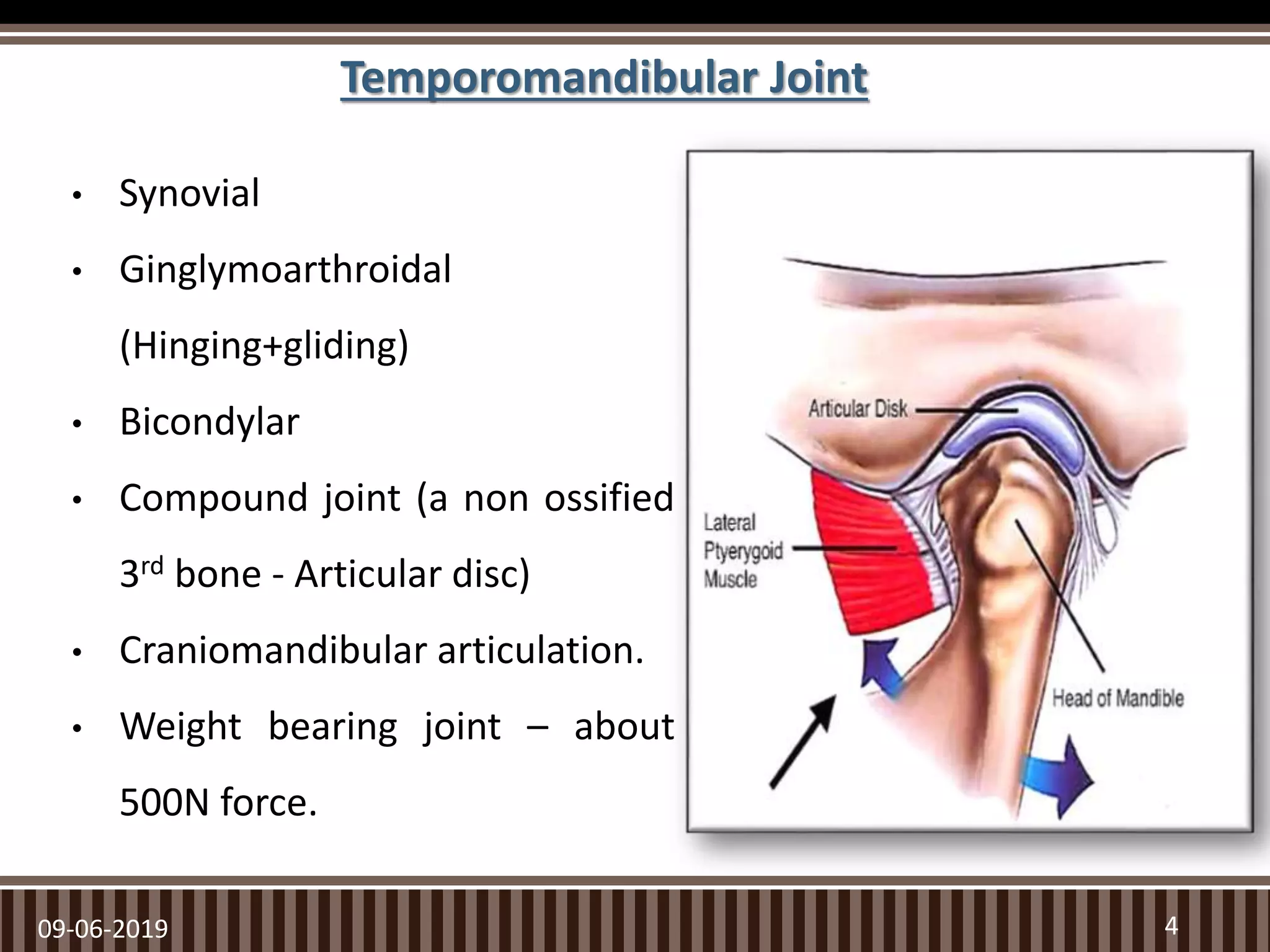
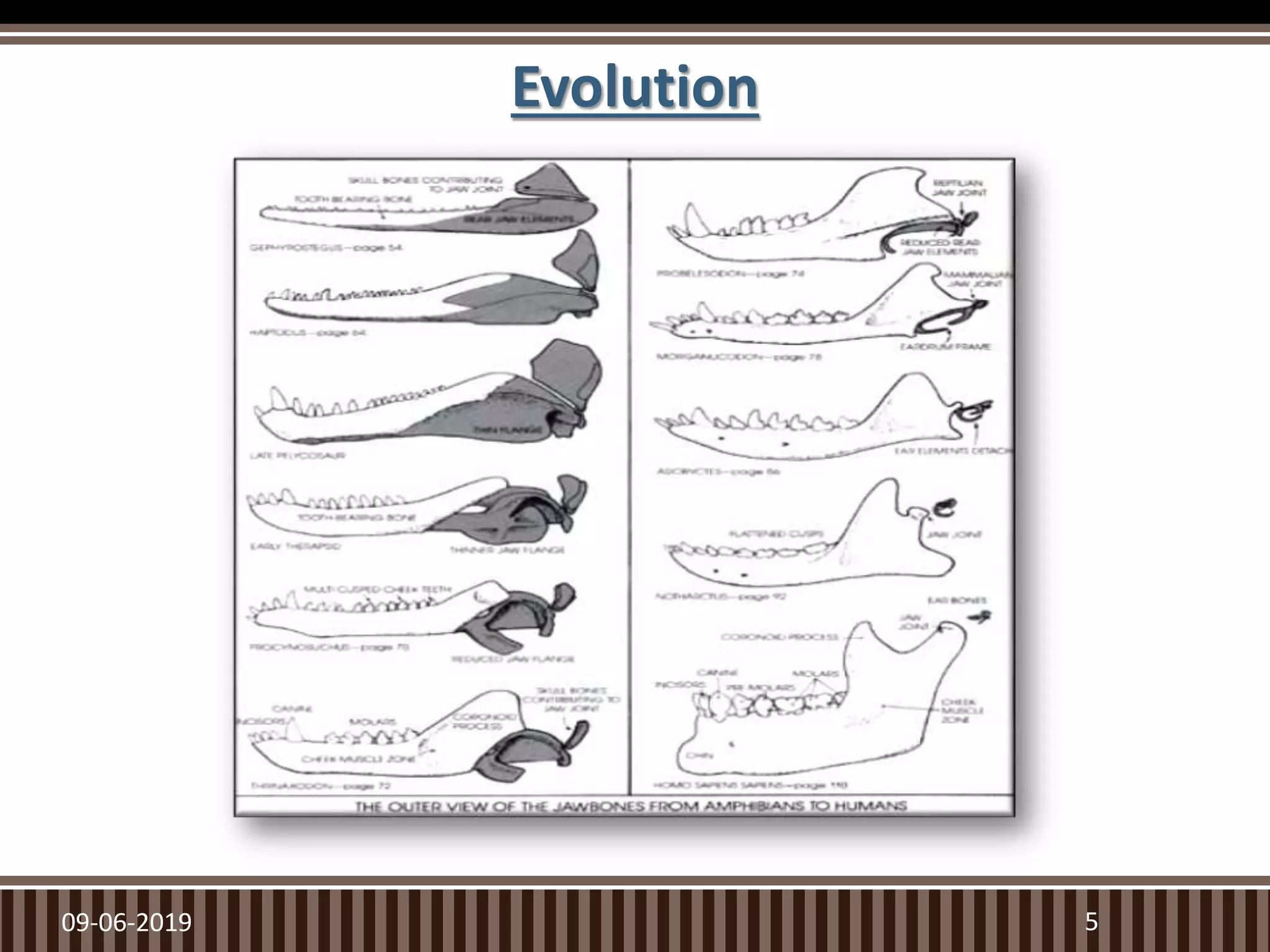
