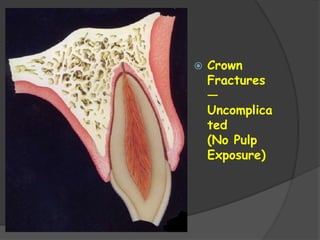
The document discusses classification systems and types of dental injuries. It describes soft tissue injuries, tooth fractures including enamel fractures and uncomplicated crown fractures without pulp exposure. For uncomplicated crown fractures, the goals of emergency treatment are to protect the pulp by placing a protective material over exposed dentin, reduce discomfort, preserve pulp vitality, and restore the fractured crown area.

























































![TREATING CORONAL & APICAL FRAGMENTS AT THE
SAME TIME:
It is difficult to get apical seal when endodontically treating only
coronal fragment.
To achieve this seal --- treatment of both coronal & apical fragment
simultaneously which is almost impossible.
low success rate
Favorable approximation of fragments --- intra radicular splint ---
rigid type of post (cobalt – chromium alloy [vitallium])](https://image.slidesharecdn.com/traumaticinjuries-220812091550-9ae6e120/85/TRAUMATIC-INJURIES-pptx-60-320.jpg)