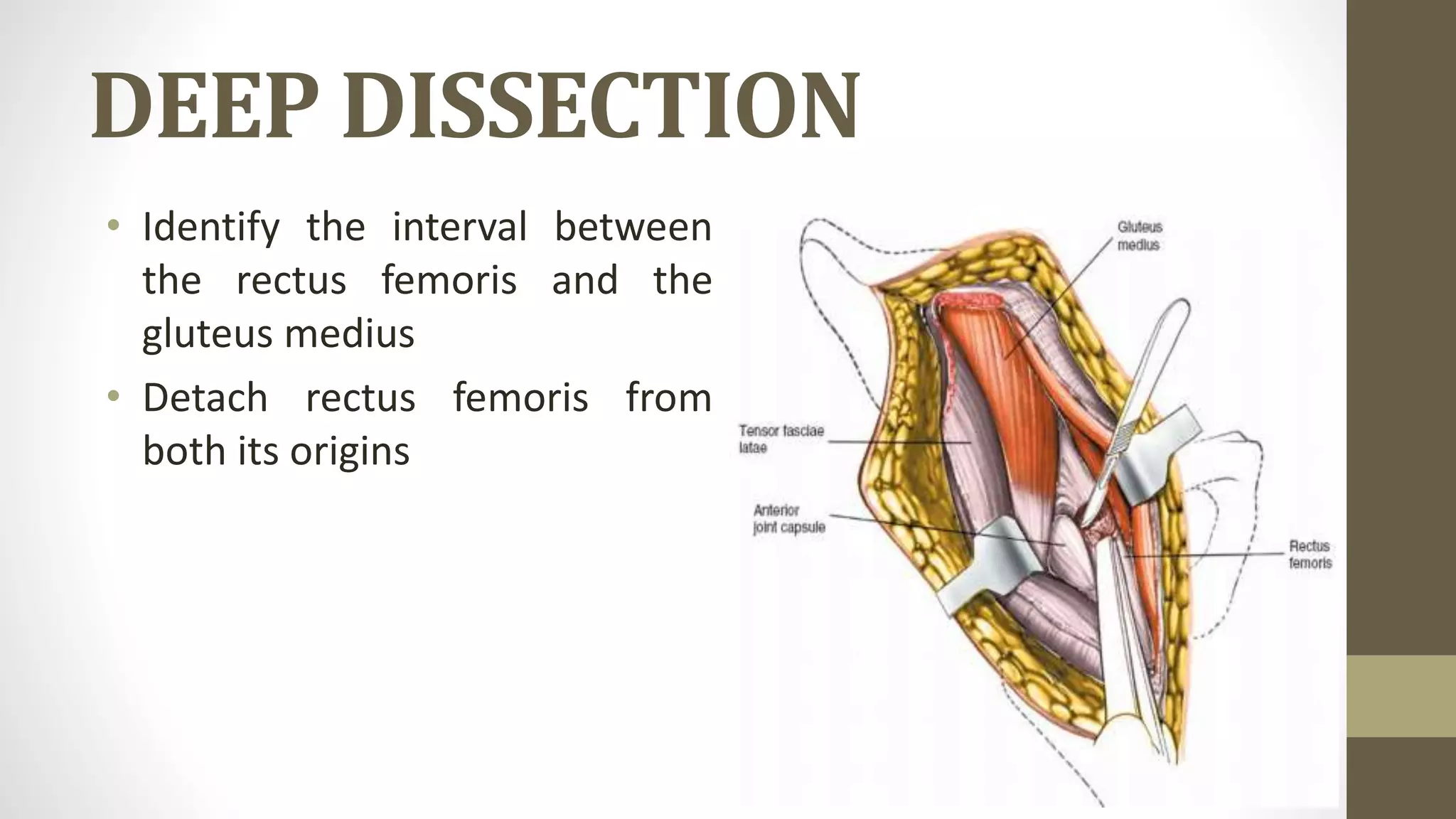
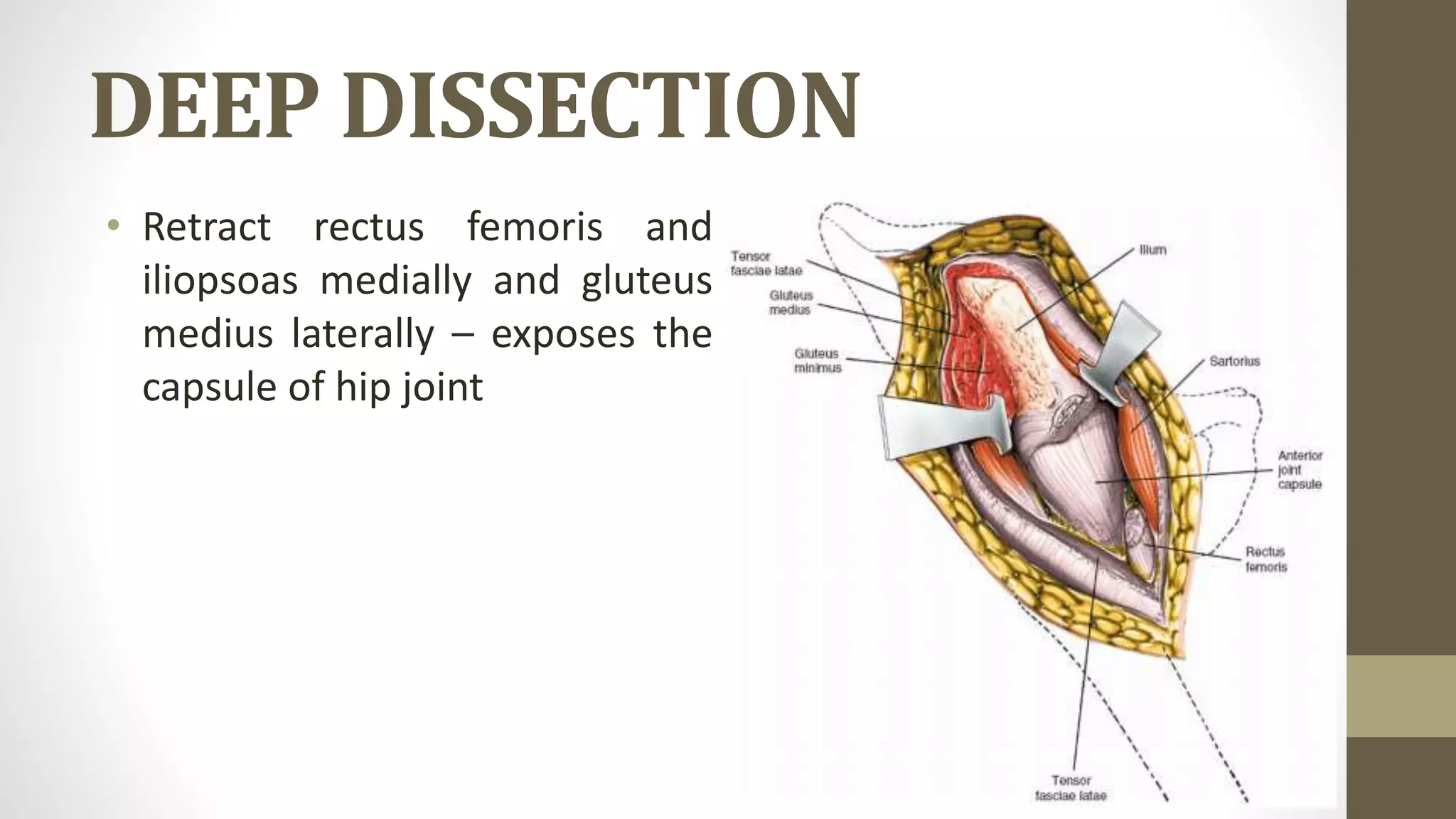
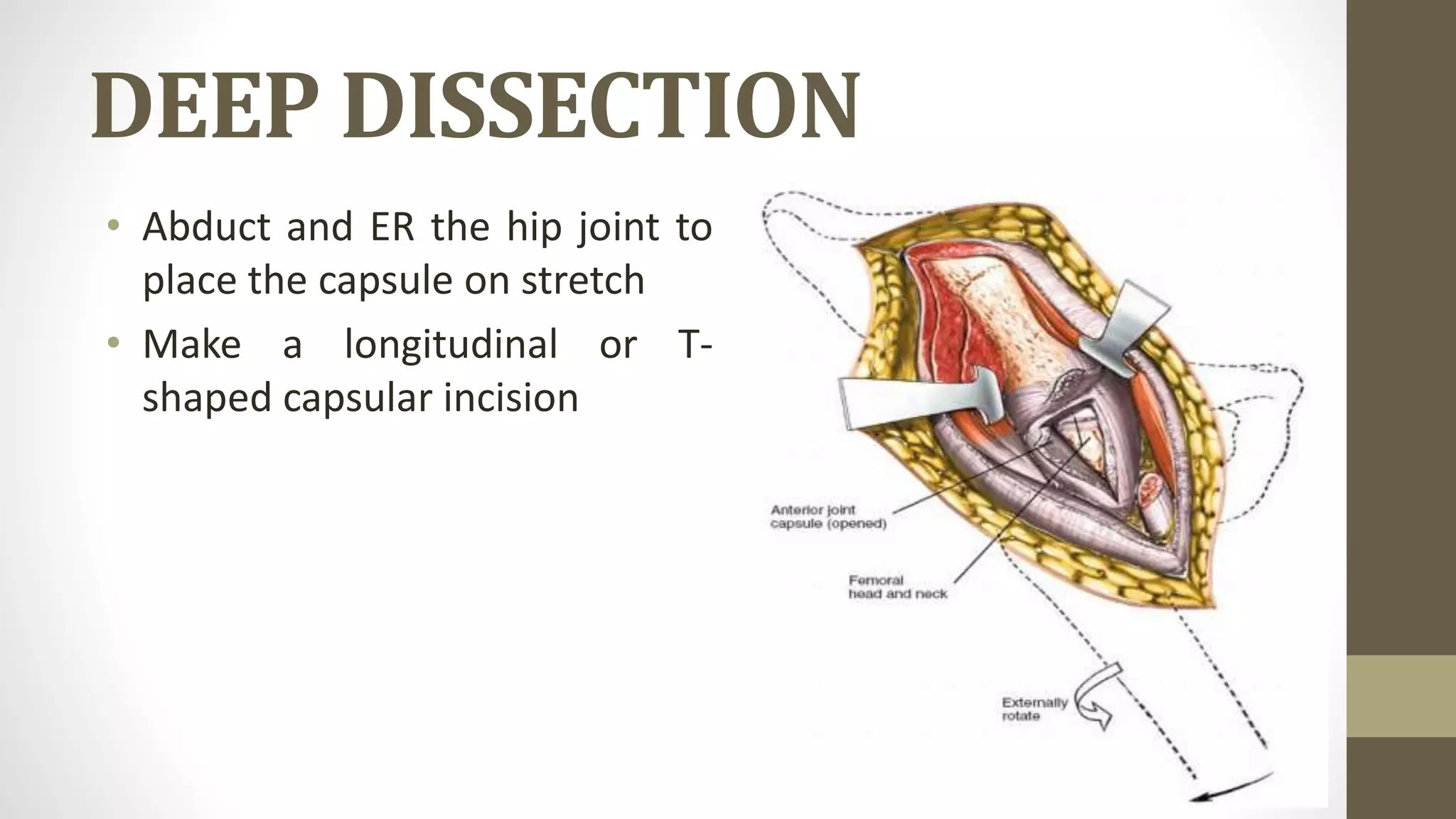
The anterior approach to the hip provides access to the hip joint and ilium through an incision along the anterior half of the iliac crest down to the ASIS, developing the internervous plane between the sartorius and TFL superficially and between the rectus femoris and gluteus medius deeply to expose the hip joint capsule for procedures like THA, pelvic osteotomies, and tumor excisions while avoiding injury to the lateral femoral cutaneous nerve and ligating branches of the lateral femoral circumflex artery.