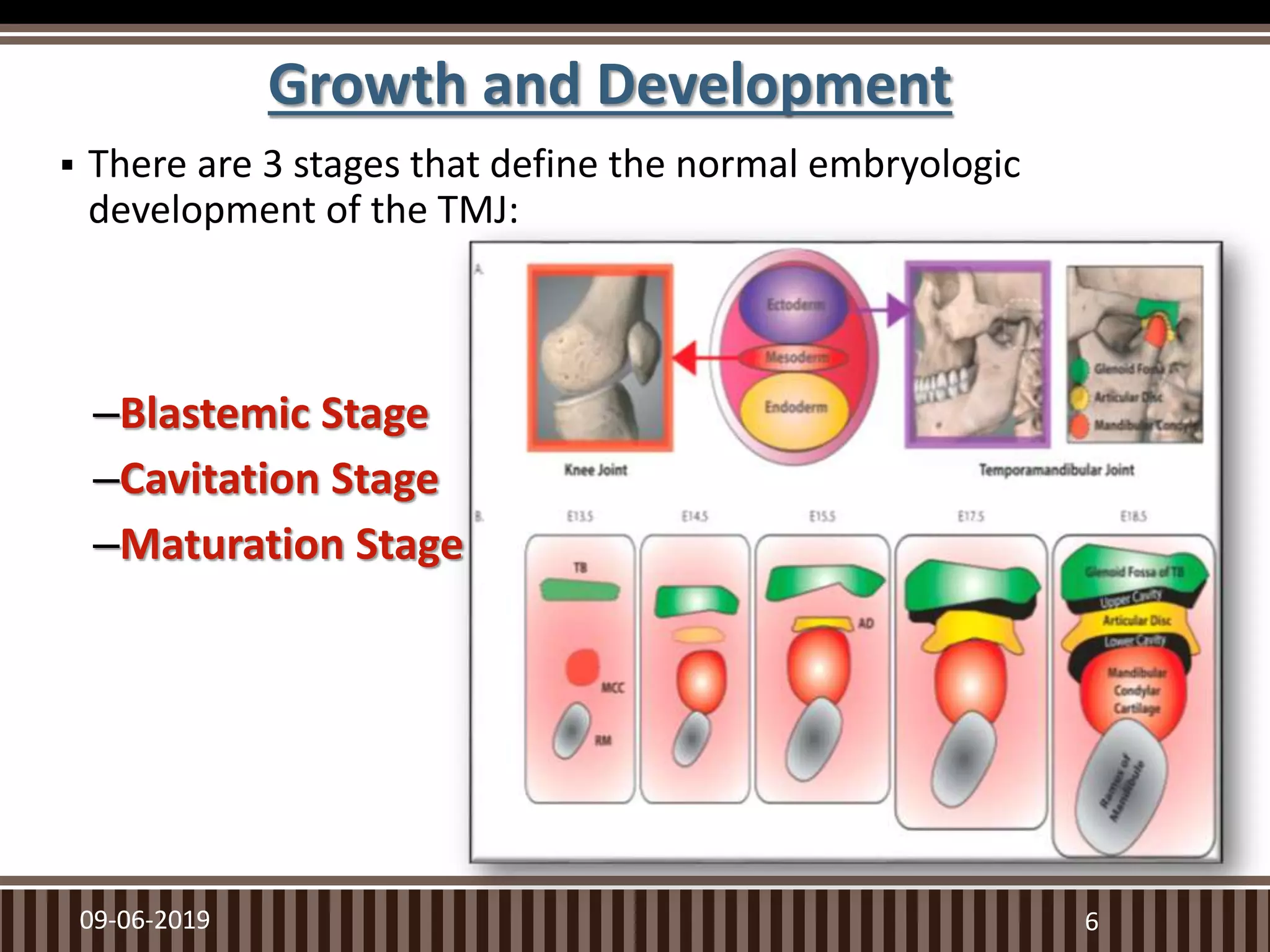
