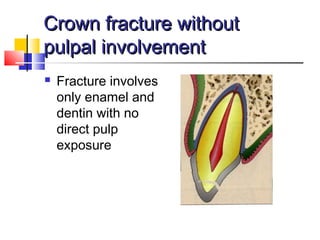
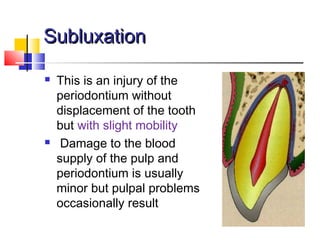
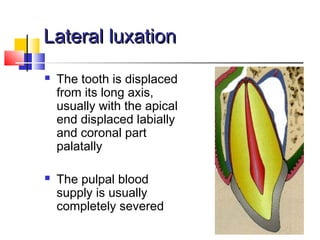
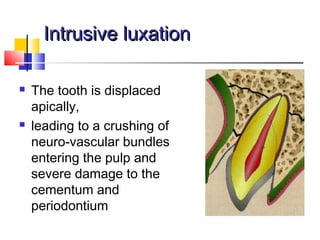
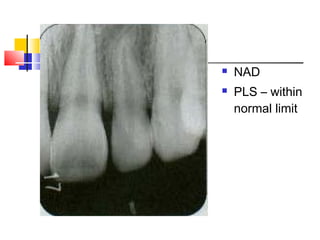
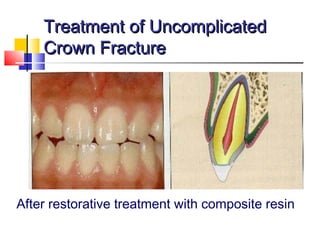
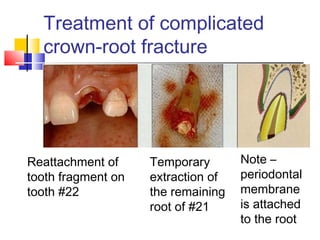
The document discusses traumatic injuries to anterior teeth in children, highlighting the psychological impact on both the child and parents. It outlines the causes, classification, diagnosis, and treatment of various dental injuries while emphasizing the critical role of timely intervention by dentists to preserve tooth vitality and aesthetics. Furthermore, it details specific case studies illustrating the complexities of treating such injuries and the importance of thorough clinical examination and documentation.