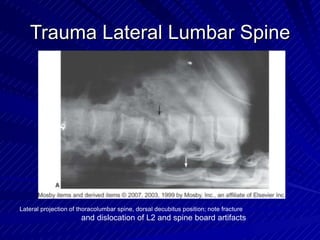
Trauma radiography involves specialized procedures to image patients with traumatic injuries. Trauma centers are classified by level depending on available resources and specialties. Level I centers have the most comprehensive services available 24/7. Radiographers in emergency departments must be prepared to perform a variety of trauma imaging procedures on patients of all ages using specialized equipment. Common trauma projections include lateral cervical spine, cervicothoracic, and thoracic and lumbar spine views. Quality, speed, accuracy and attention to detail are important principles for optimal trauma radiography.