1) Mammography is an x-ray exam used to detect breast changes, with modern machines using low doses of radiation.
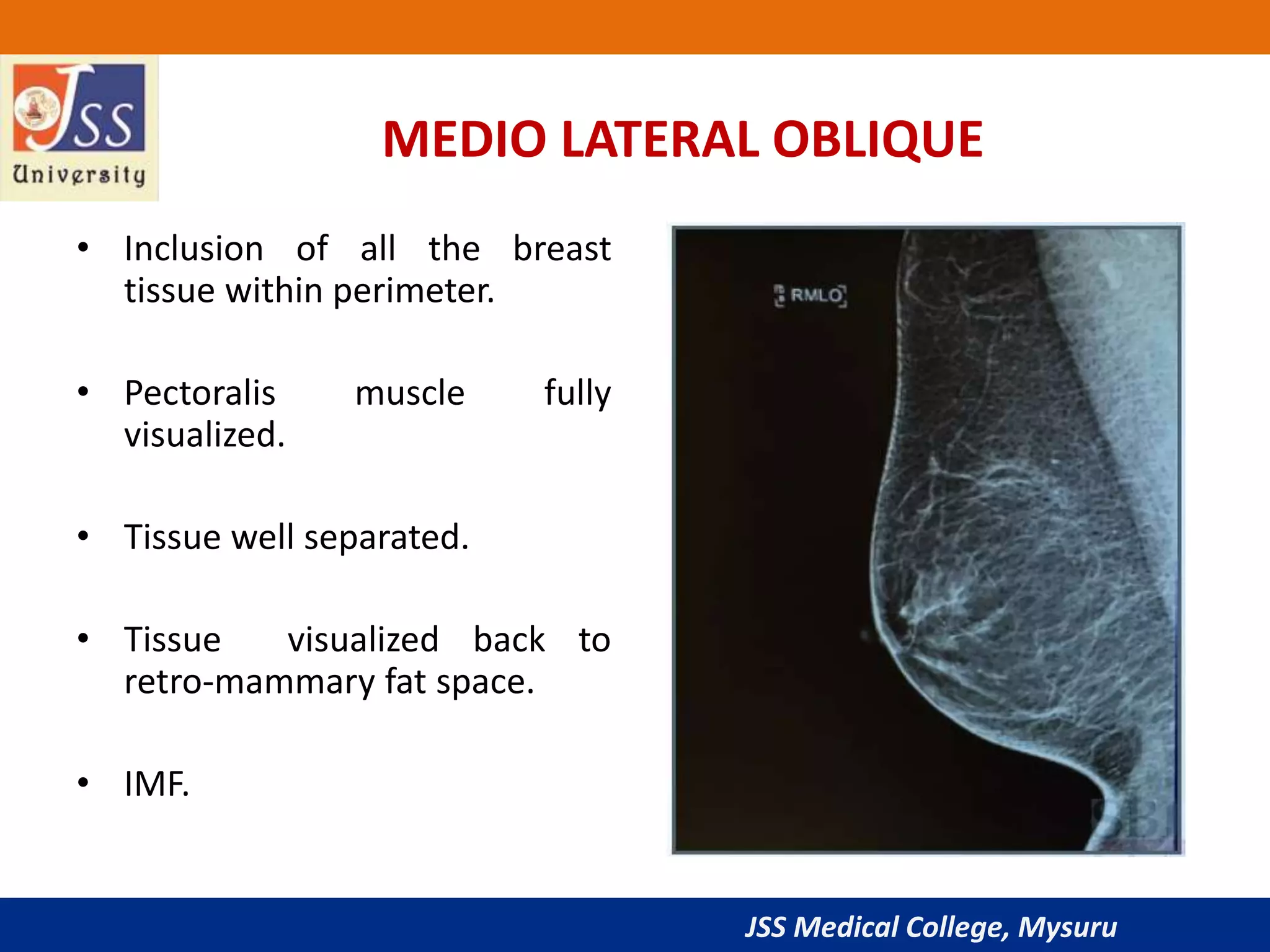
2) The document discusses mammography techniques, including standard craniocaudal and mediolateral oblique views as well as additional views.
3) Contraindications and recommendations for screening are provided based on risk factors and age. The document provides an overview of mammography procedures and guidelines.