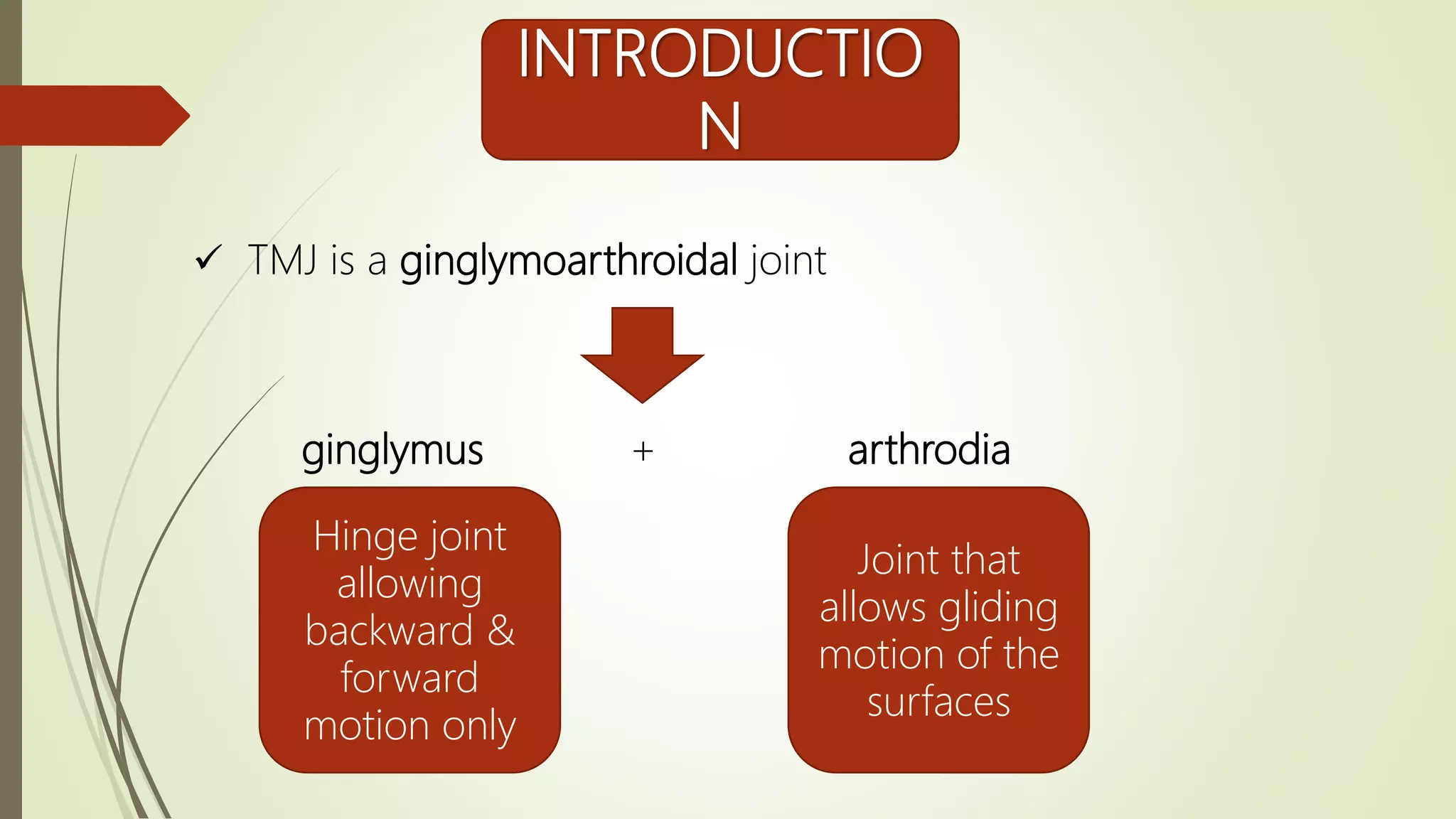
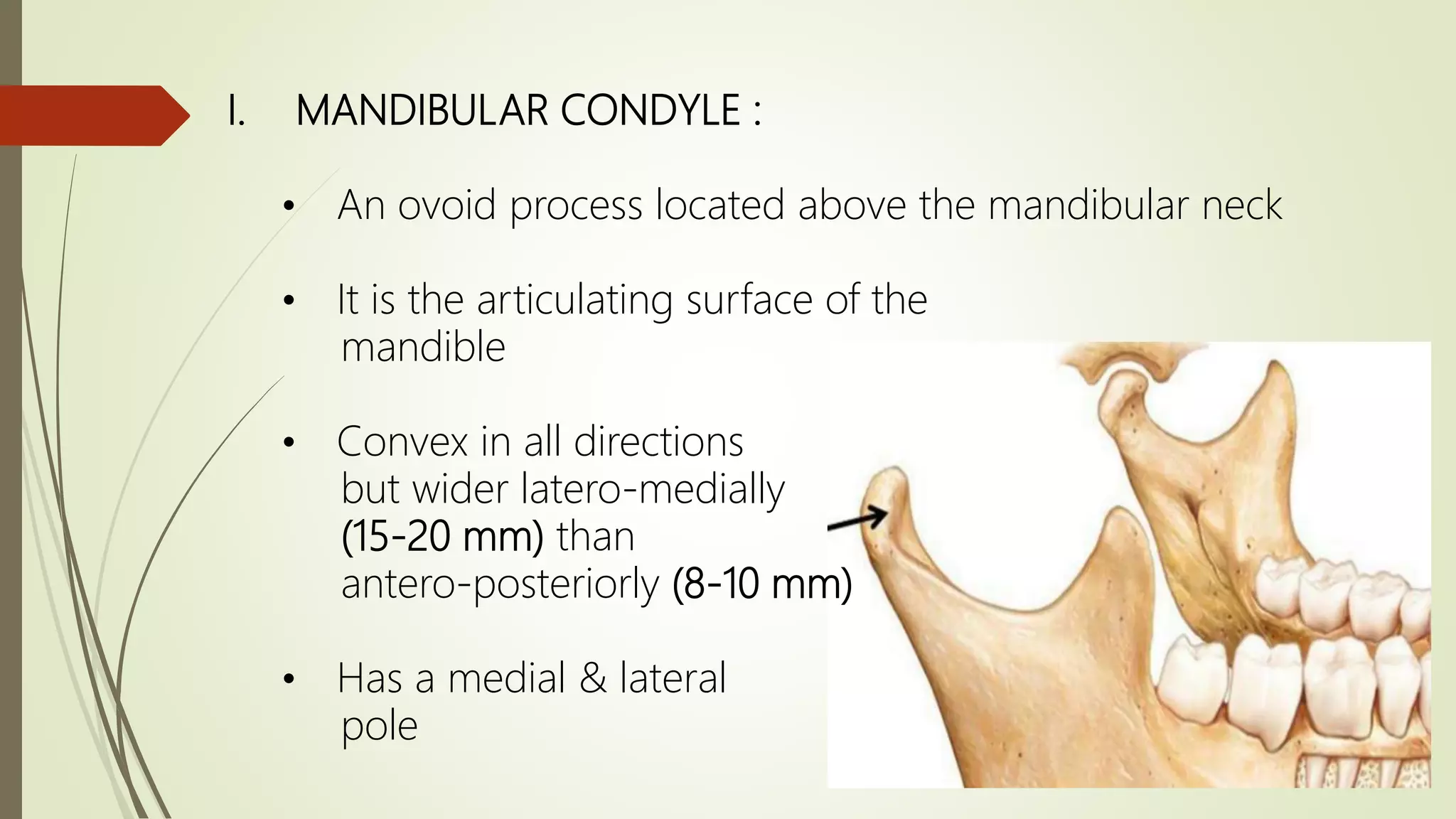
