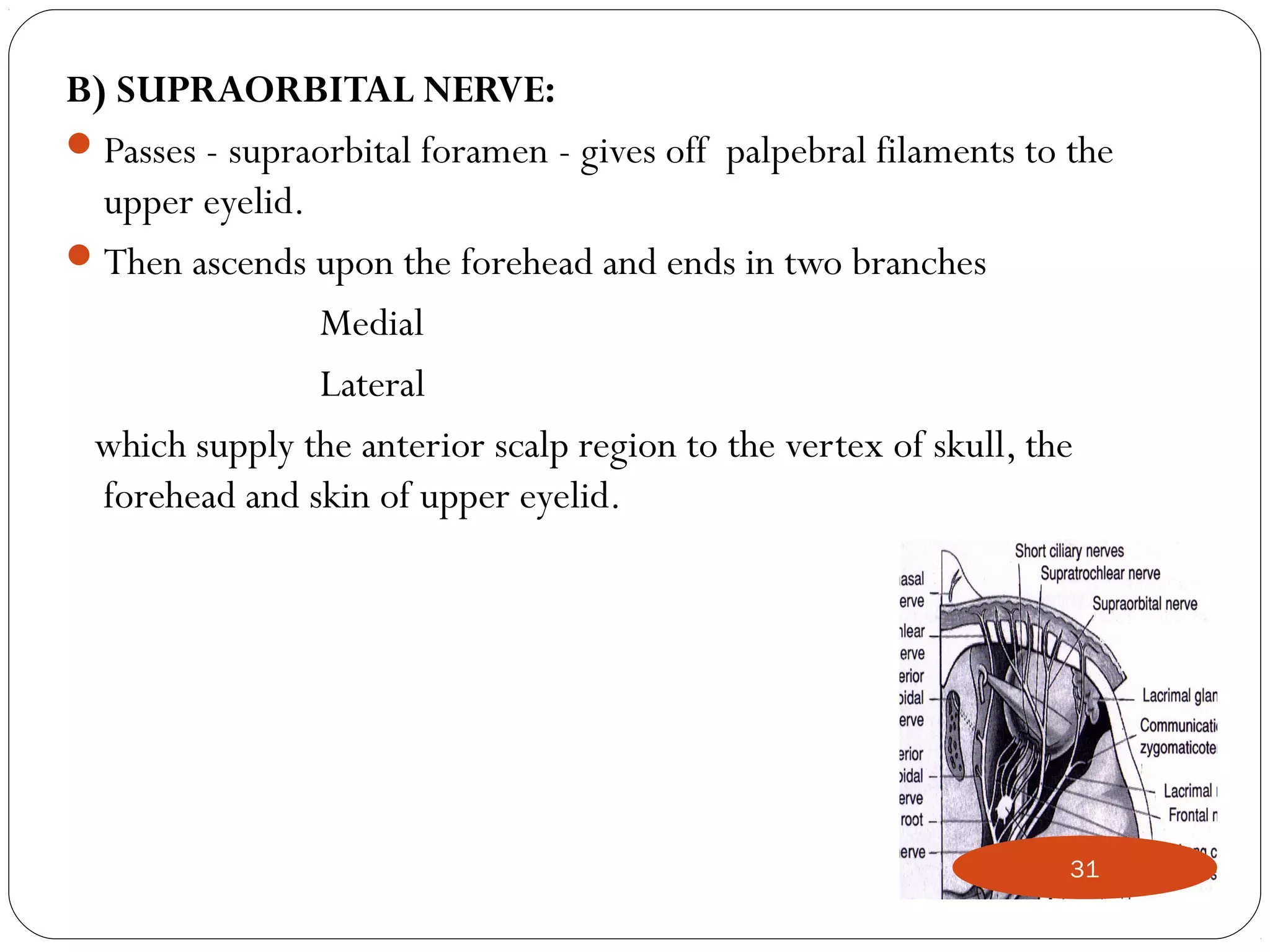
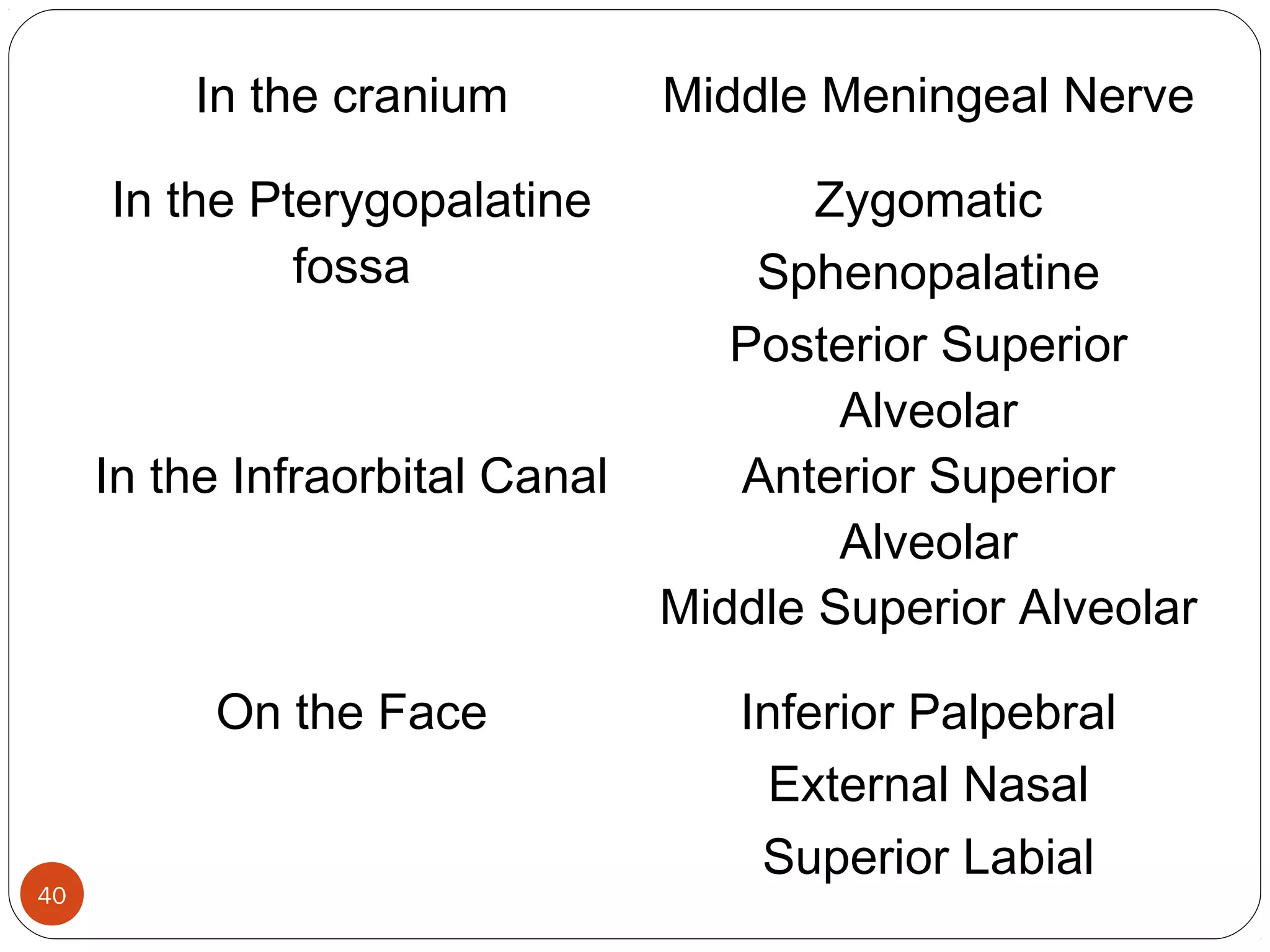
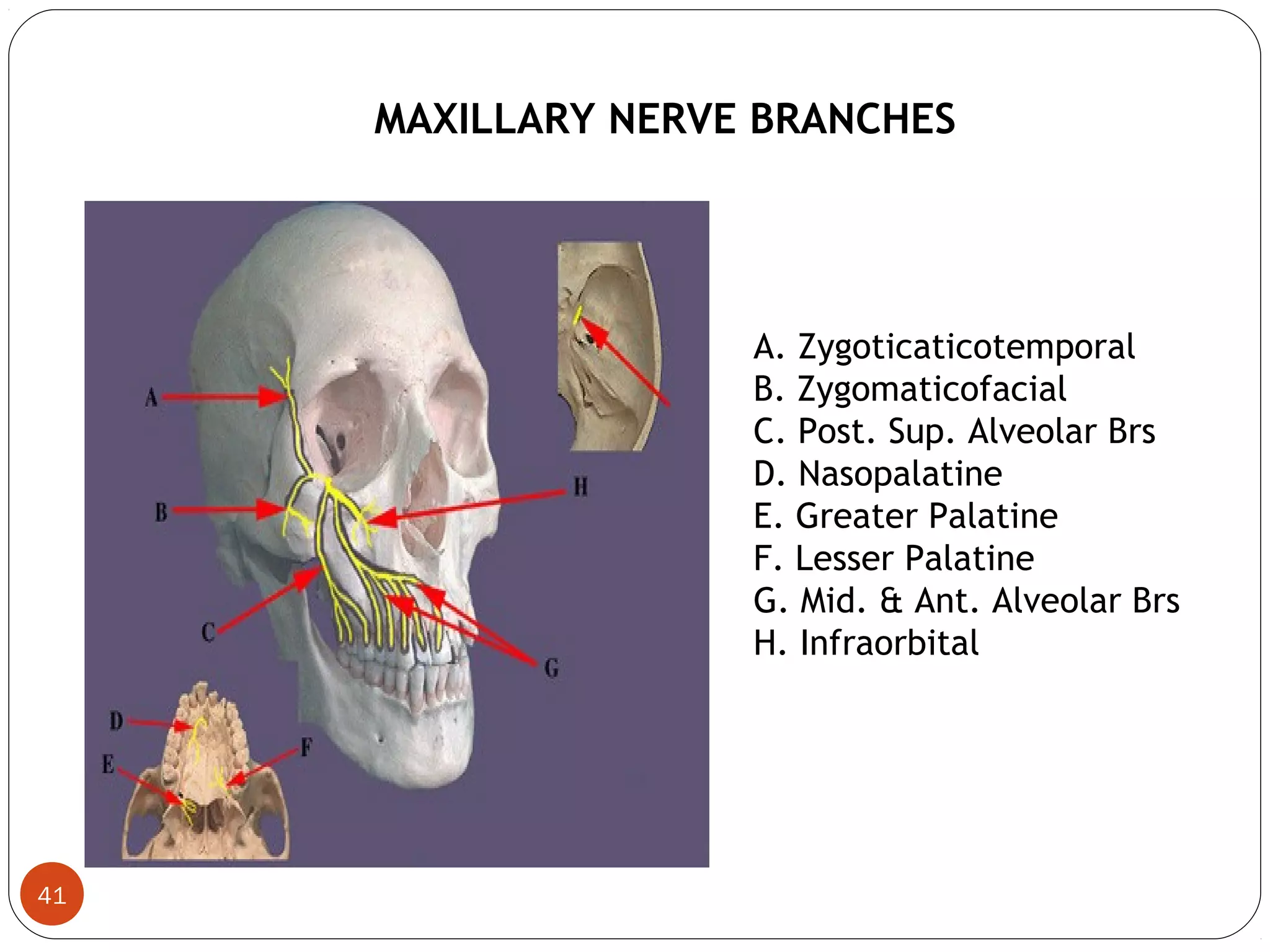
