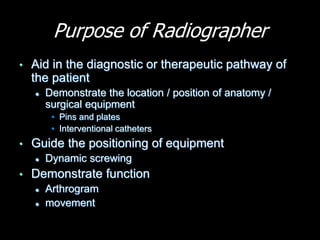
The document discusses the role and responsibilities of a radiographer in the operating theatre. It outlines the key tasks of preparing equipment, ensuring patient details are entered correctly, and using protective equipment. The radiographer aids surgical procedures by producing diagnostic images to visualize anatomy and equipment placement. Key responsibilities include minimizing radiation dose, maintaining sterilization, effective communication with the surgical team, and working collaboratively to improve imaging techniques.