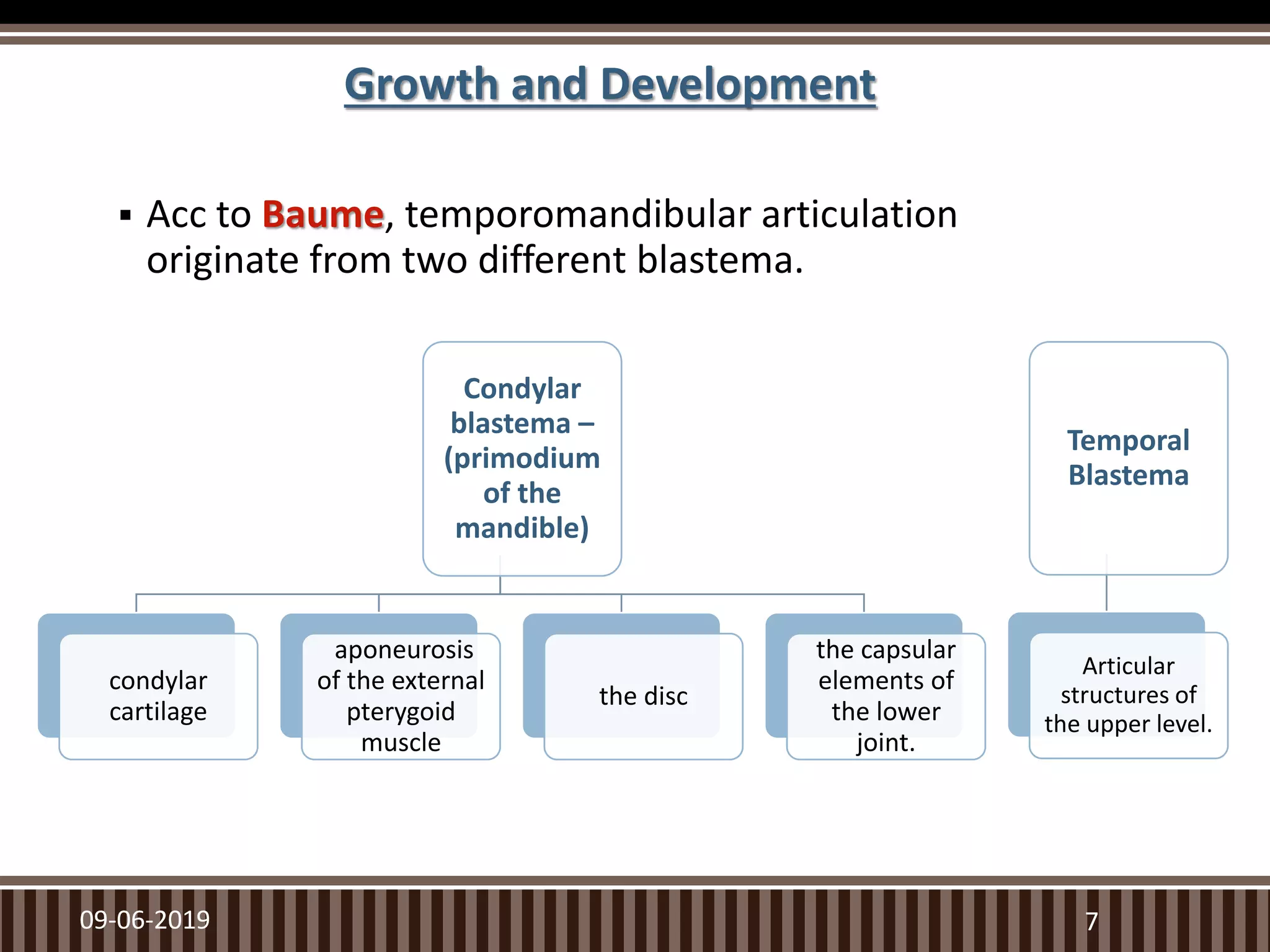
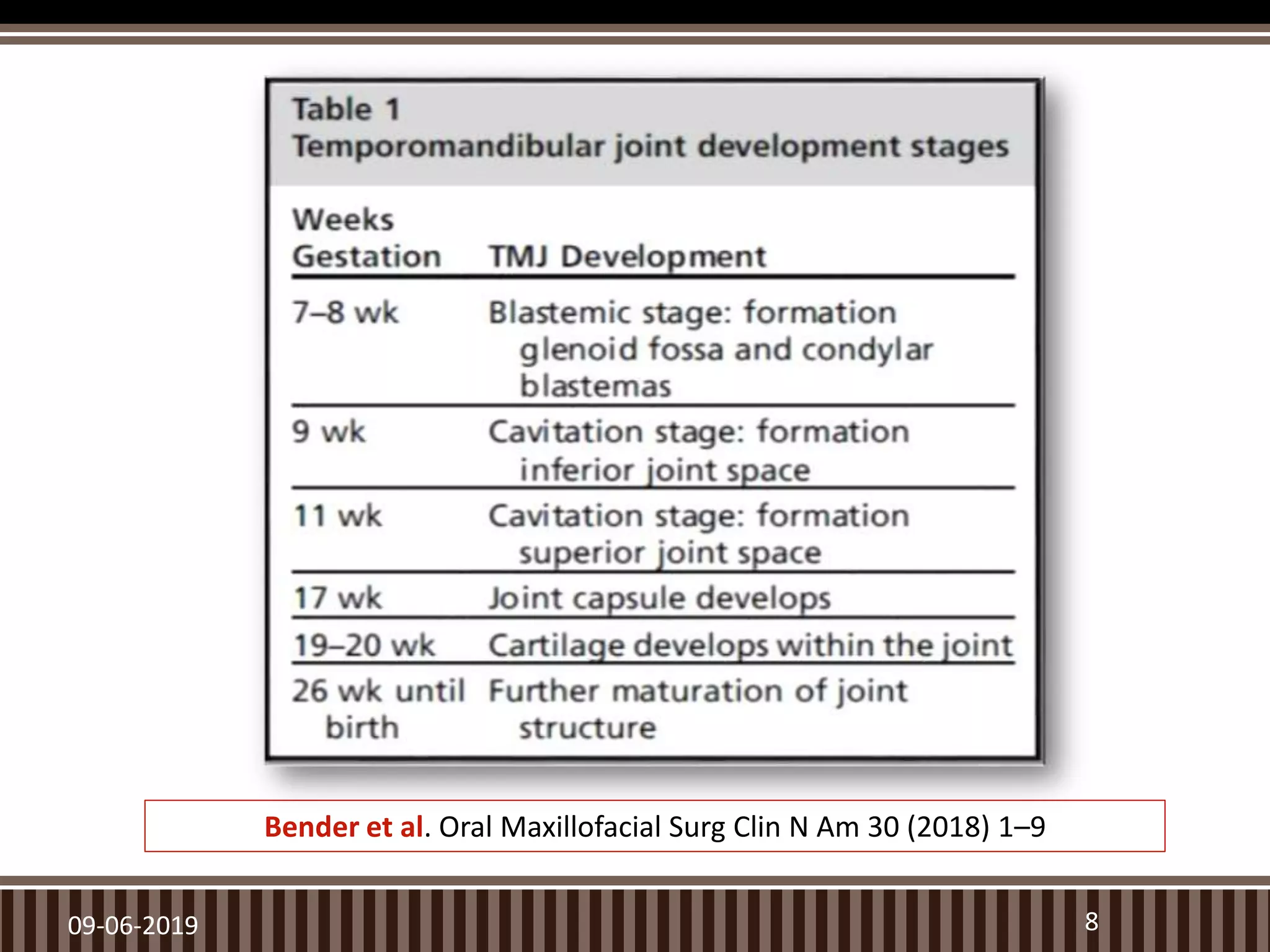