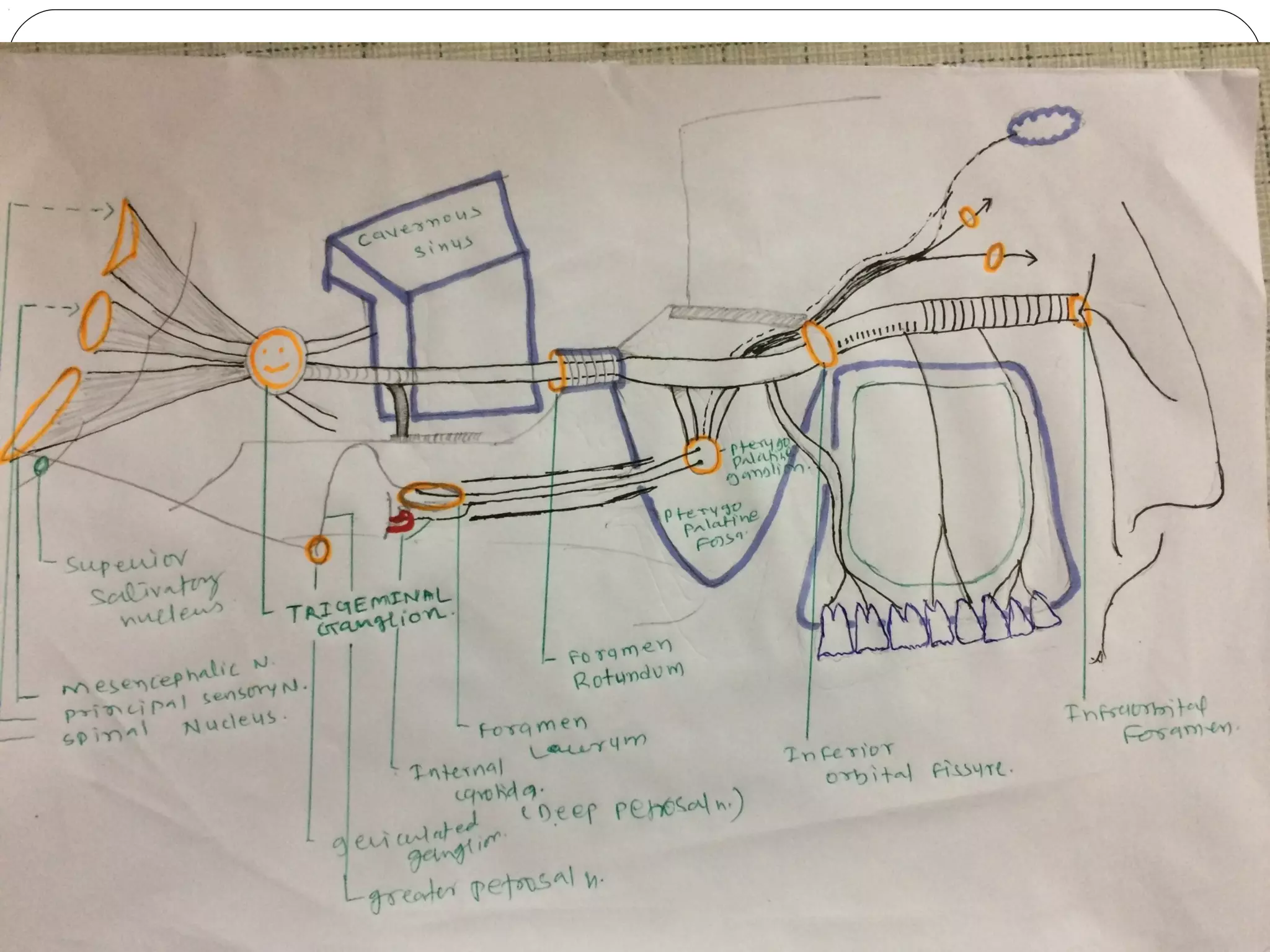
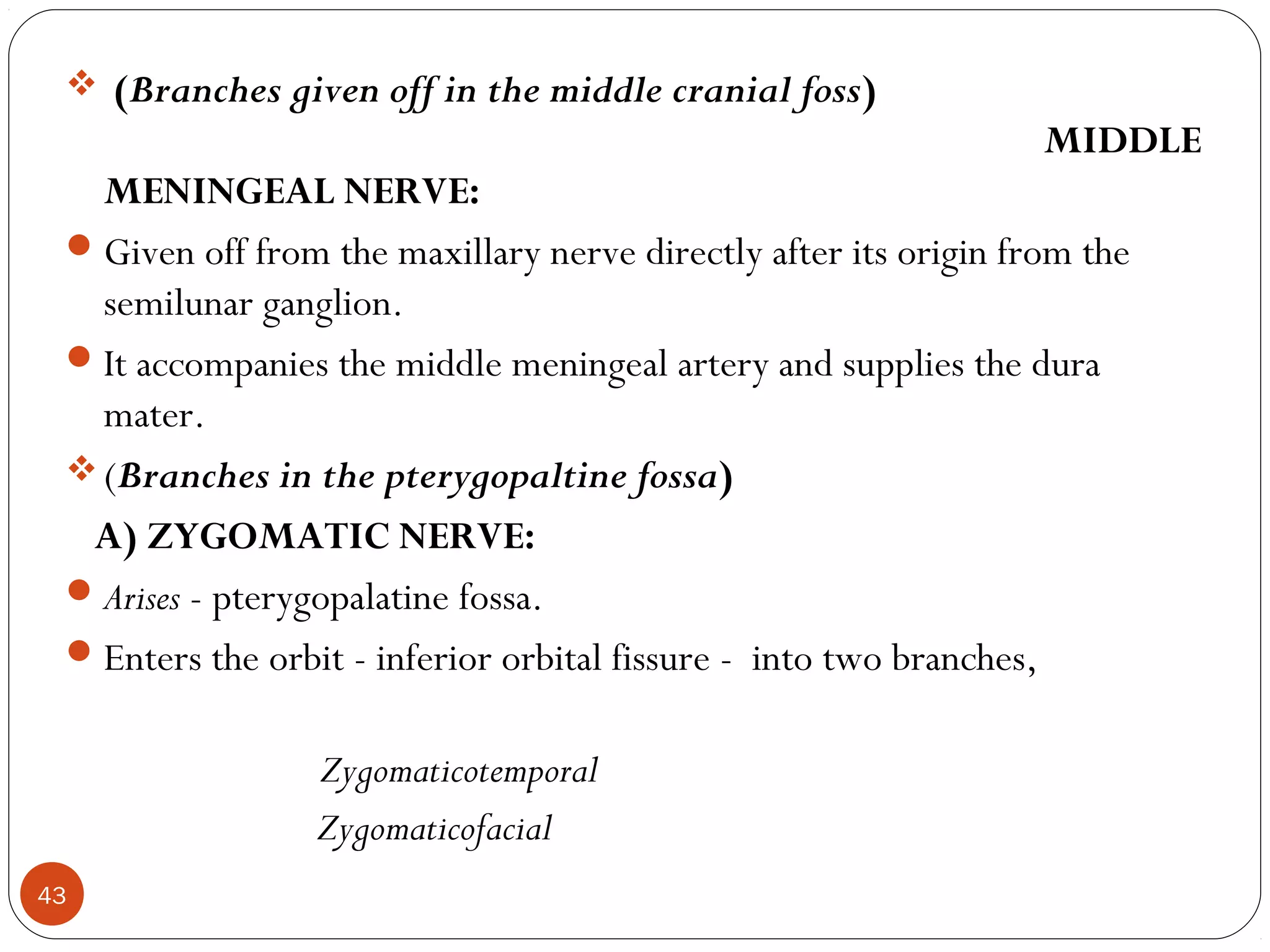
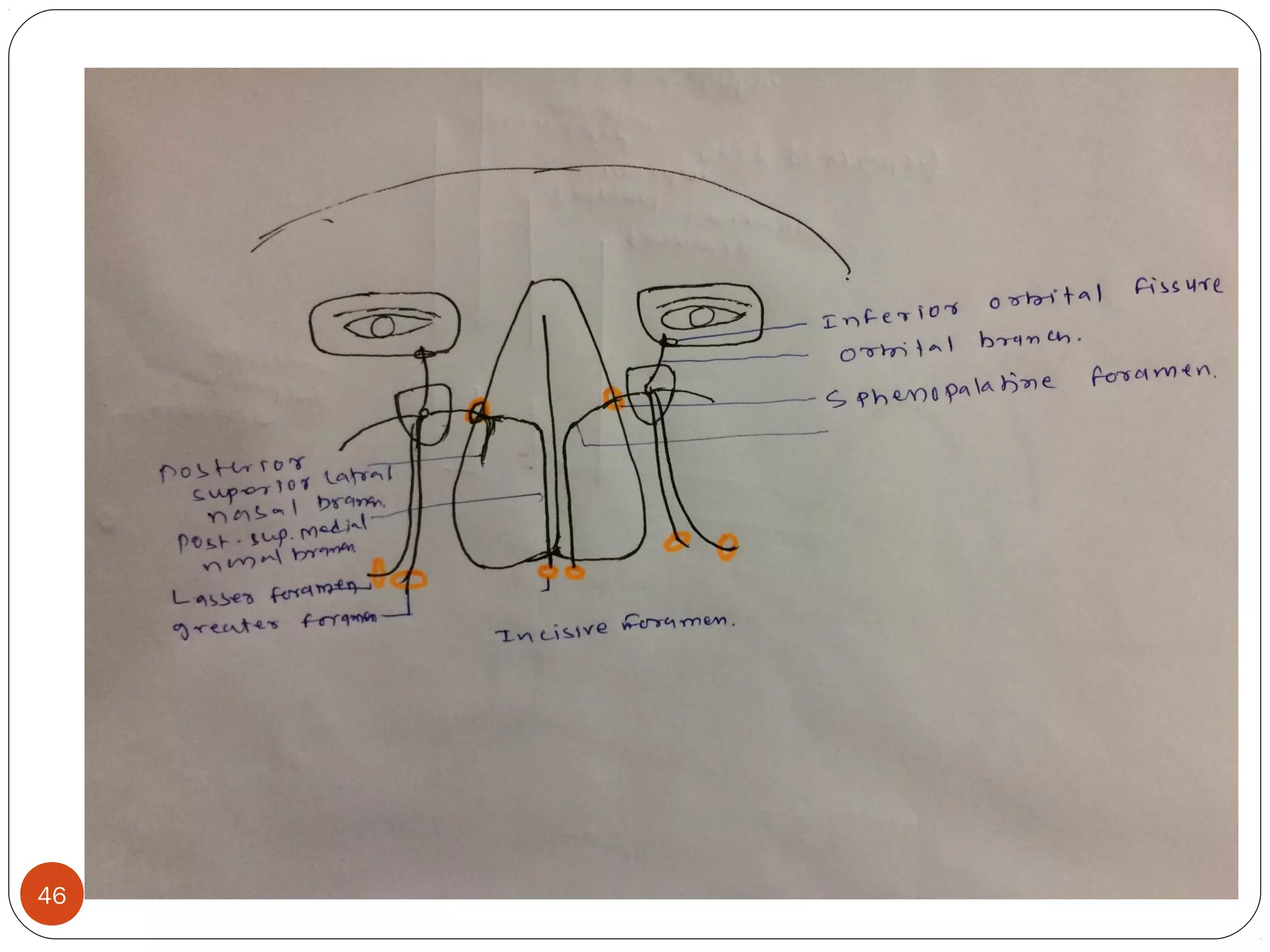
