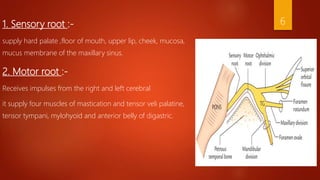
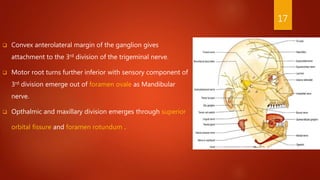
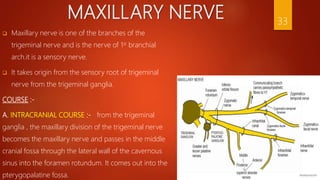
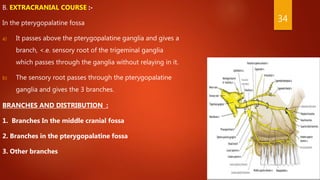
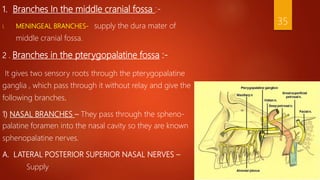
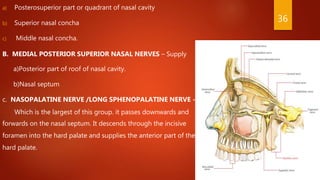
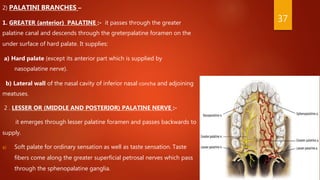
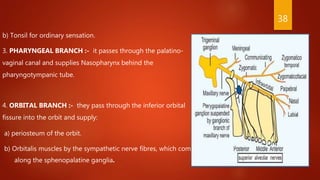
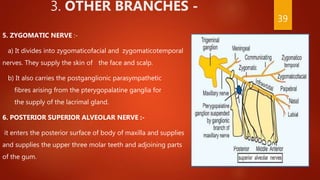
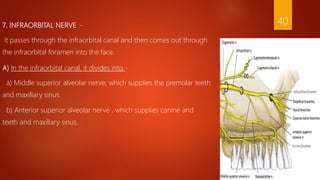
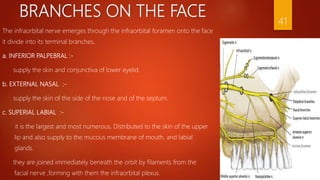
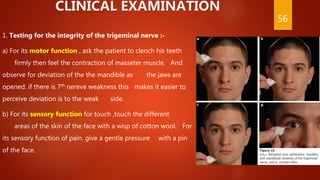
The maxillary nerve is a branch of the trigeminal nerve that arises from the trigeminal ganglia and provides sensory innervation to parts of the face, nasal cavity, and palate. It passes through the foramen rotundum into the pterygopalatine fossa where it gives off branches including the nasopalatine nerve that supplies the hard palate and nasal septum, and the greater and lesser palatine nerves that innervate the palate. The infraorbital nerve is a terminal branch that emerges on the face through the infraorbital foramen and divides further to innervate the lower eyelid, nose, upper lip, and gums.