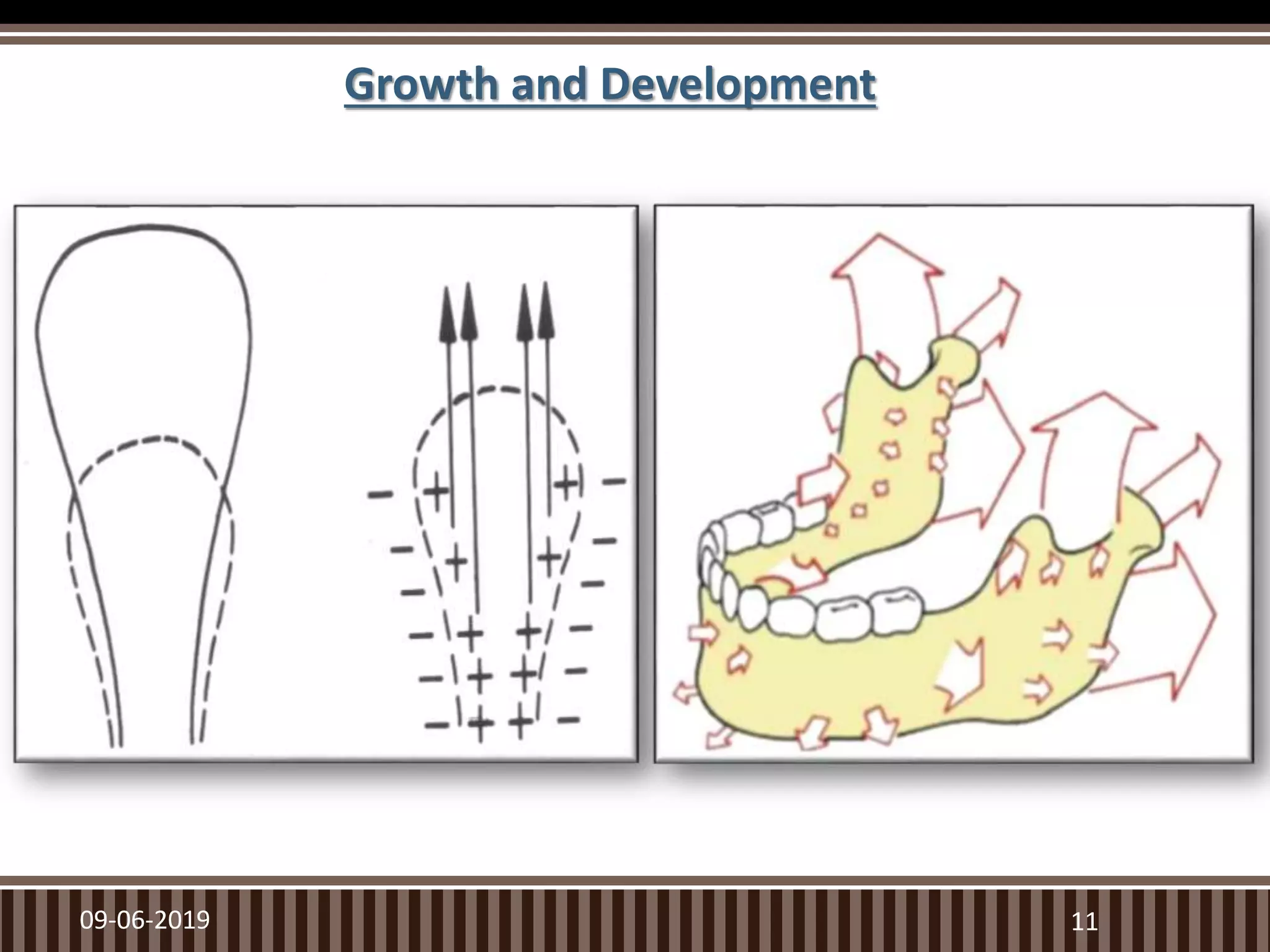