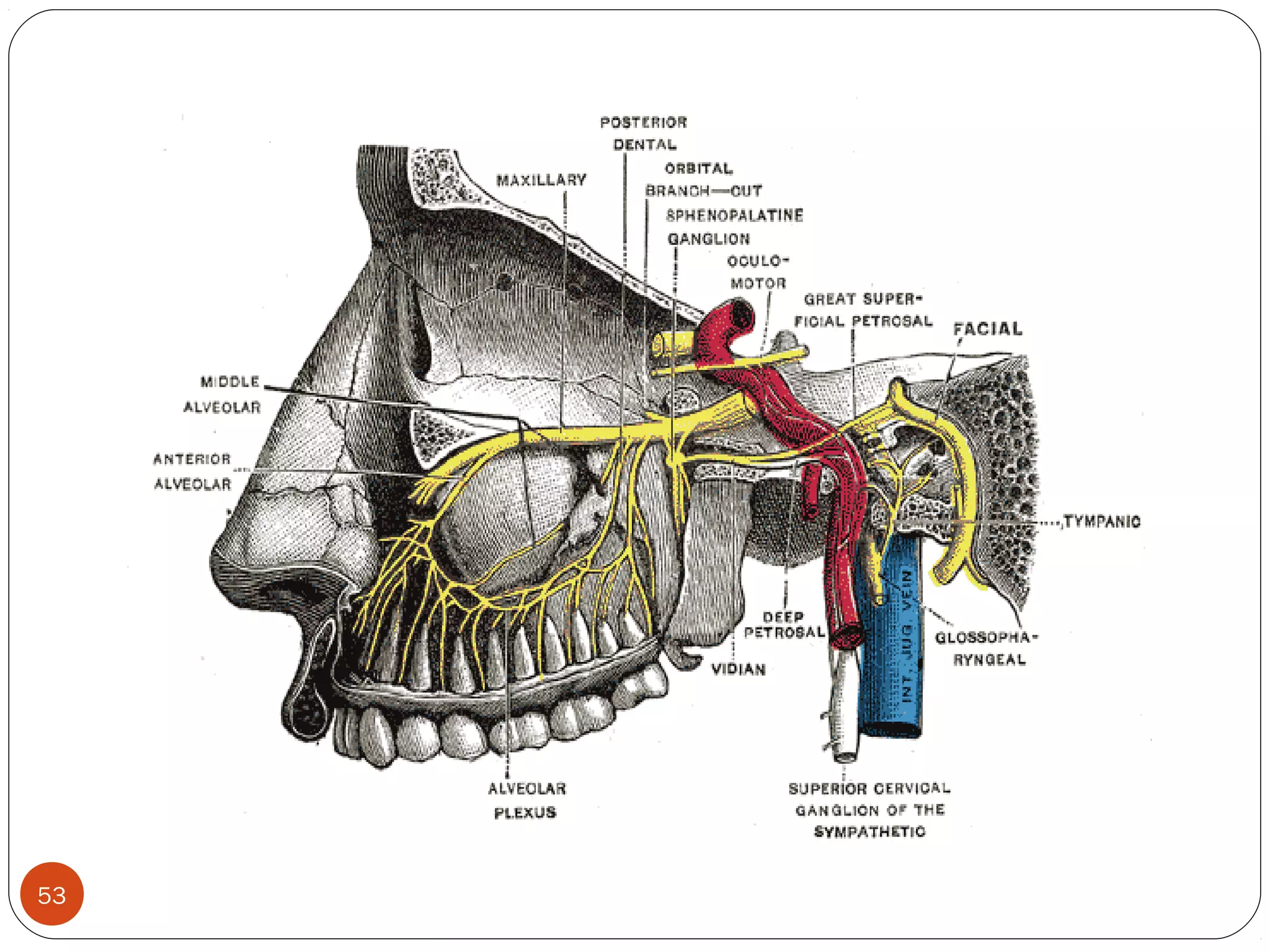
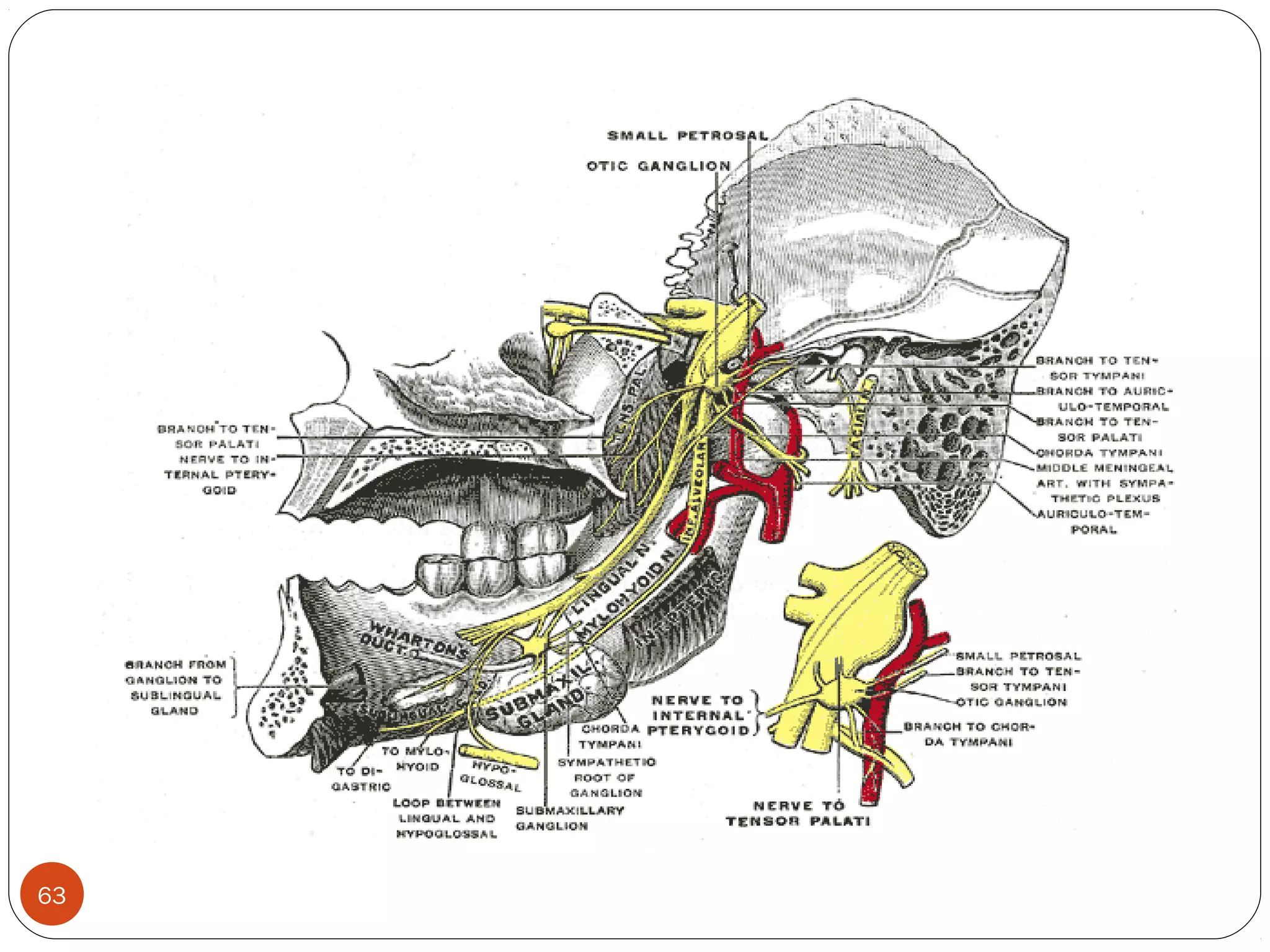
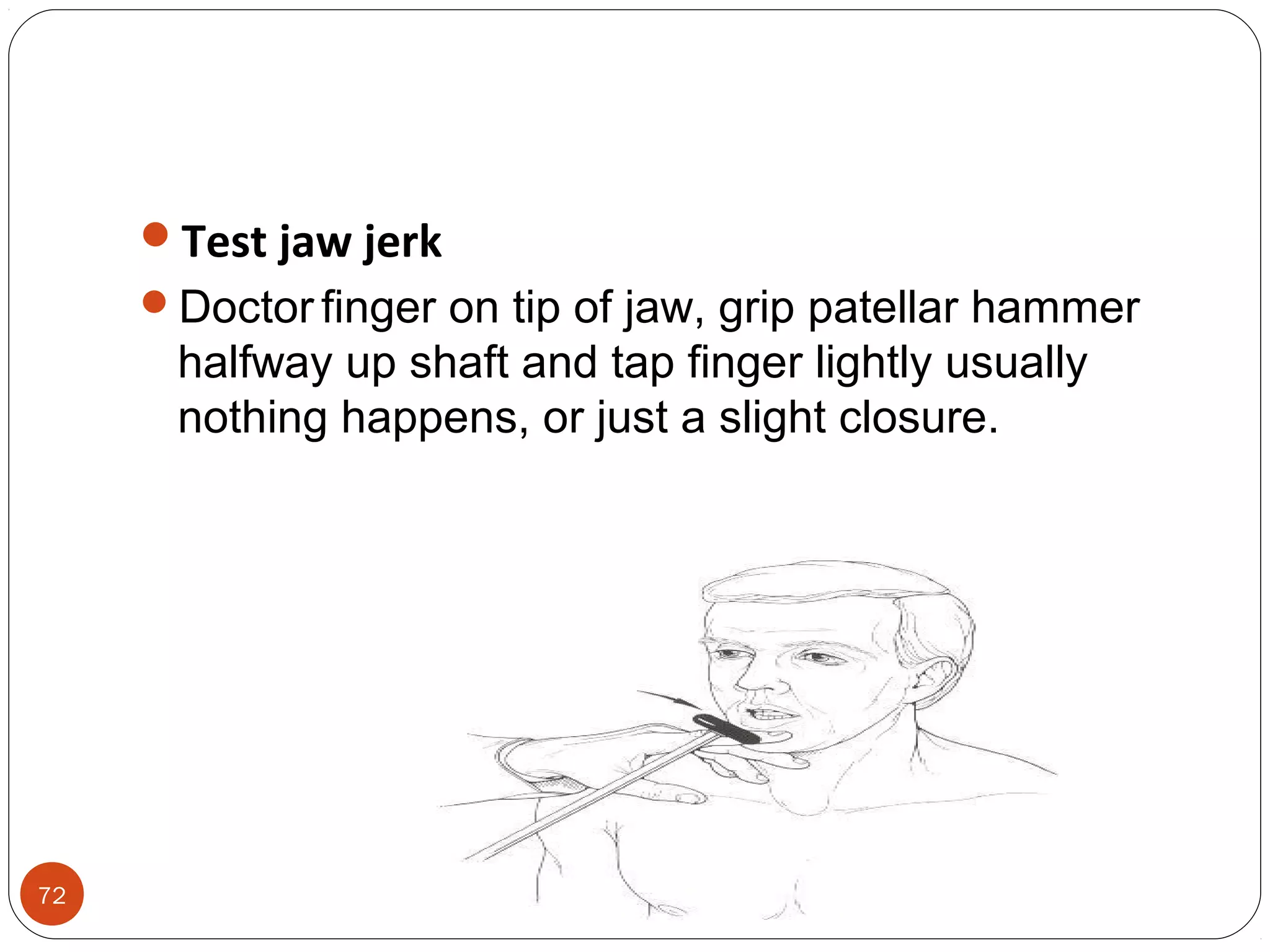
