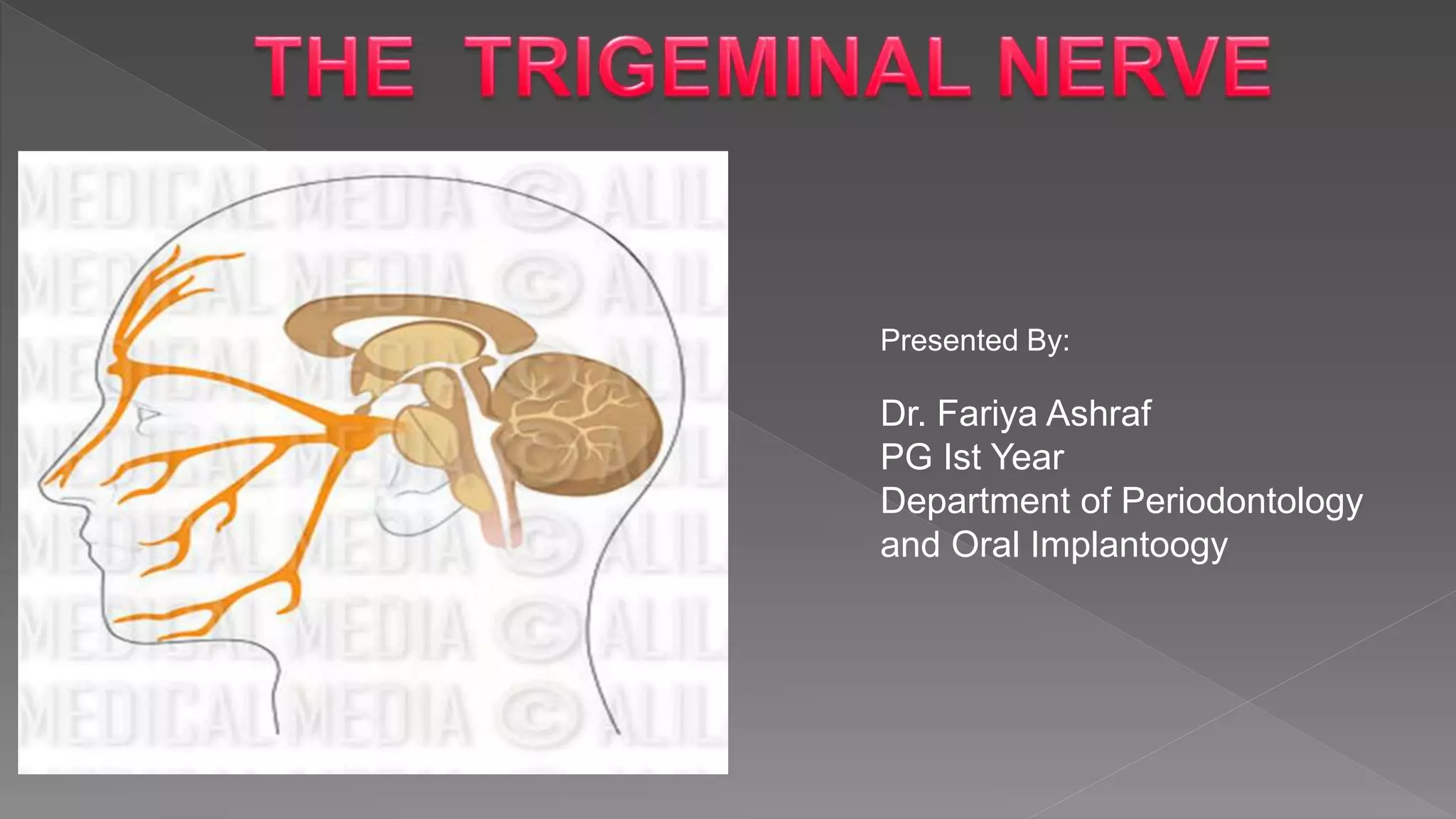
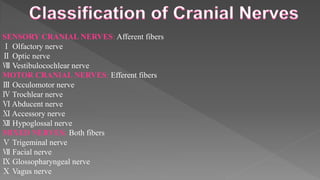
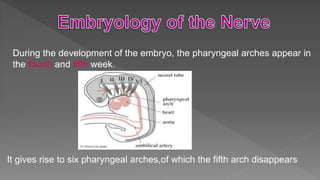
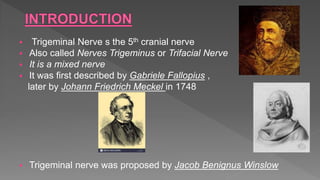
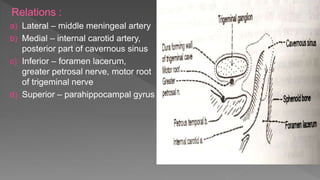
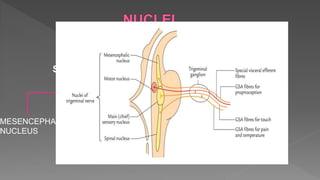
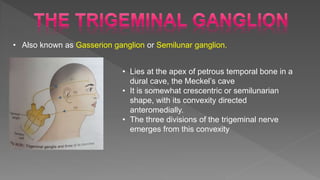
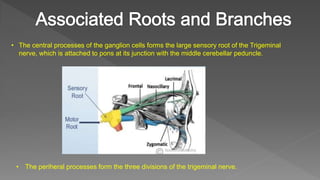
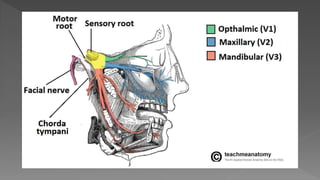
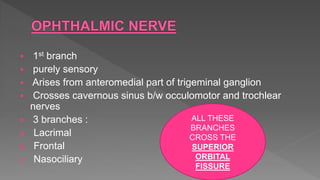
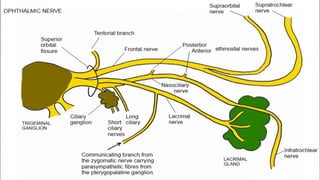
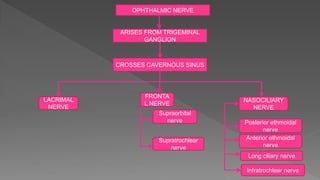
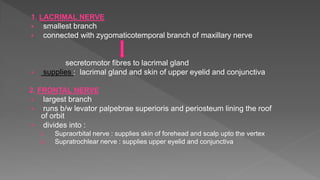
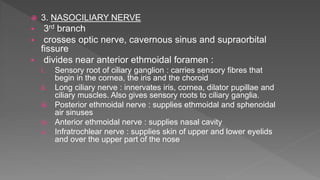
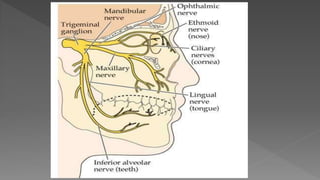
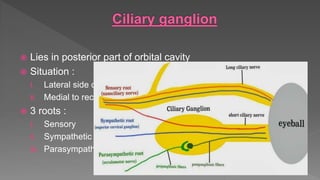
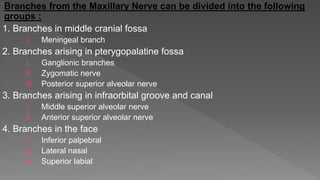
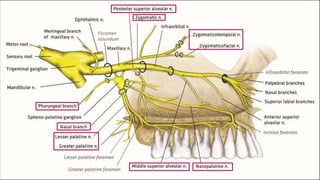