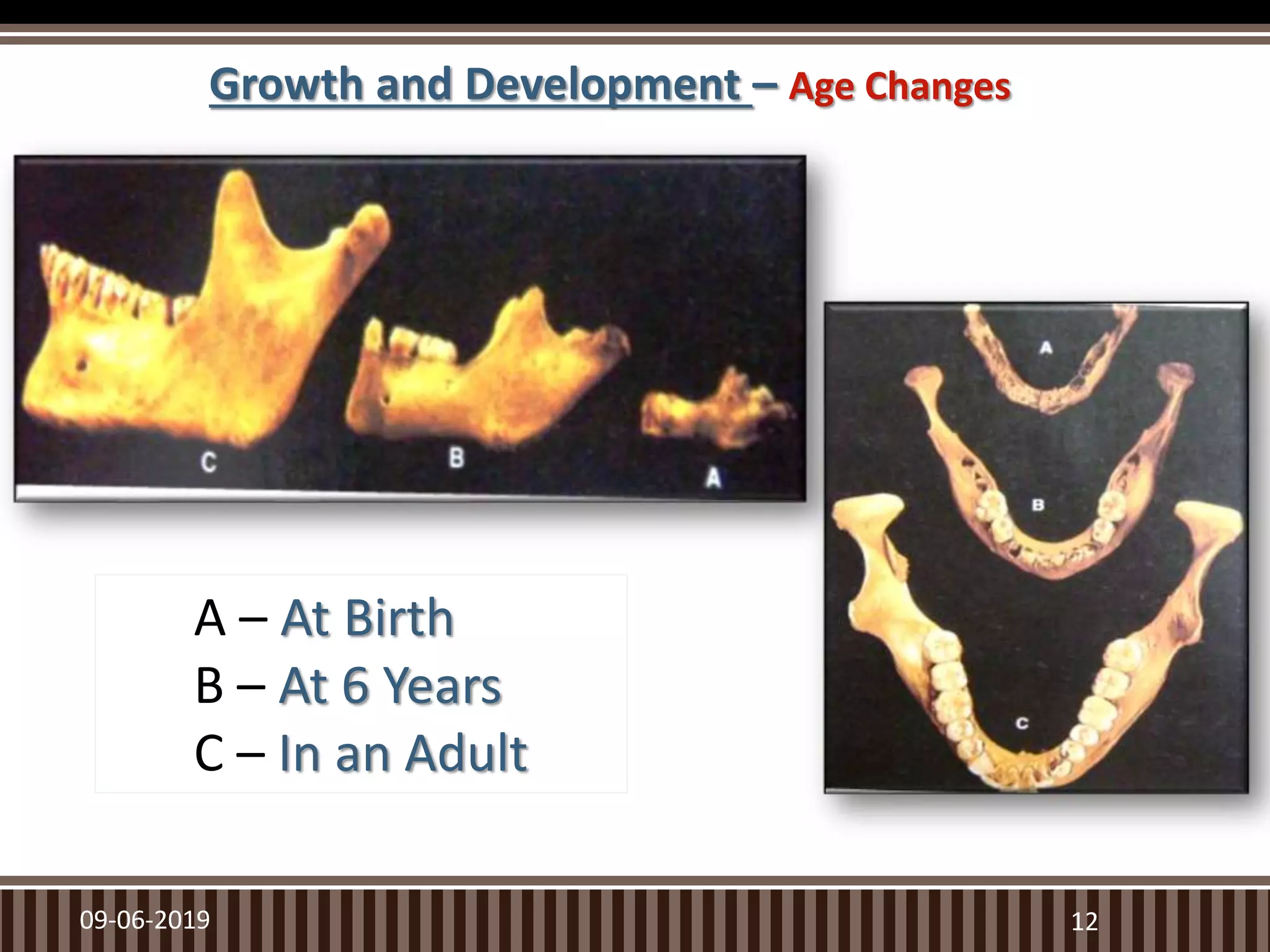
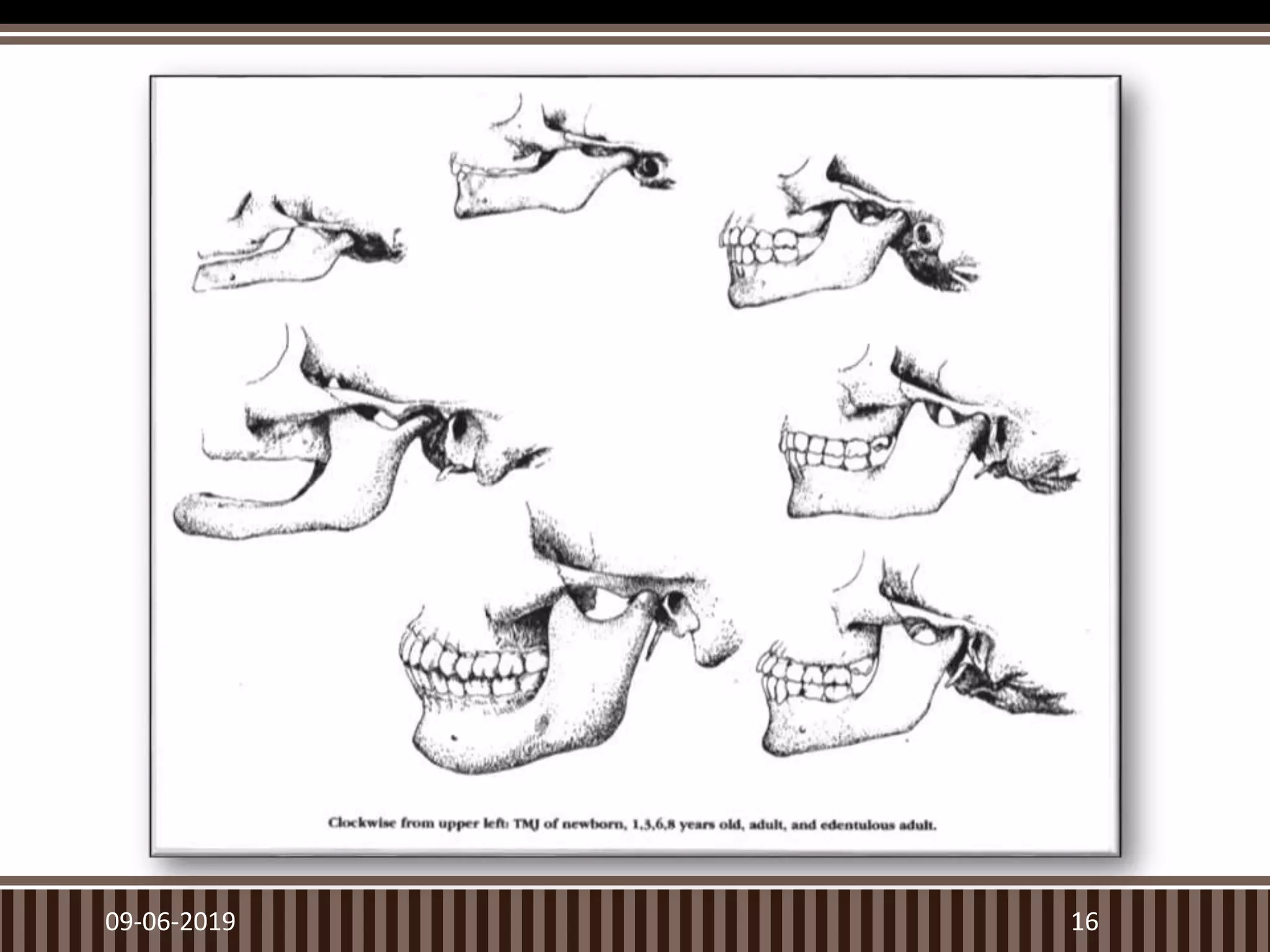