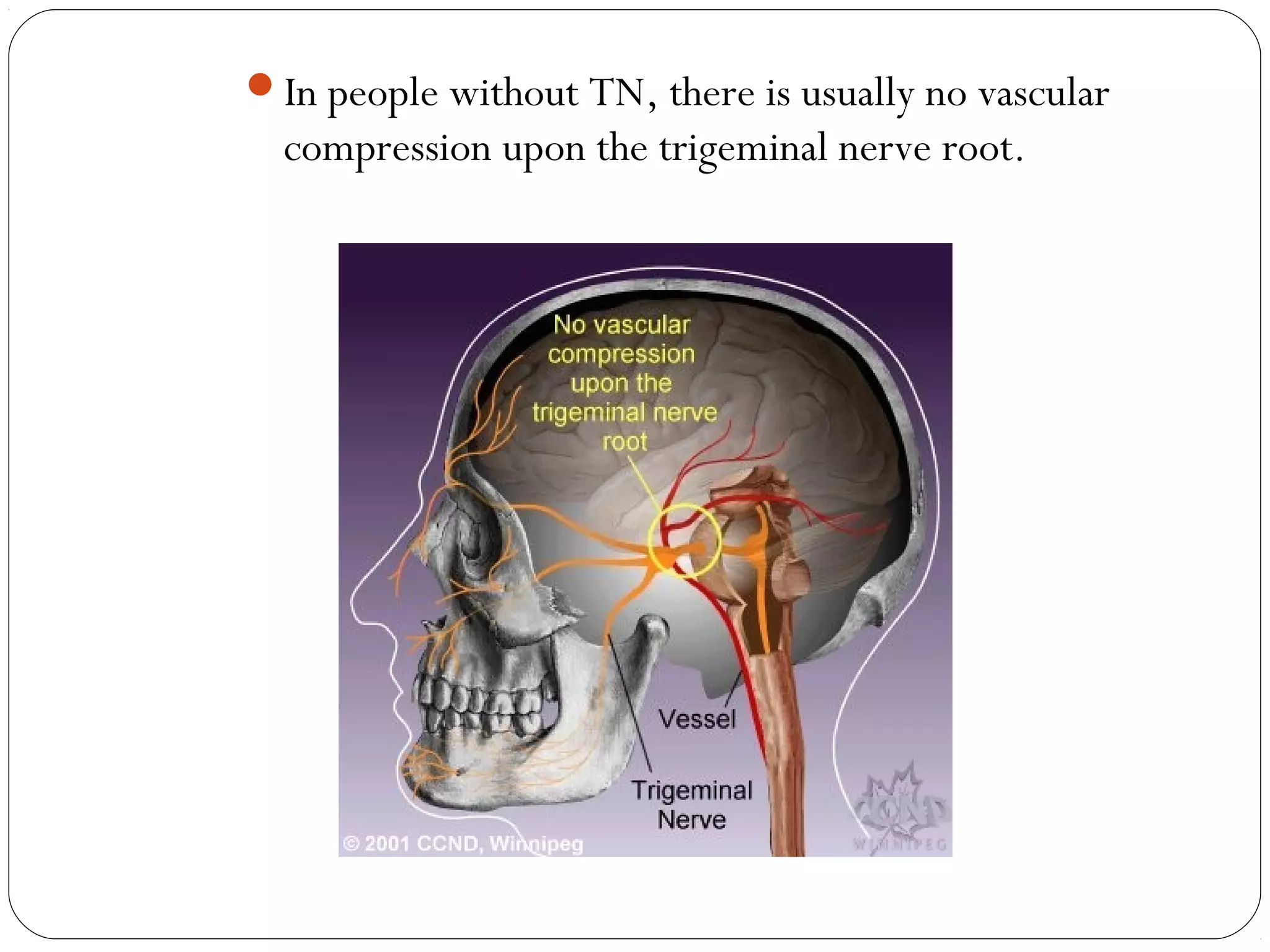
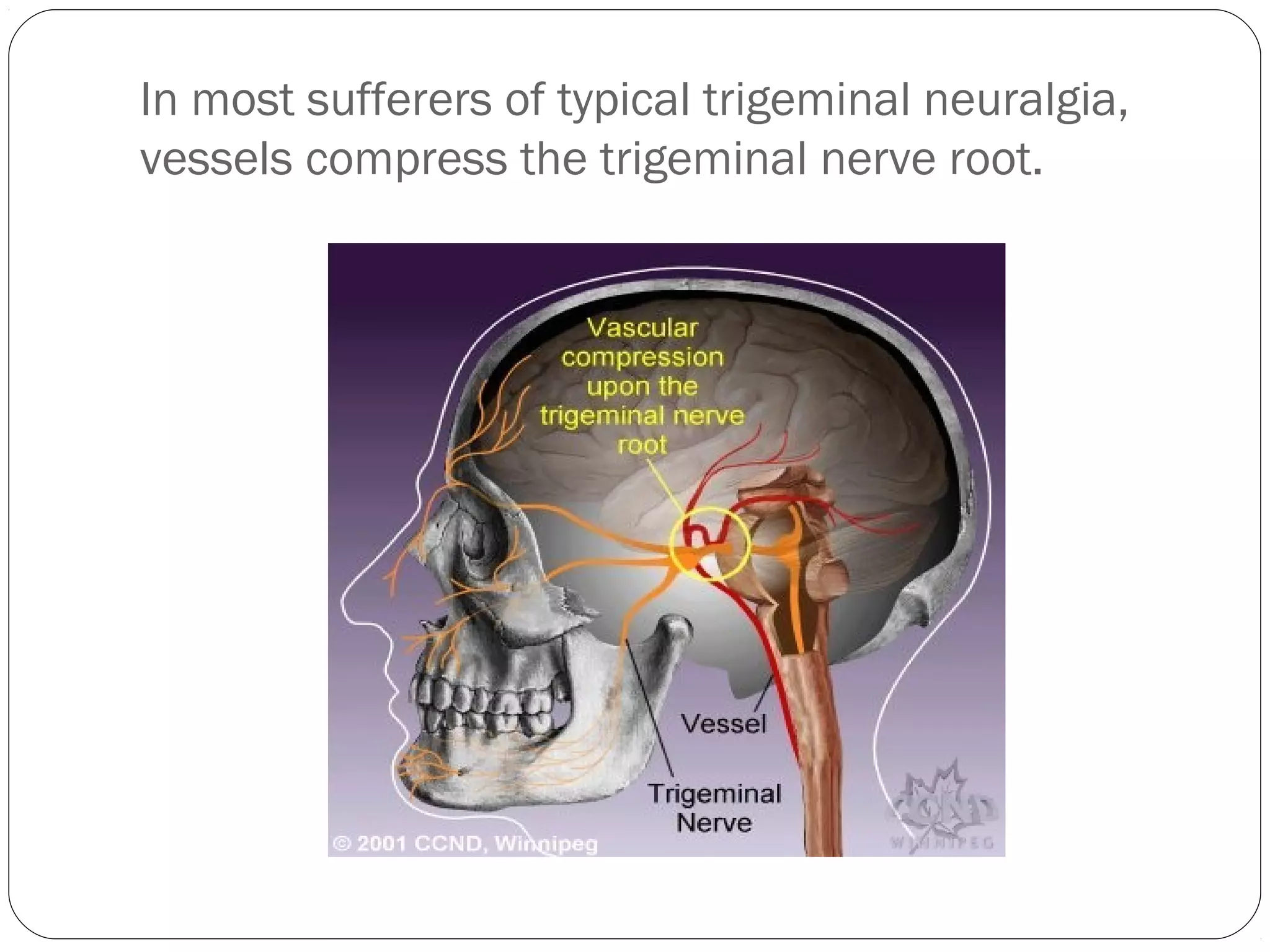
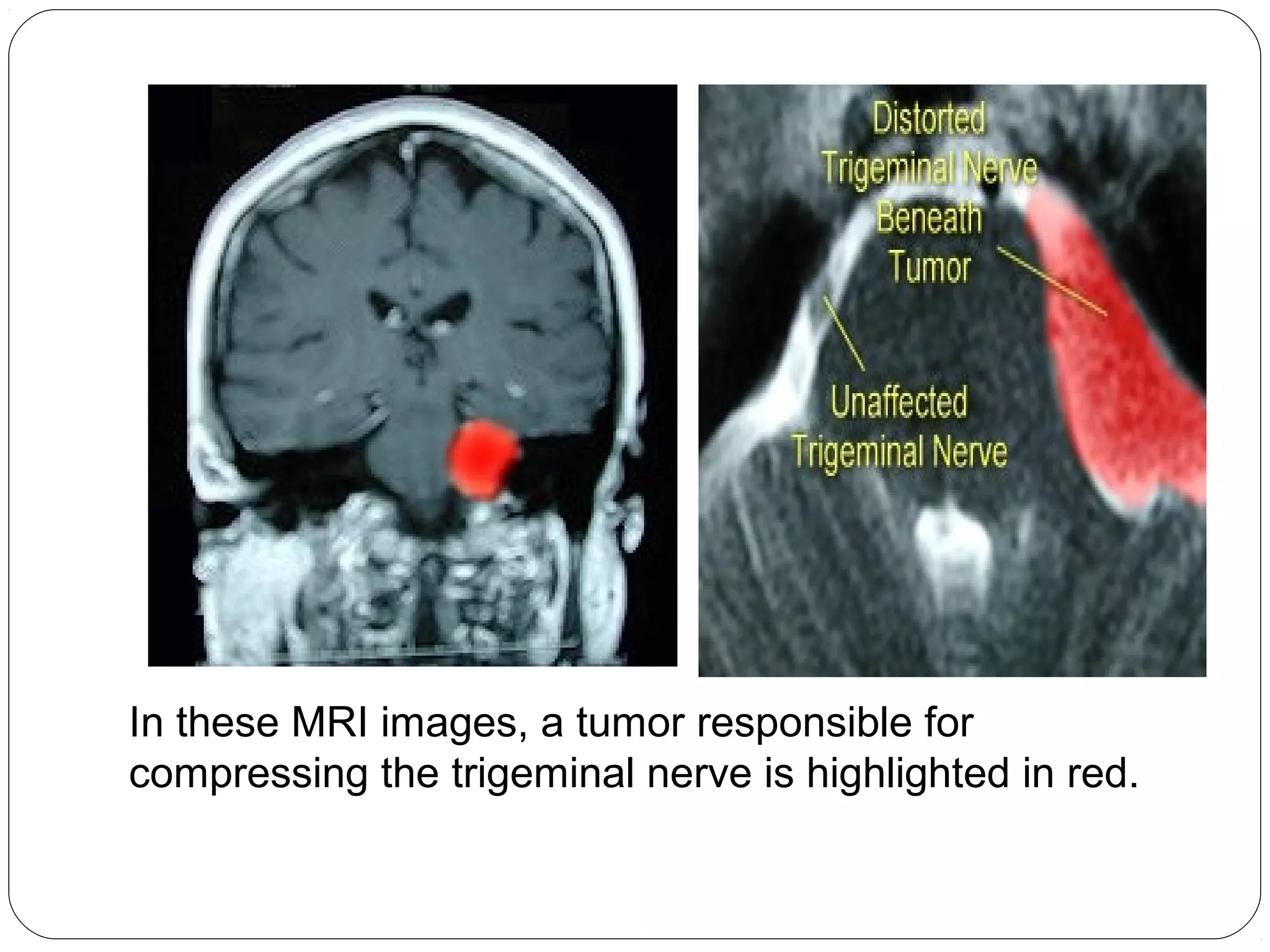