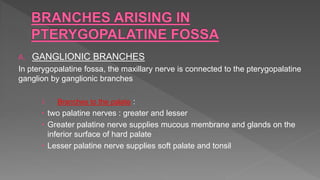
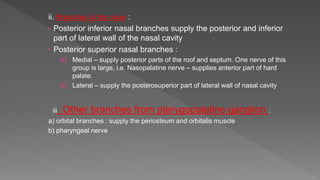
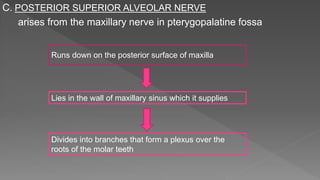
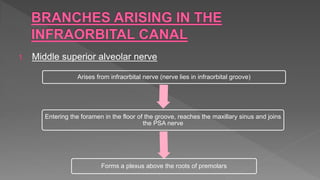
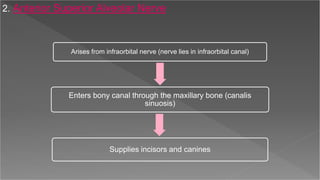
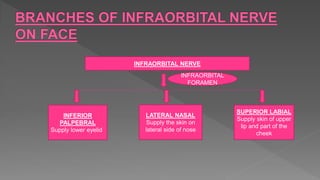
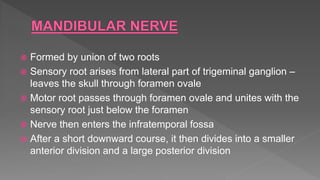
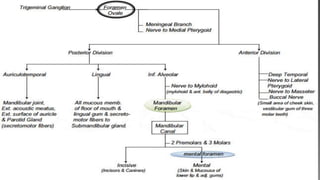
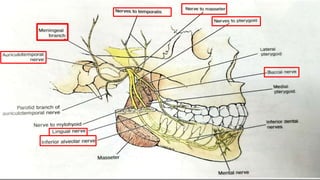
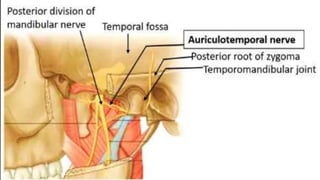
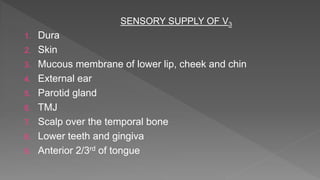
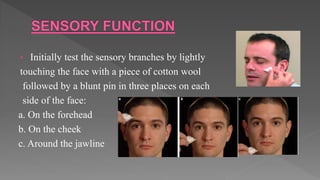
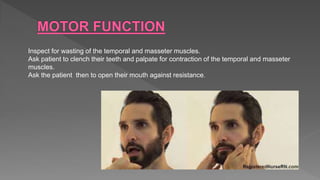
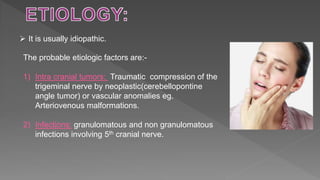
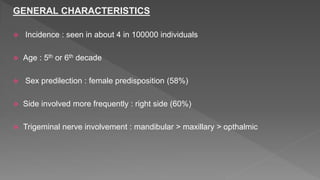
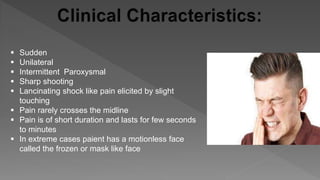
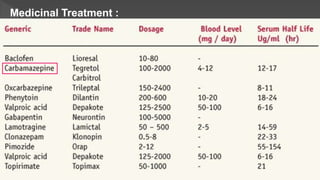
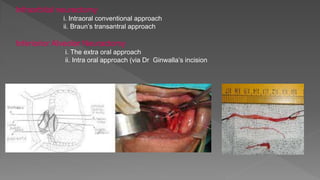
