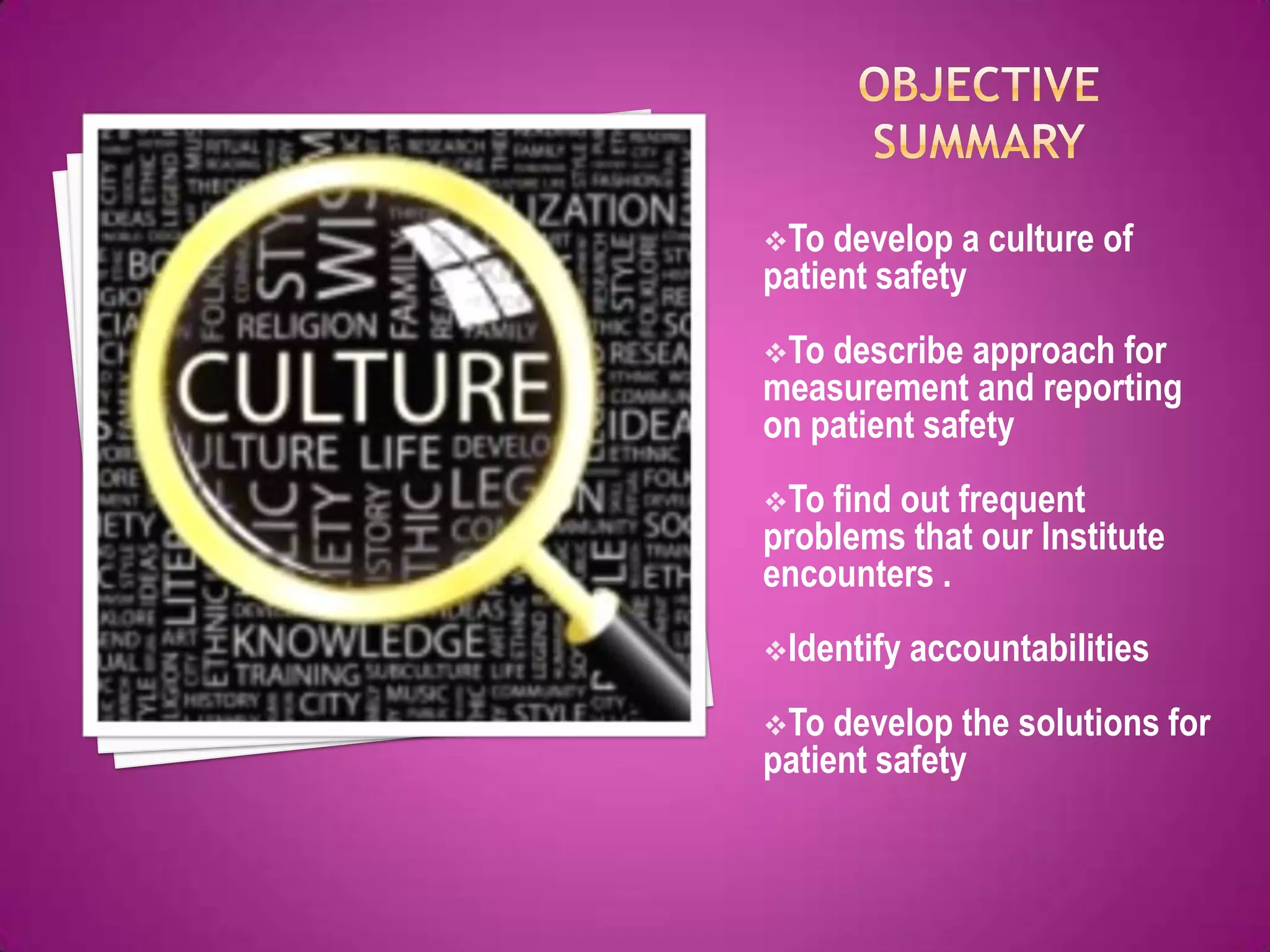
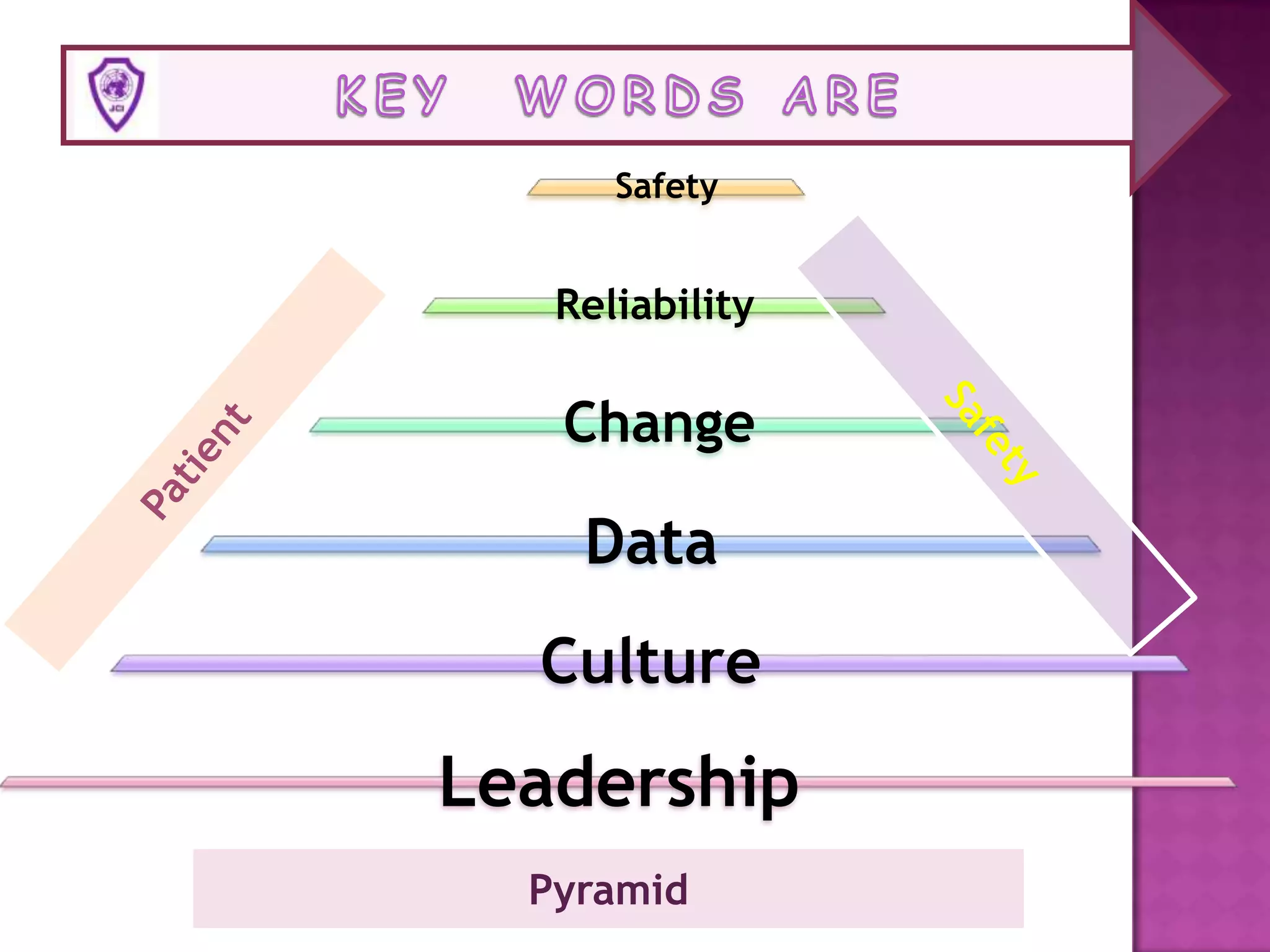
The presentation will last 25 minutes followed by a 5 minute question and answer session. The presentation will discuss establishing a safety culture at the hospital by overseeing various aspects of safety including patient safety, employee safety, radiation safety, environmental safety, and disaster management. It will review incident reports and analyze staff injuries to identify issues and promote a culture of reporting near misses. The presentation will also discuss risk management programs in hospitals and identify common safety issues like patient identification, medication safety, healthcare-associated infections, and falls. [END SUMMARY]