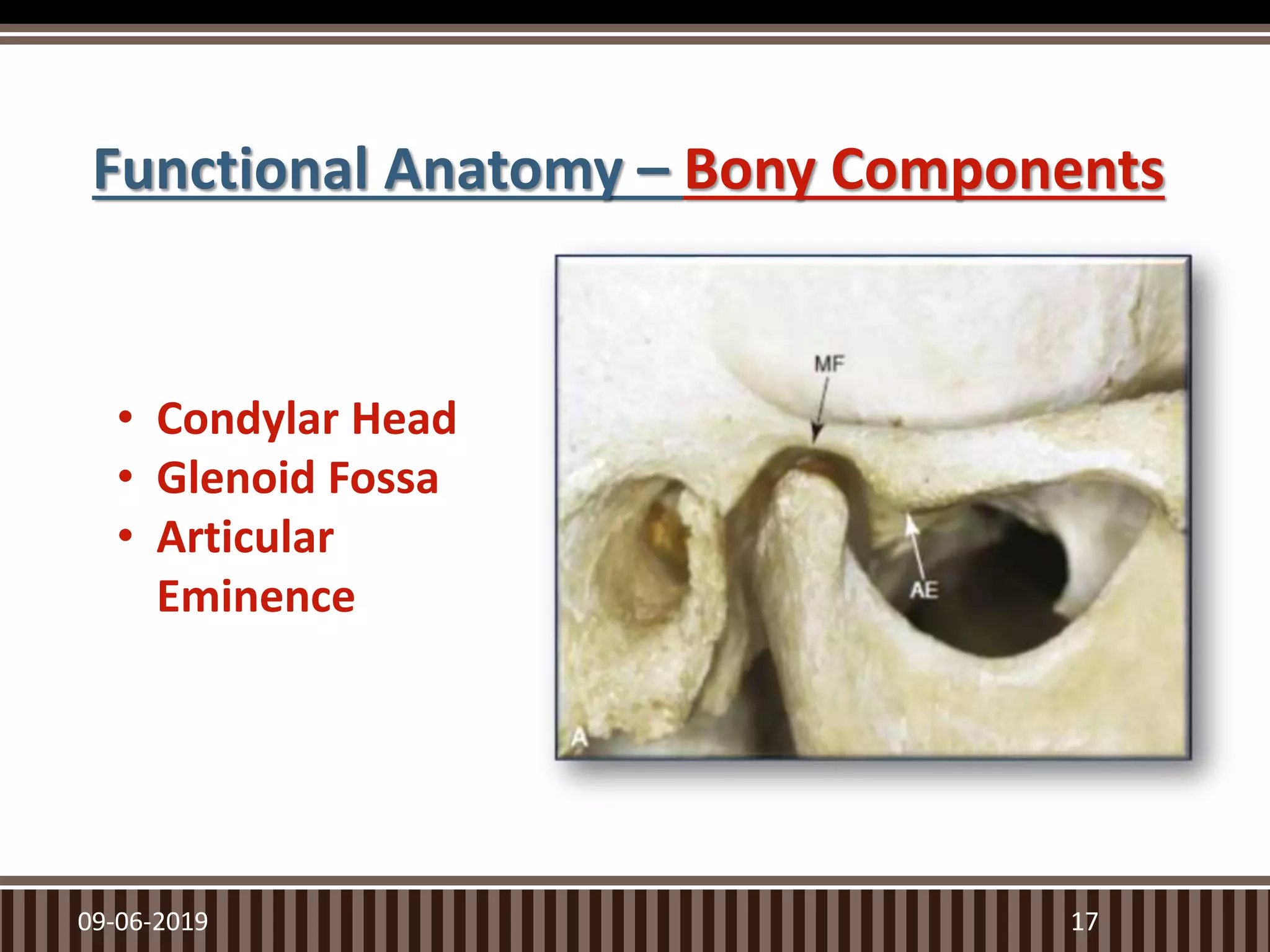
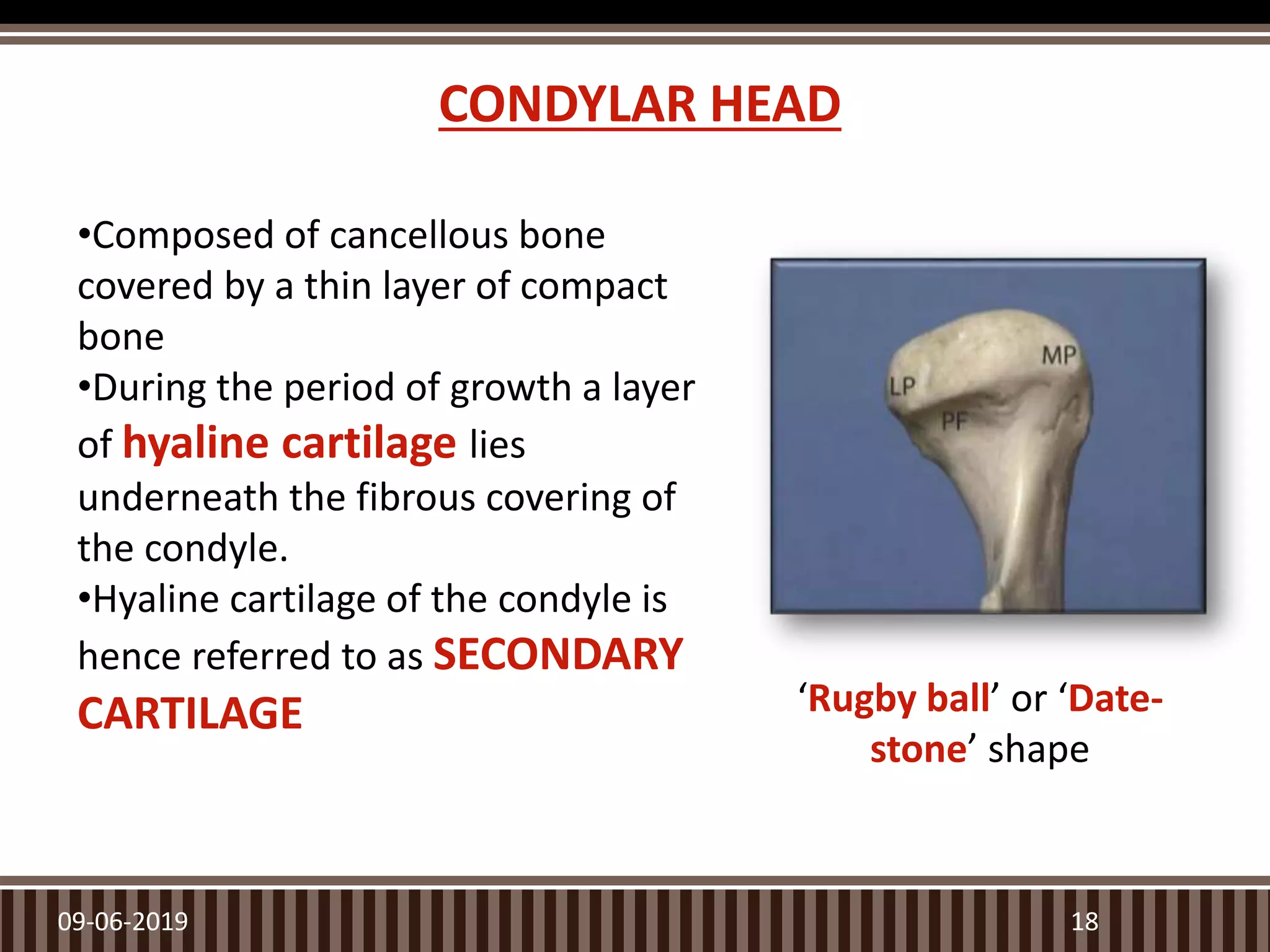