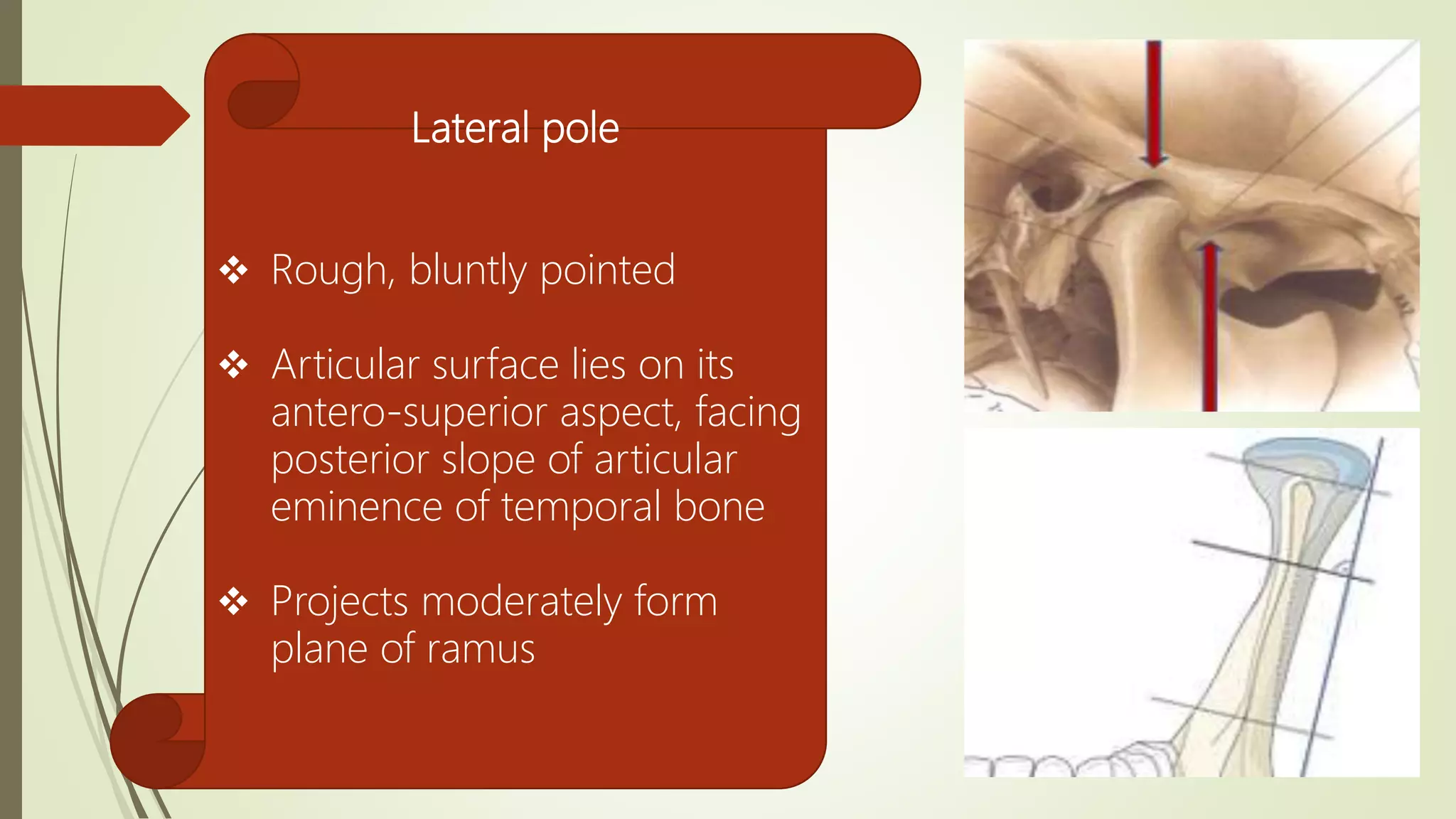
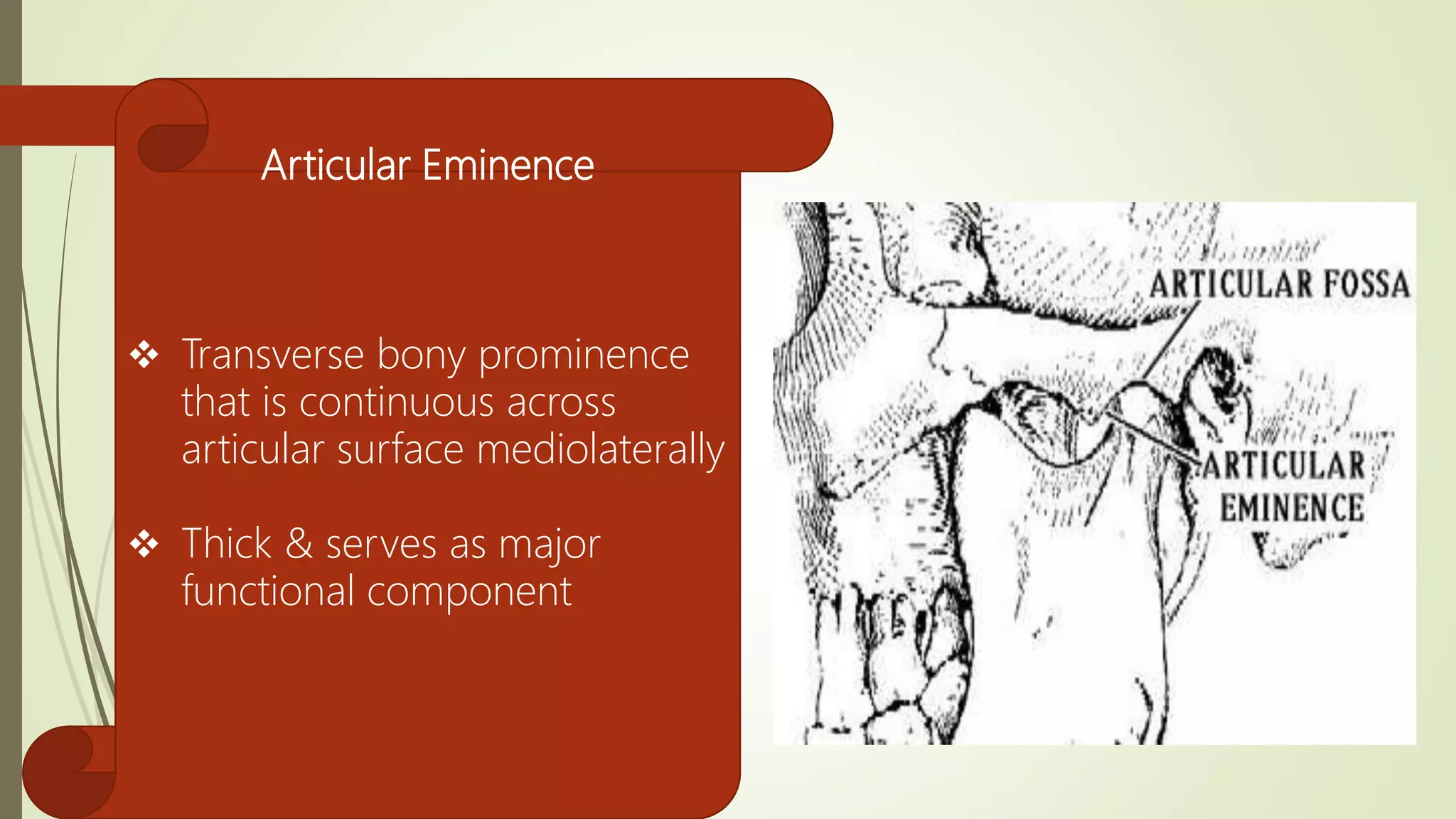
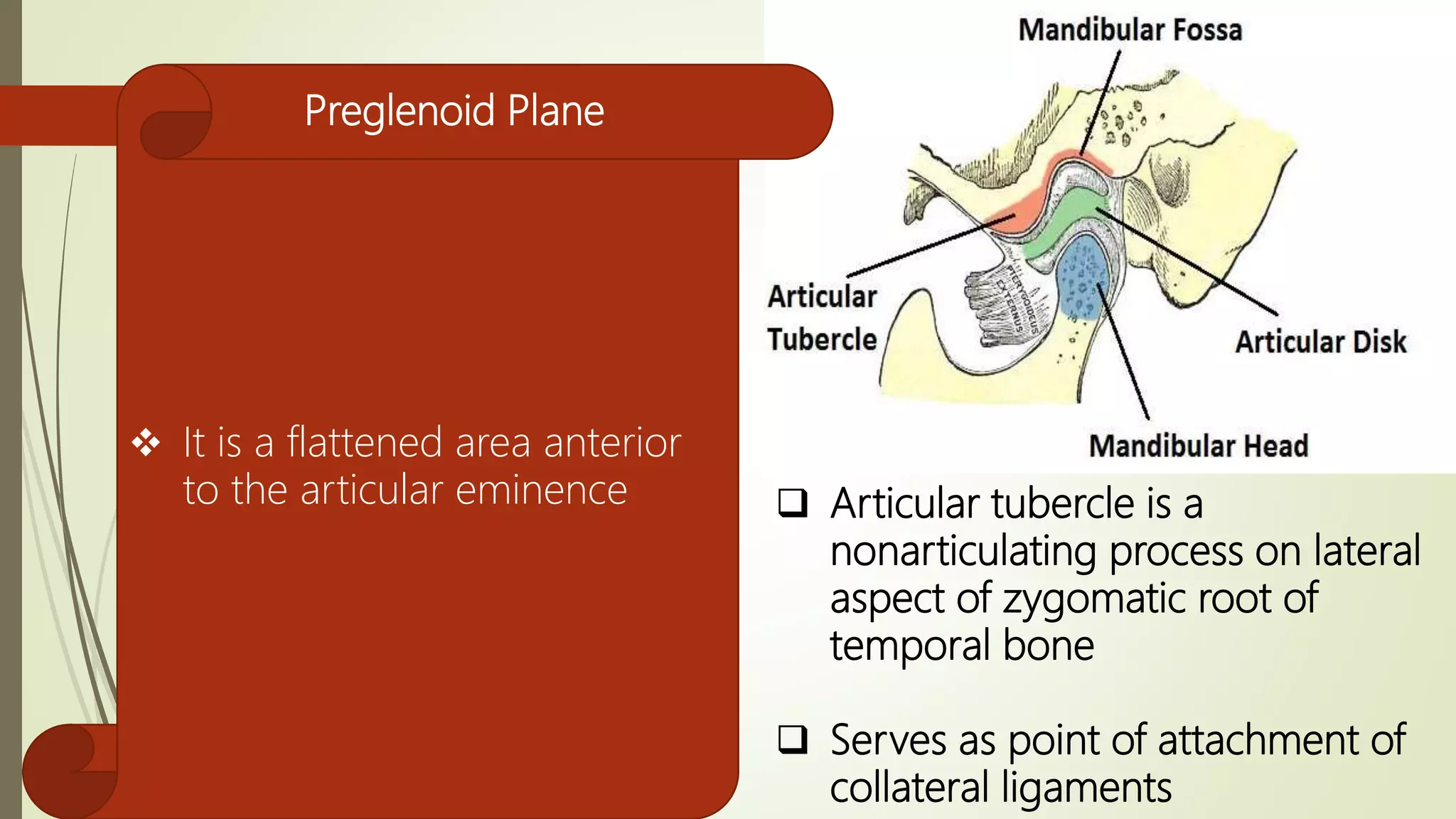
