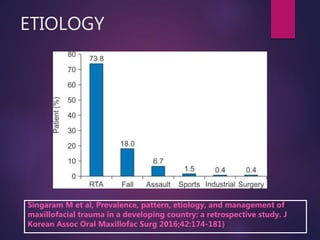
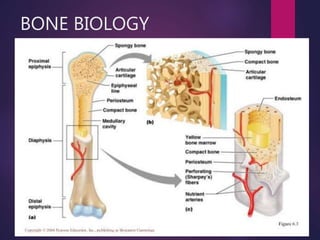
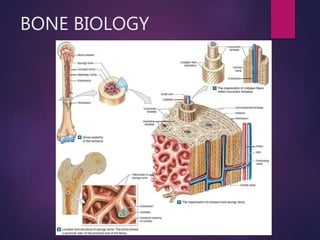
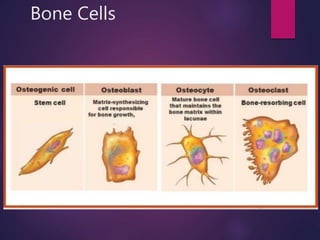
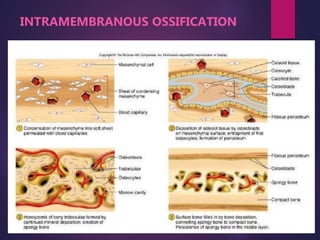
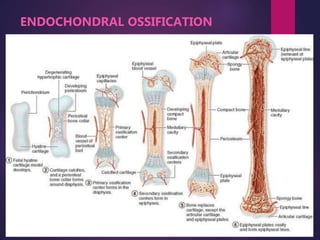
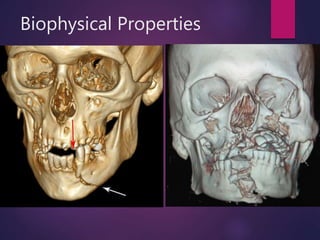
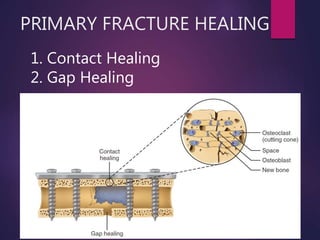
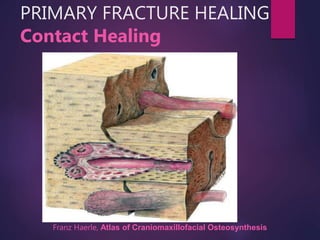
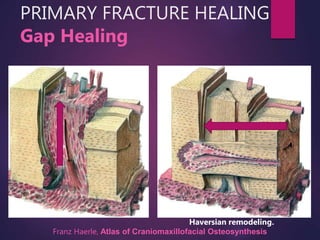
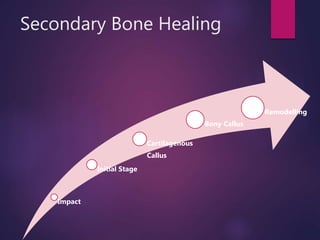
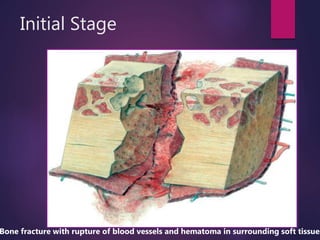
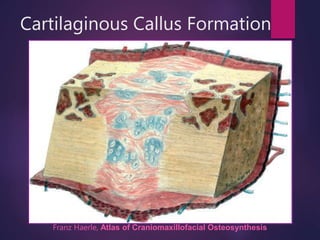
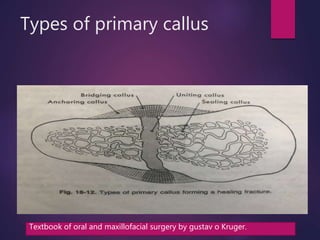
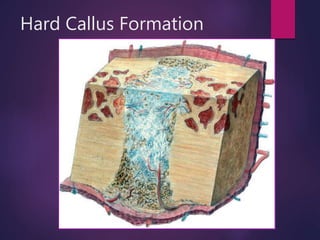
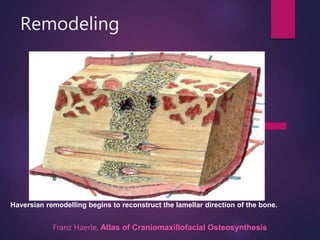
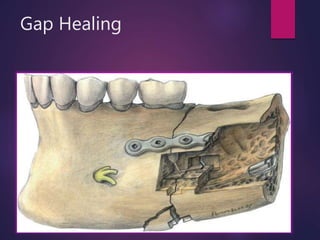
The document discusses fracture healing, presenting different types such as primary and secondary healing, and their respective mechanisms including intramembranous and endochondral ossification. It highlights the complications of fracture healing like non-union and mal-union, along with their etiology and management strategies. The conclusion emphasizes the importance of understanding bone healing science for optimal treatment outcomes.