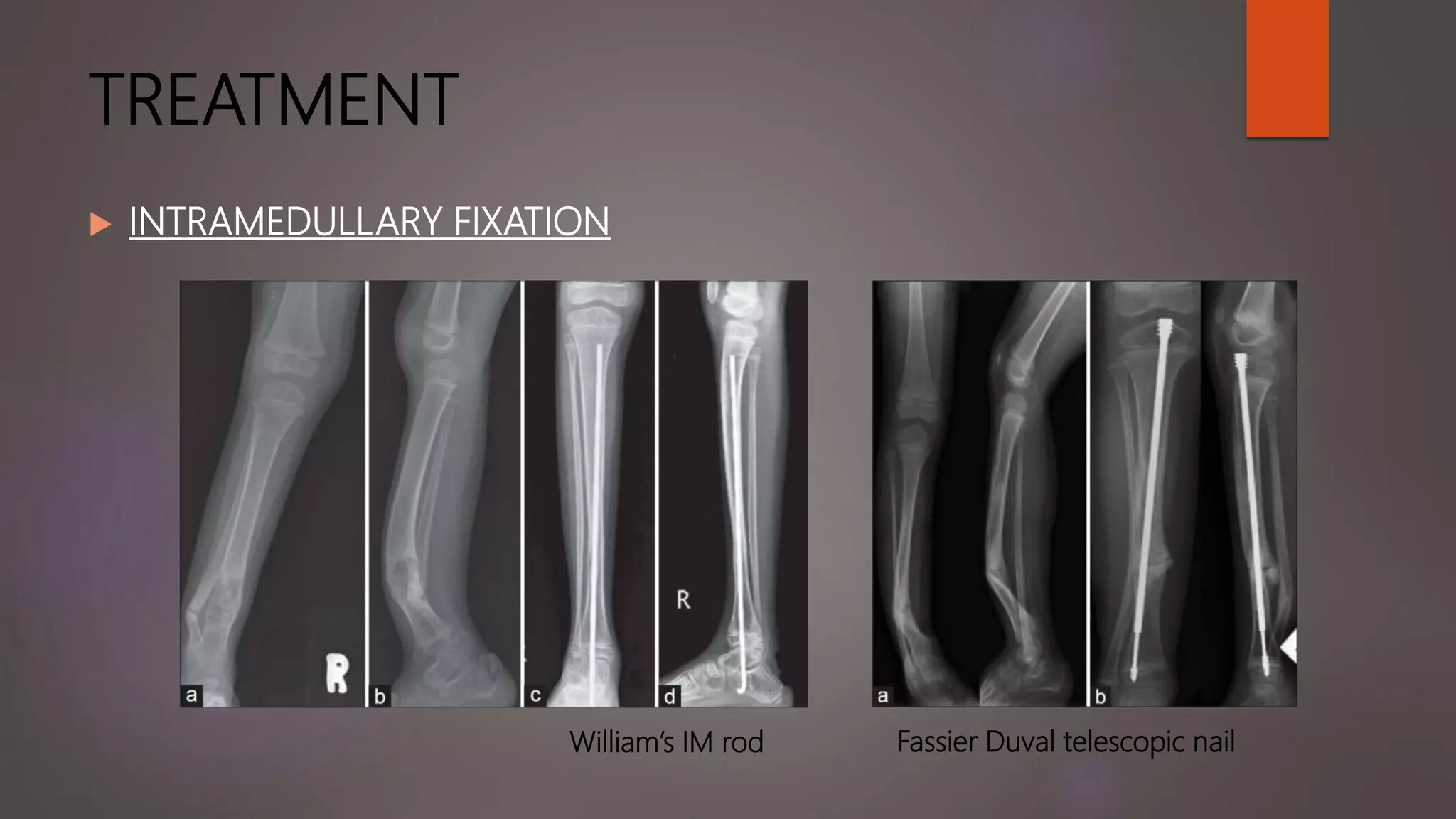
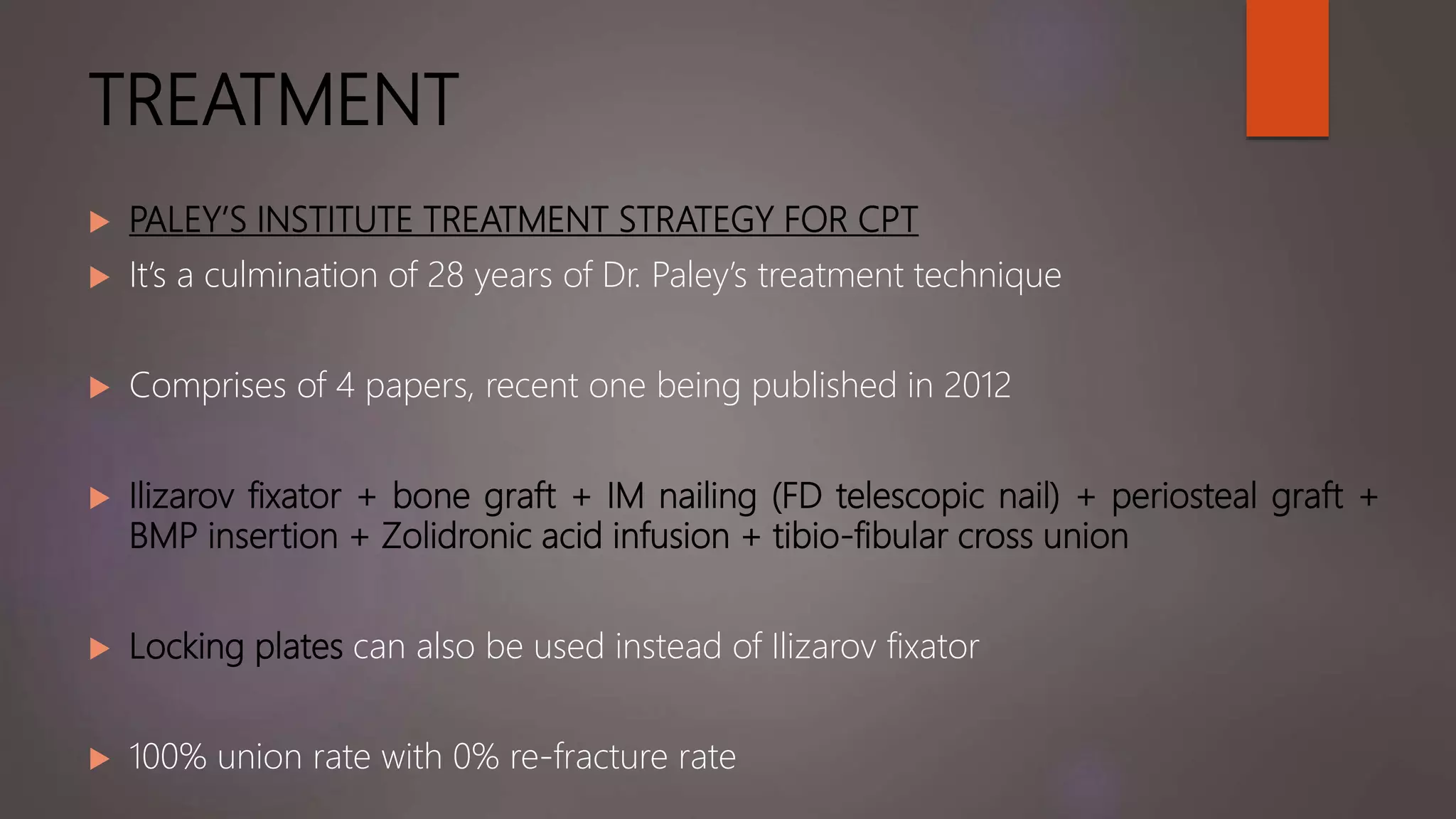
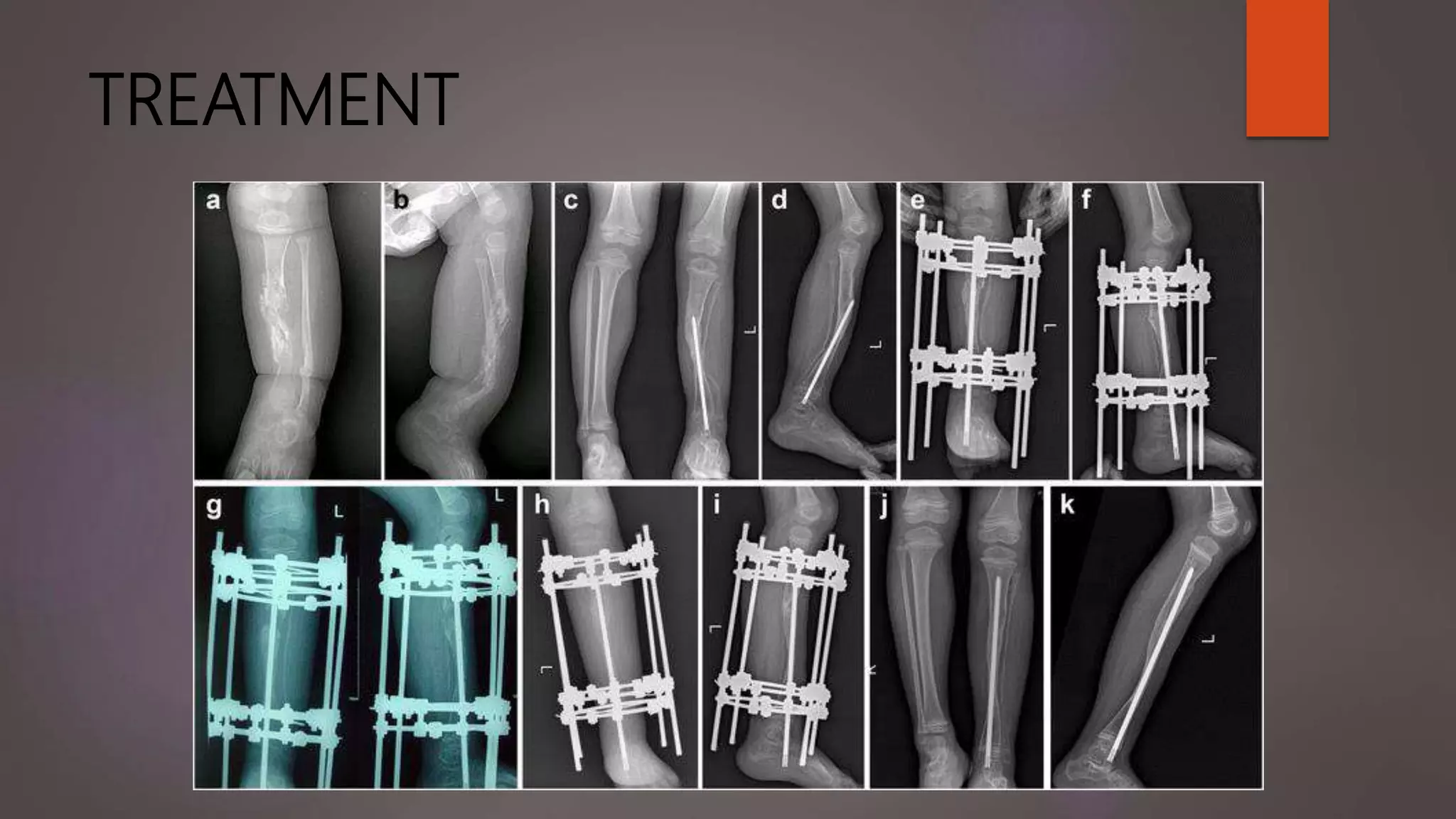
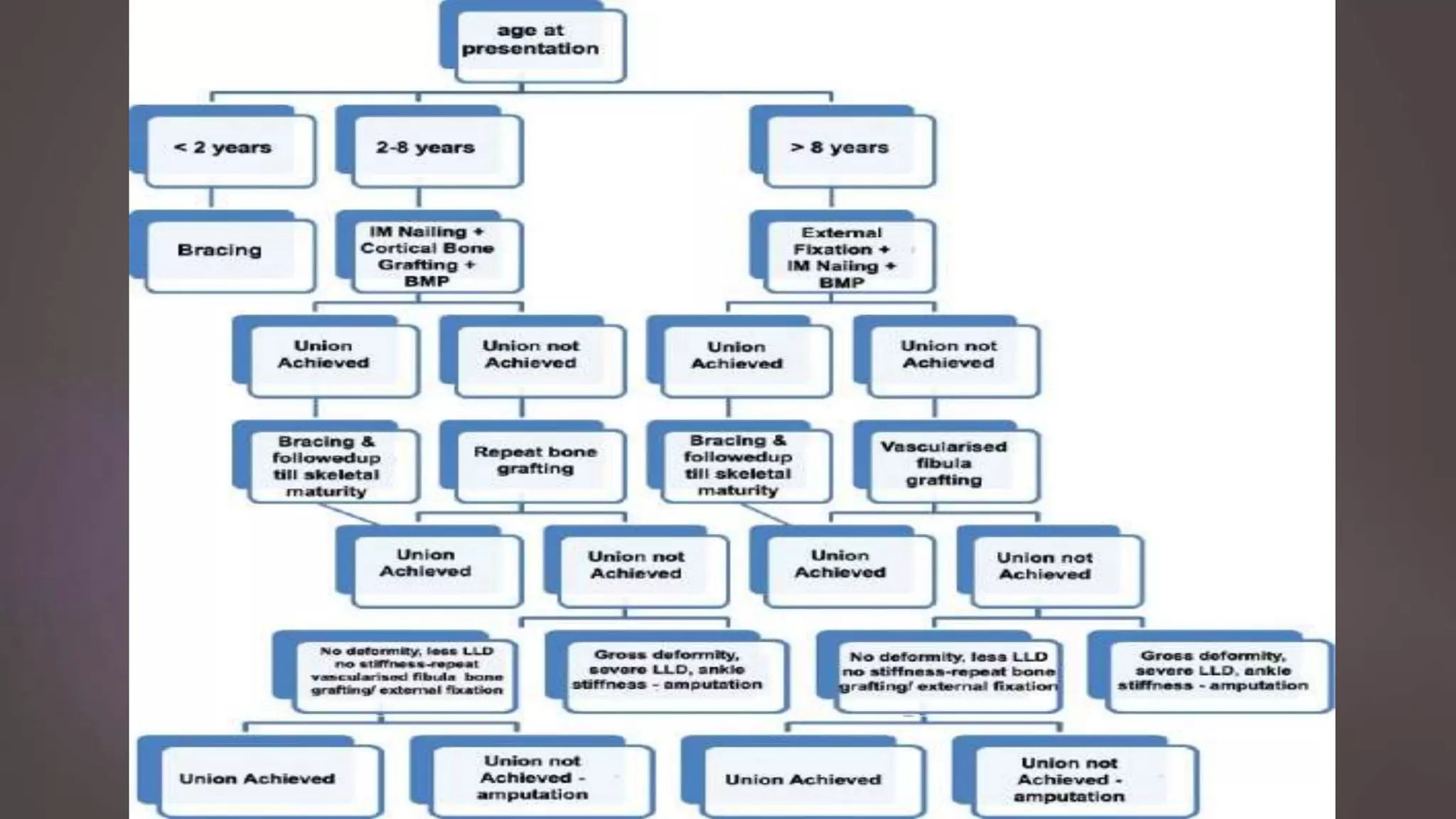
Congenital pseudarthrosis of the tibia is a rare birth defect involving a non-union of the tibia that occurs spontaneously or after minor trauma, usually within the first 2 years of life. It is often associated with neurofibromatosis. Surgical treatment involves resection of the pseudarthrosis and surrounding tissue, restoration of alignment, and intramedullary fixation with augmentation techniques like bone grafting or BMPs. Complications can include re-fracture, ankle deformity, and tibial shortening. Prognosis is poorer with lower age at treatment, previous failed treatment, neurofibromatosis, and increased follow up needed.