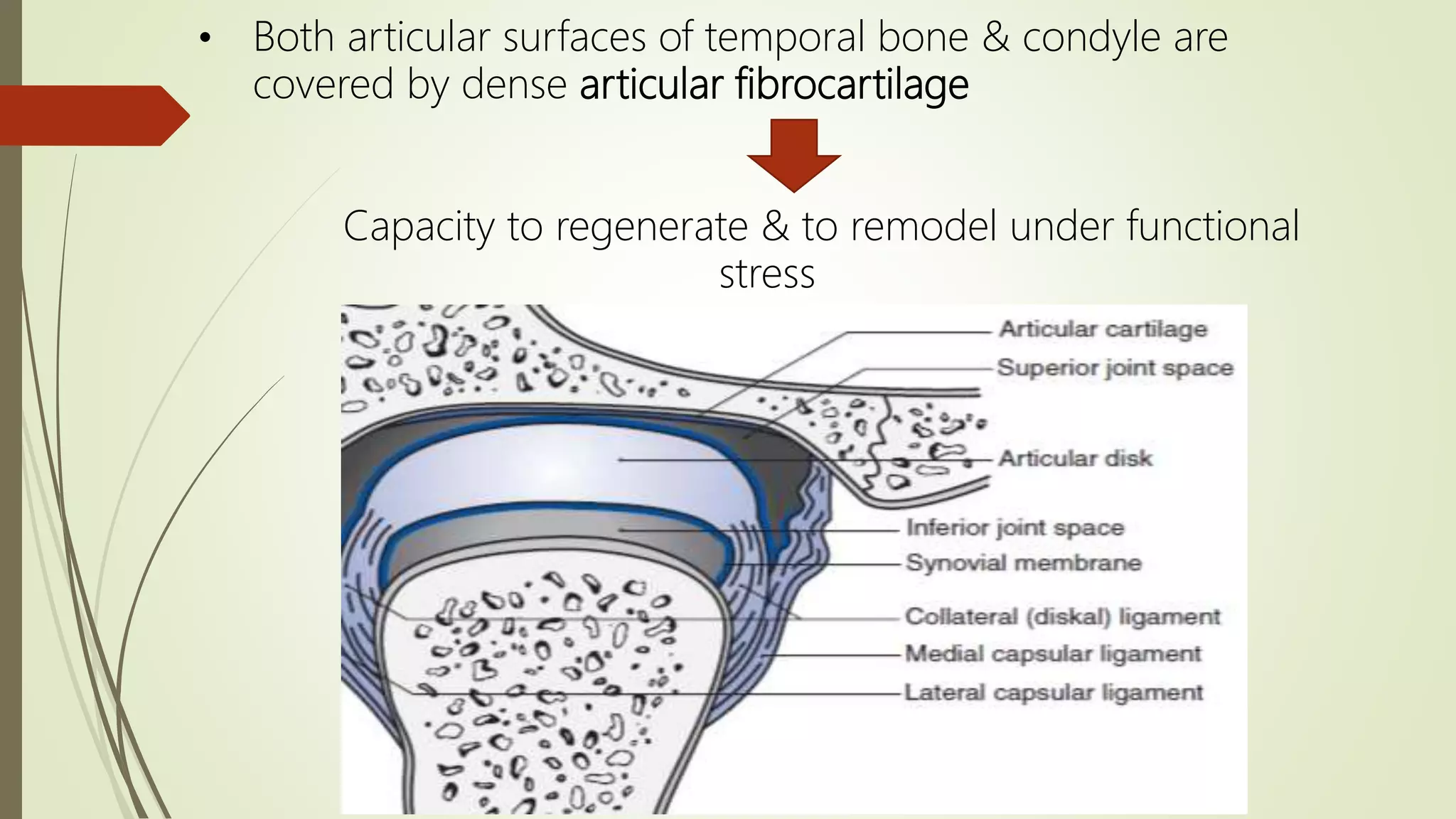
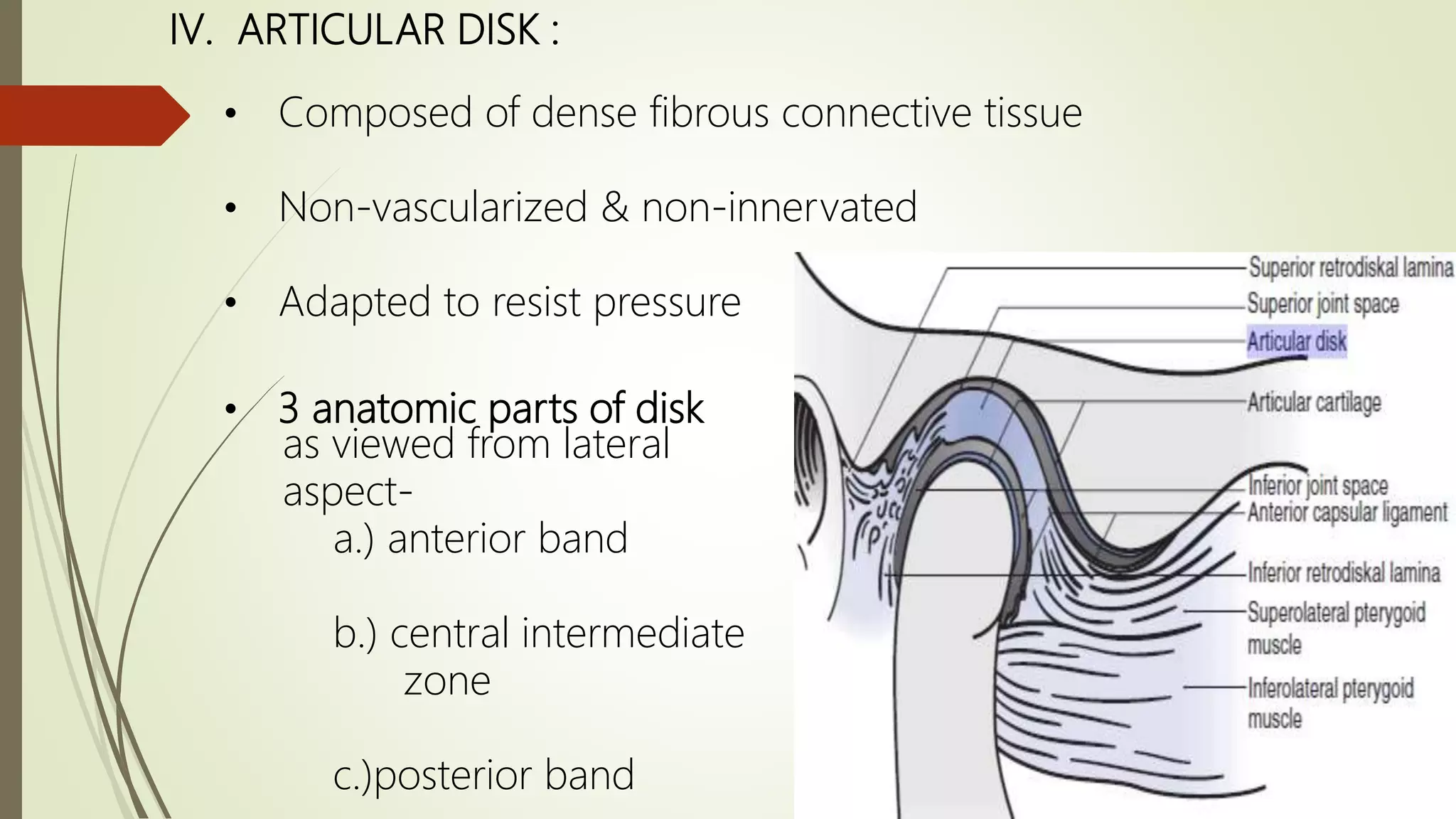