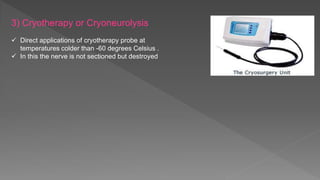
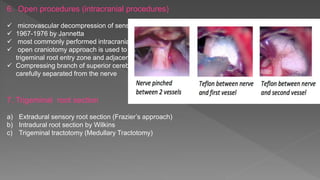
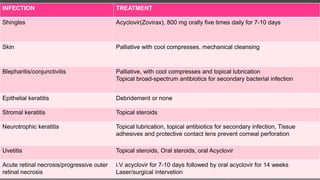
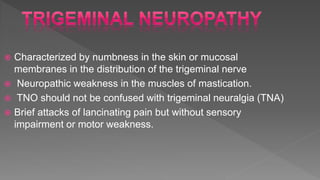
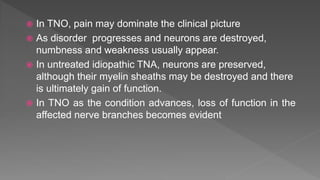
This document summarizes the trigeminal nerve, including its embryology, anatomy, branches, functions and clinical considerations. It begins with the embryology of the pharyngeal arches and how they relate to nerve development. It then describes the trigeminal ganglion, roots and nuclei. The three divisions of the trigeminal nerve and their branches are outlined. Clinical tests for examining the trigeminal nerve and classifying injuries are summarized. Common causes of trigeminal nerve injuries and their treatment approaches are briefly discussed.