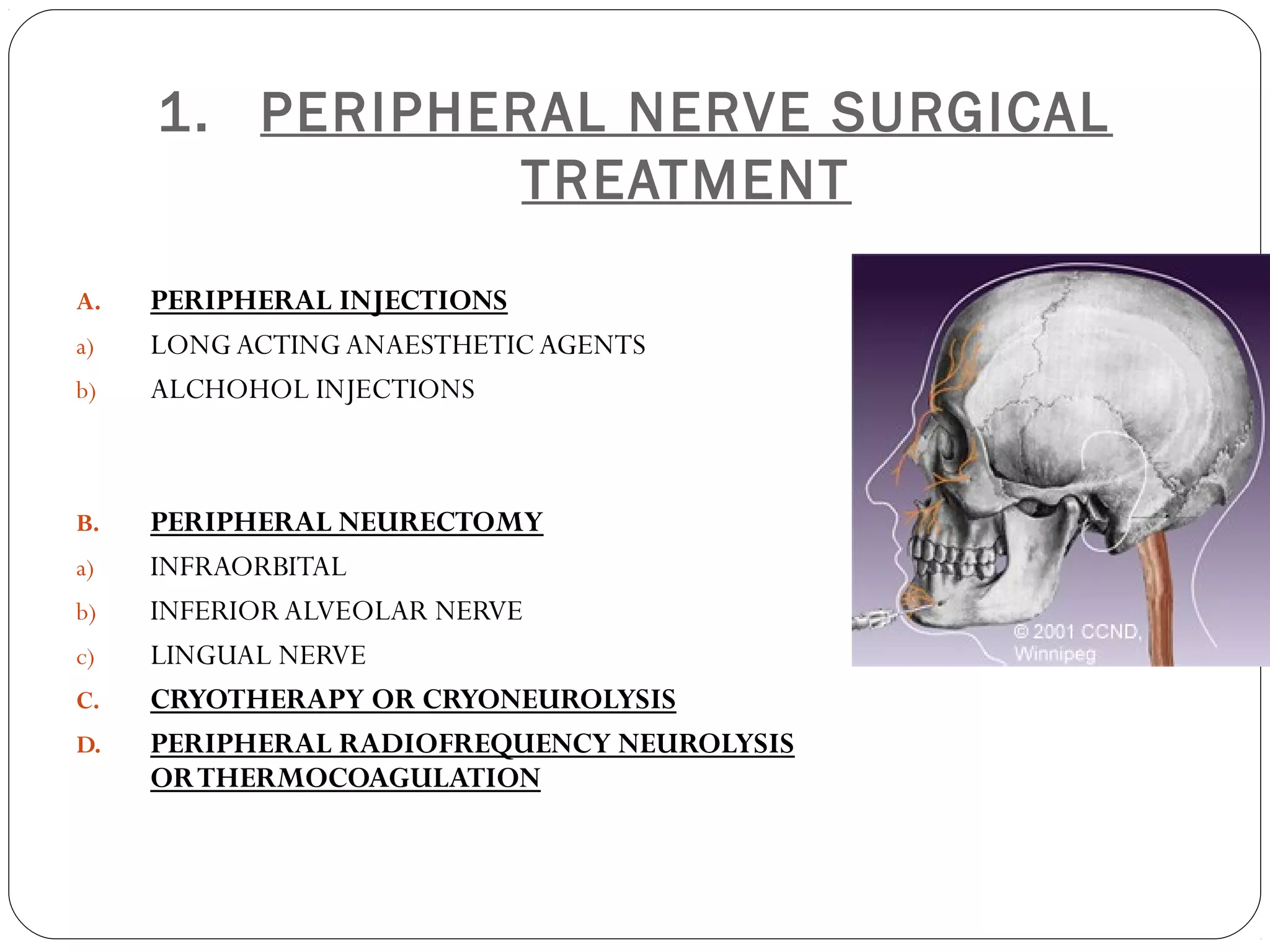
The document provides an in-depth overview of the trigeminal nerve, the largest cranial nerve, detailing its anatomy, functions, and branches. It describes the sensory and motor functions, the various nuclei associated with the trigeminal nerve, and the specific branches that arise from its divisions: ophthalmic, maxillary, and mandibular. Additionally, it covers the course and distribution of these branches and their functional components in relation to facial sensation and mastication.