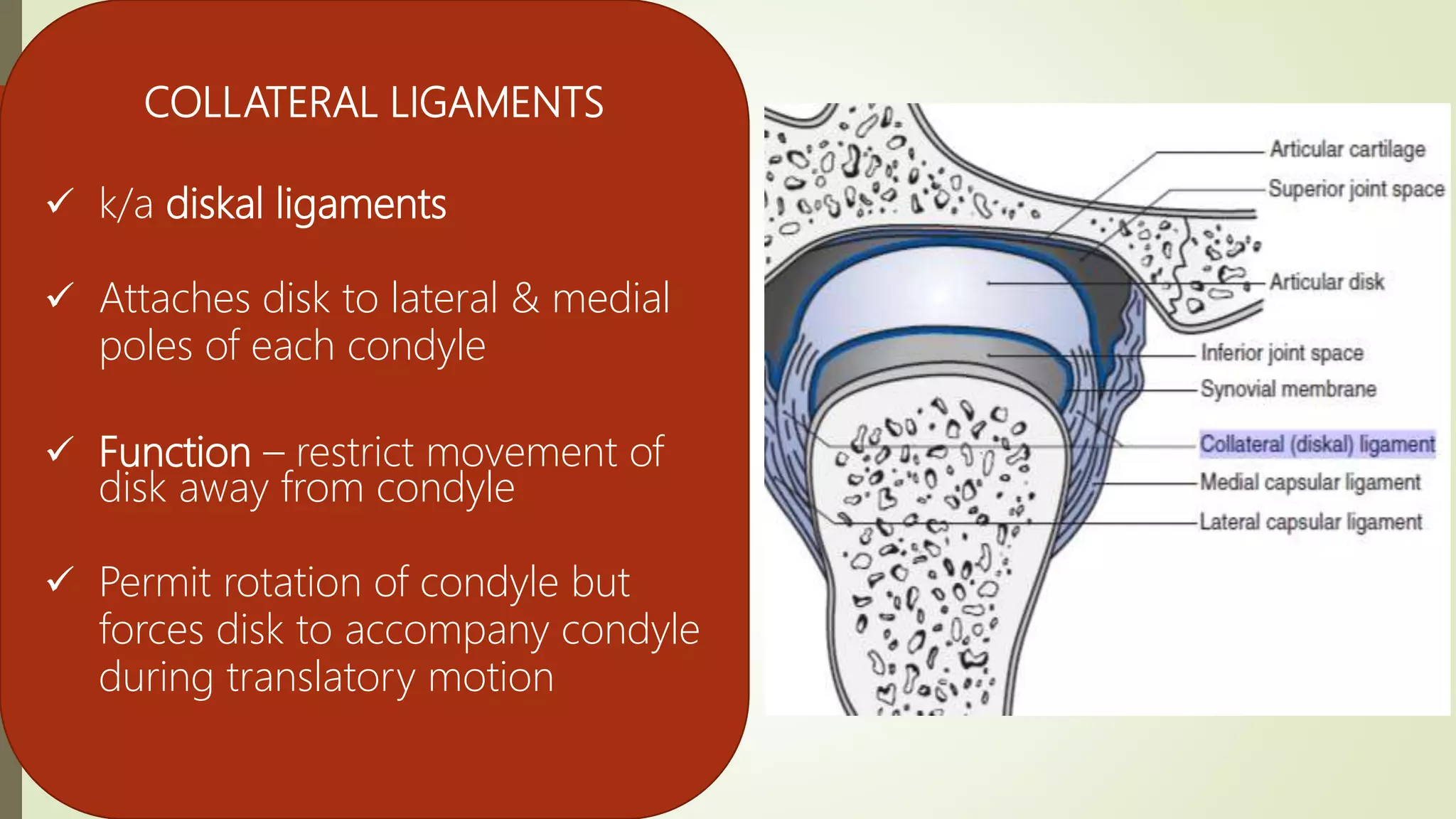
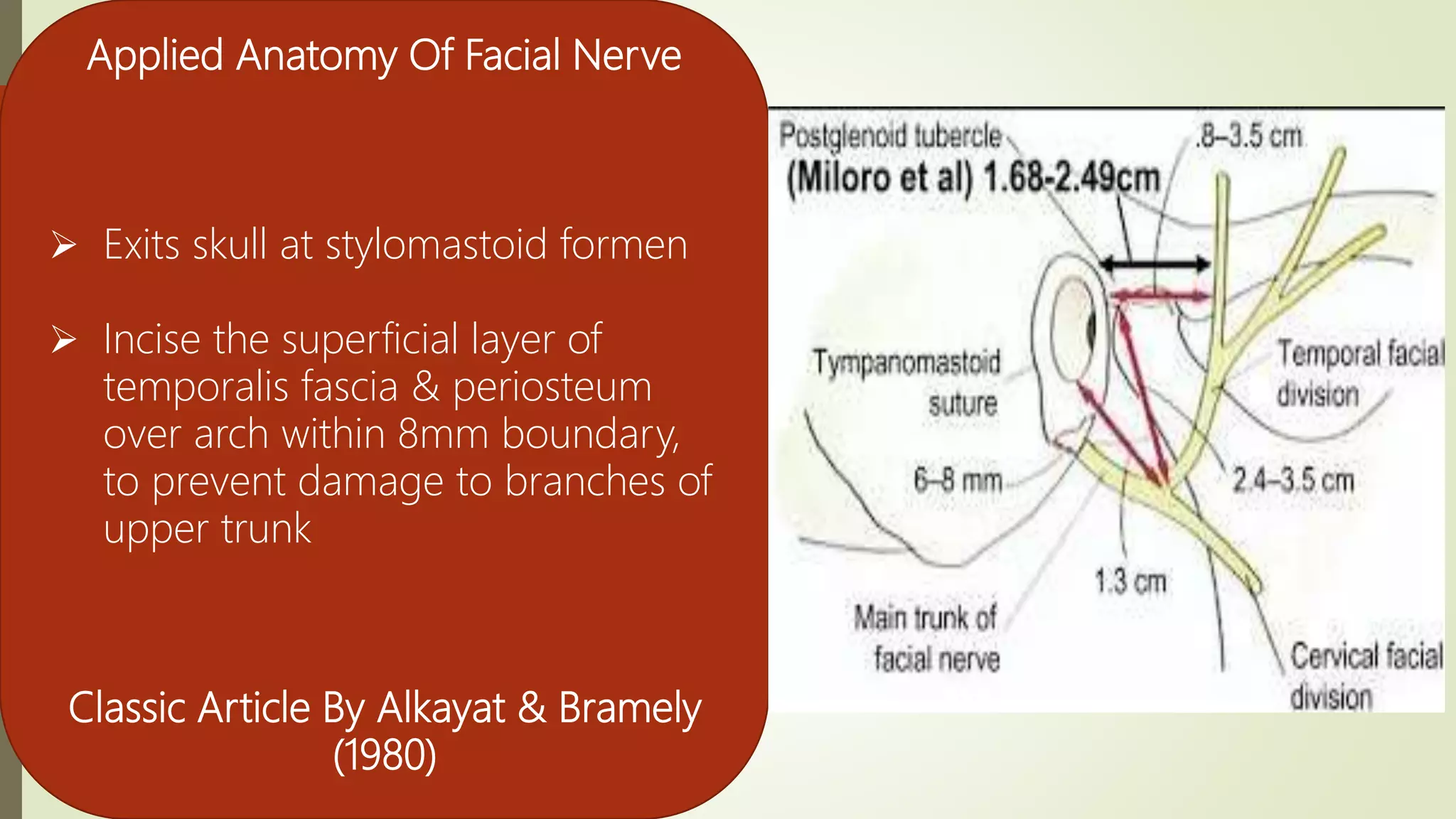
The document provides an overview of the temporomandibular joint (TMJ), detailing its unique features, components, and significance in maxillofacial surgery. It highlights the joint's structure, functions, and various surgical approaches to address TMJ issues. Additionally, it emphasizes the importance of understanding TMJ anatomy for successful surgical interventions.