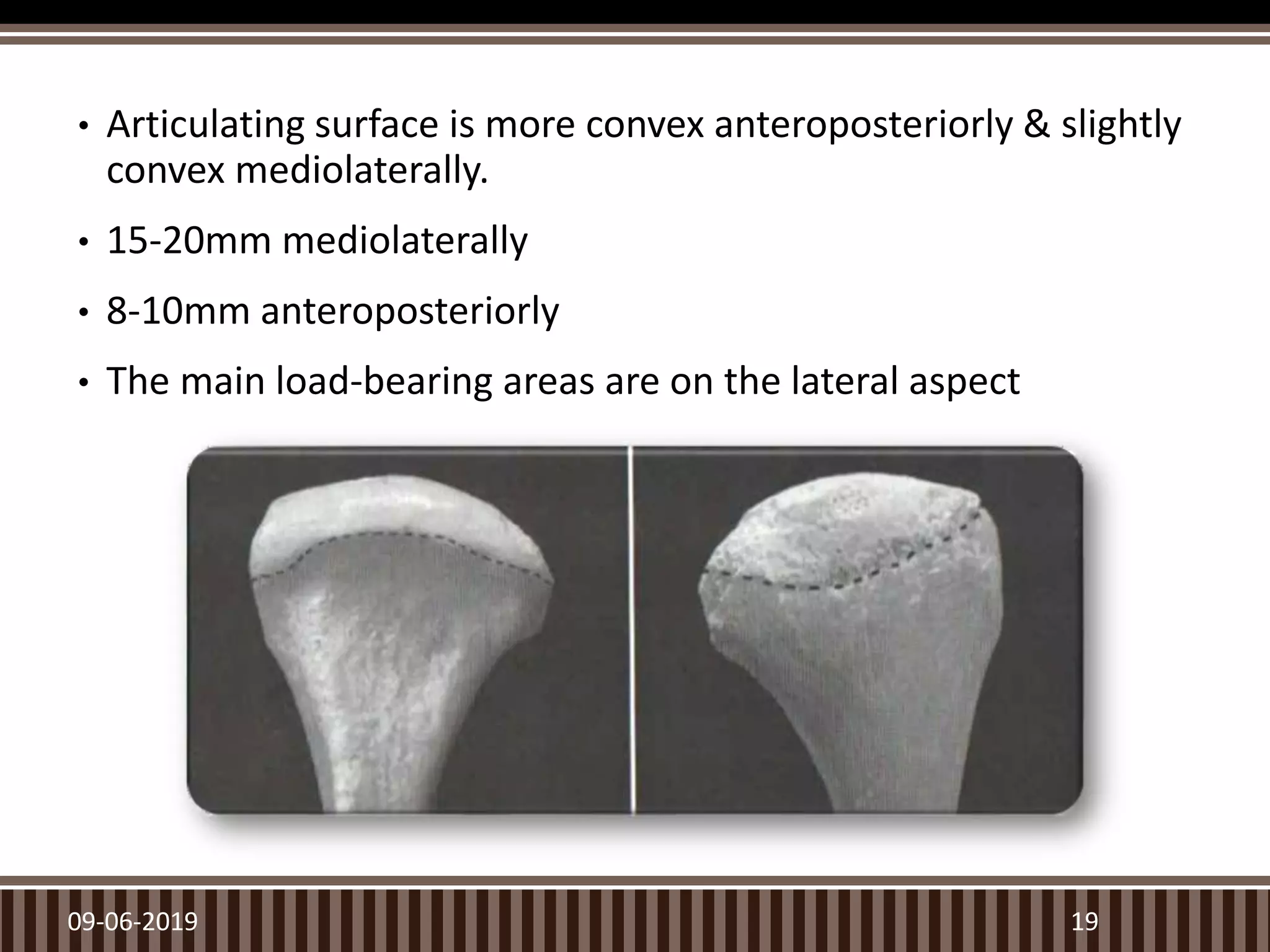
