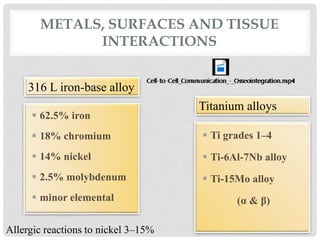
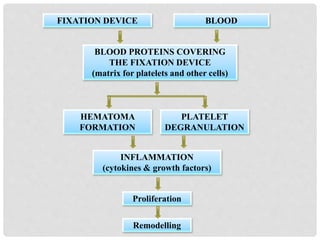
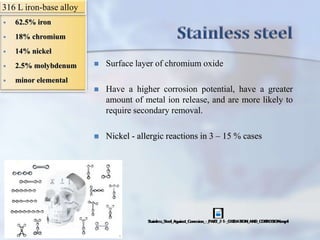
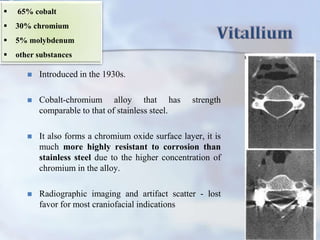
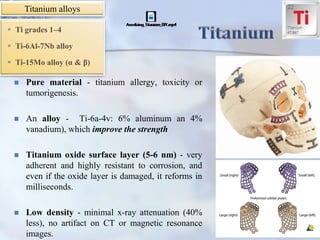
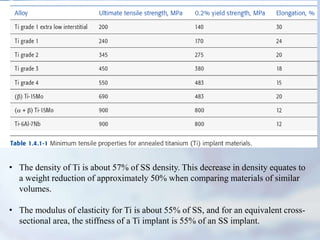
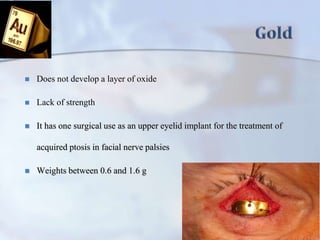
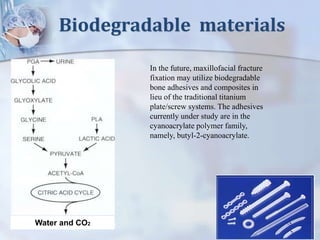
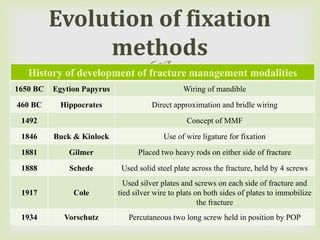
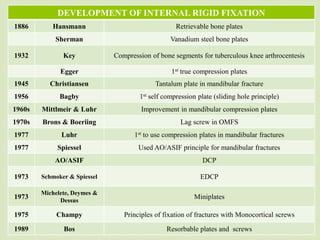
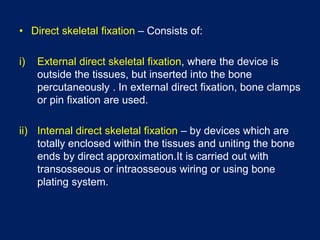
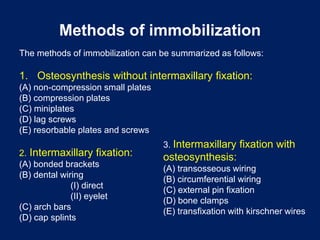
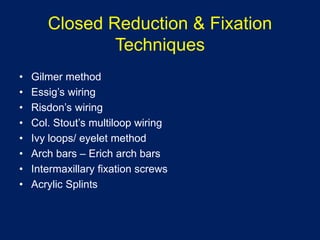
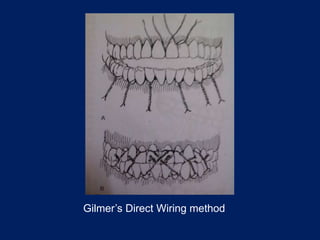
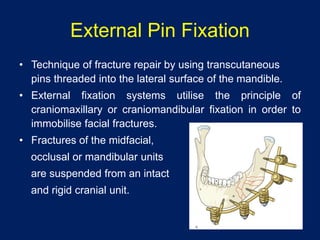
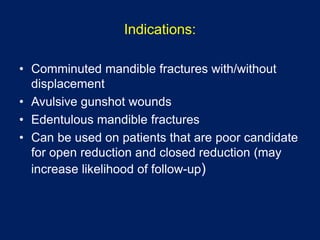
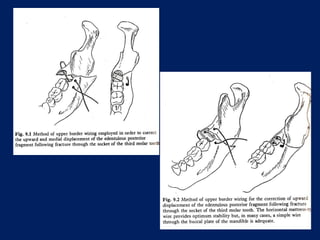
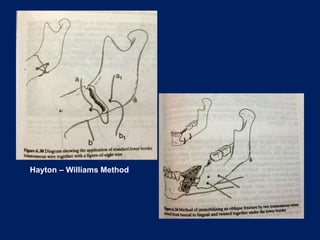
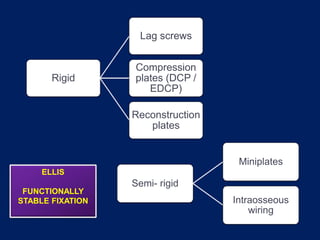
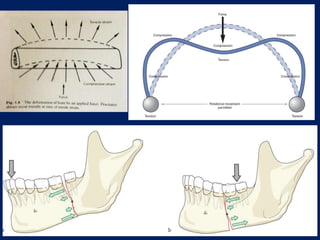
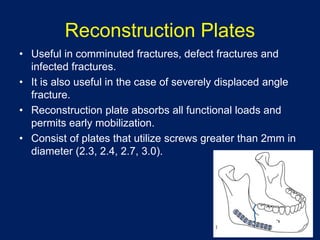
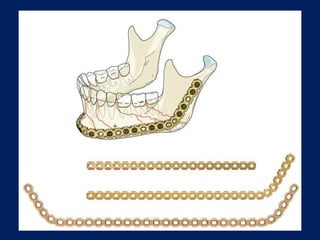
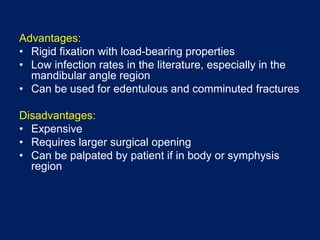
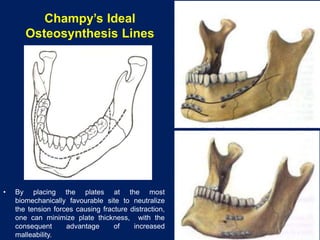
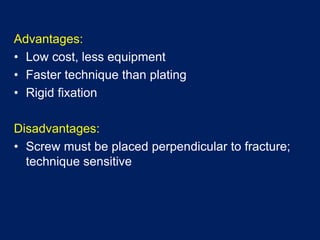
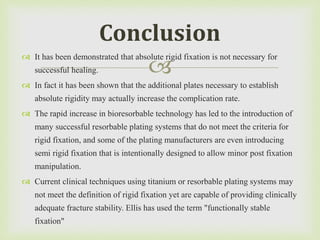
This document discusses various methods of internal fixation for maxillofacial fractures. It begins with an introduction to metallurgy and the evolution of fixation methods. Some common metals used for internal fixation like stainless steel, Vitallium, and titanium alloys are described. Various historical methods of fixation are outlined, followed by principles of rigid internal fixation using plates, screws, and wires. Both closed and open reduction techniques are summarized.