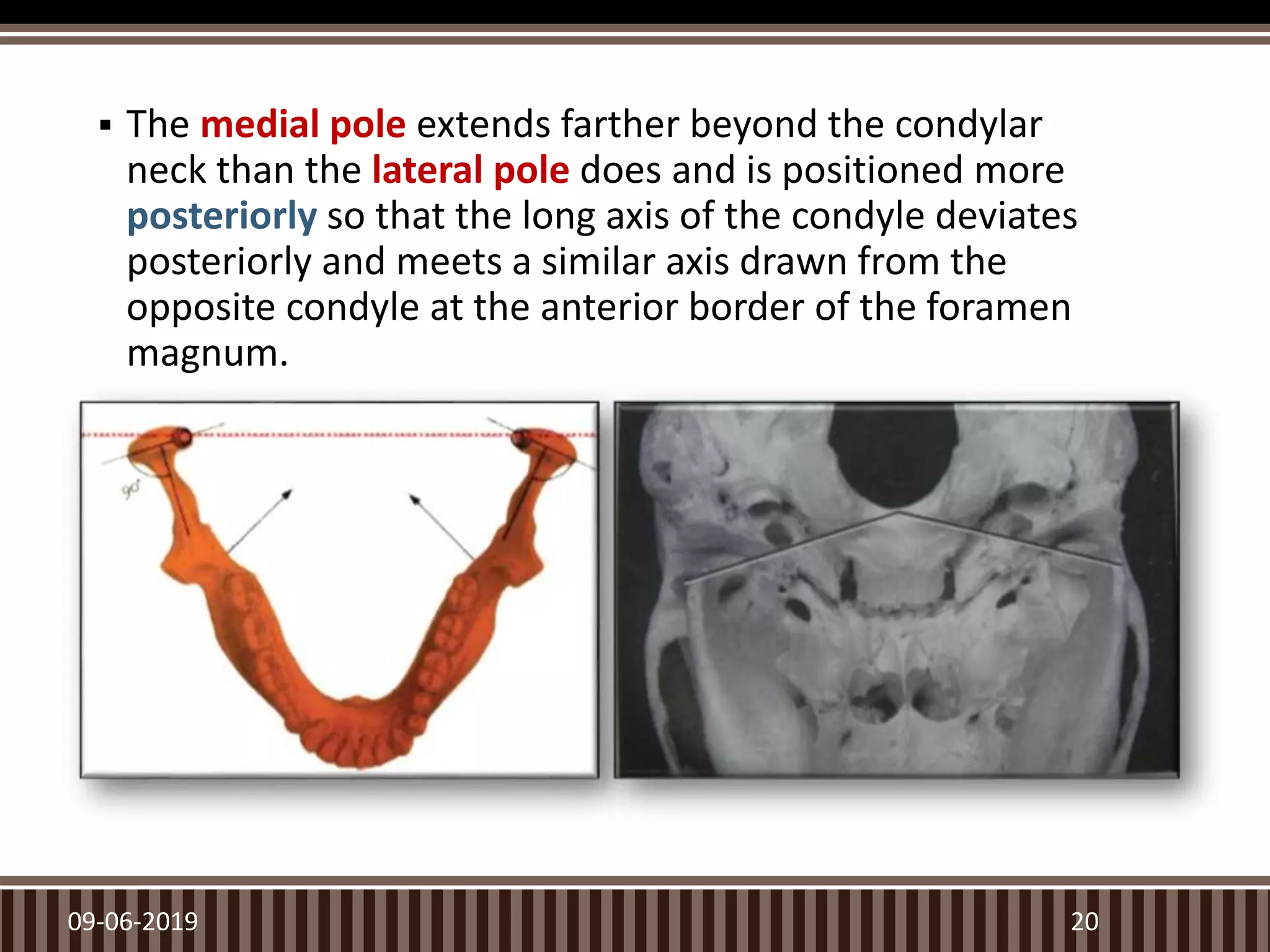
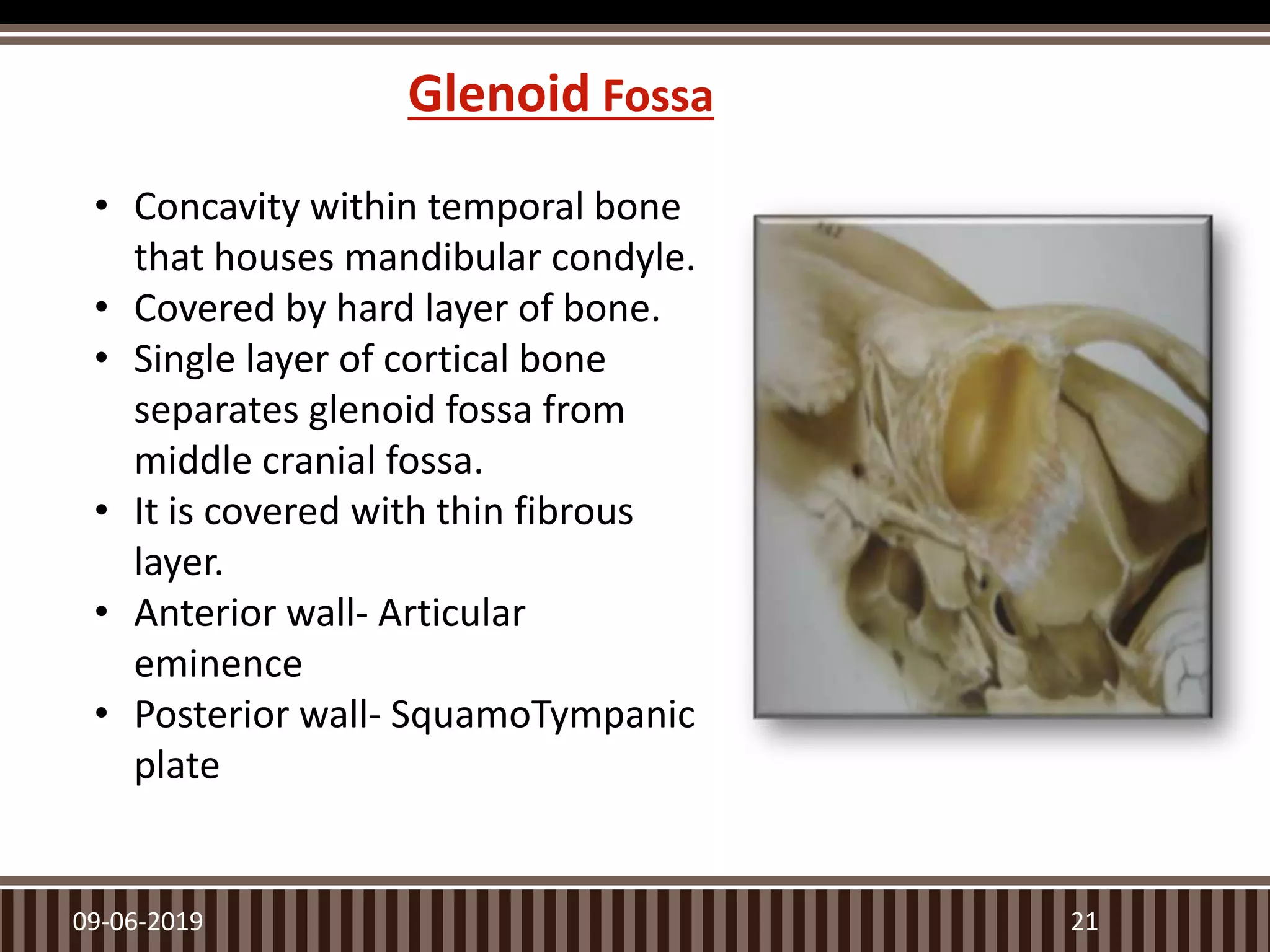
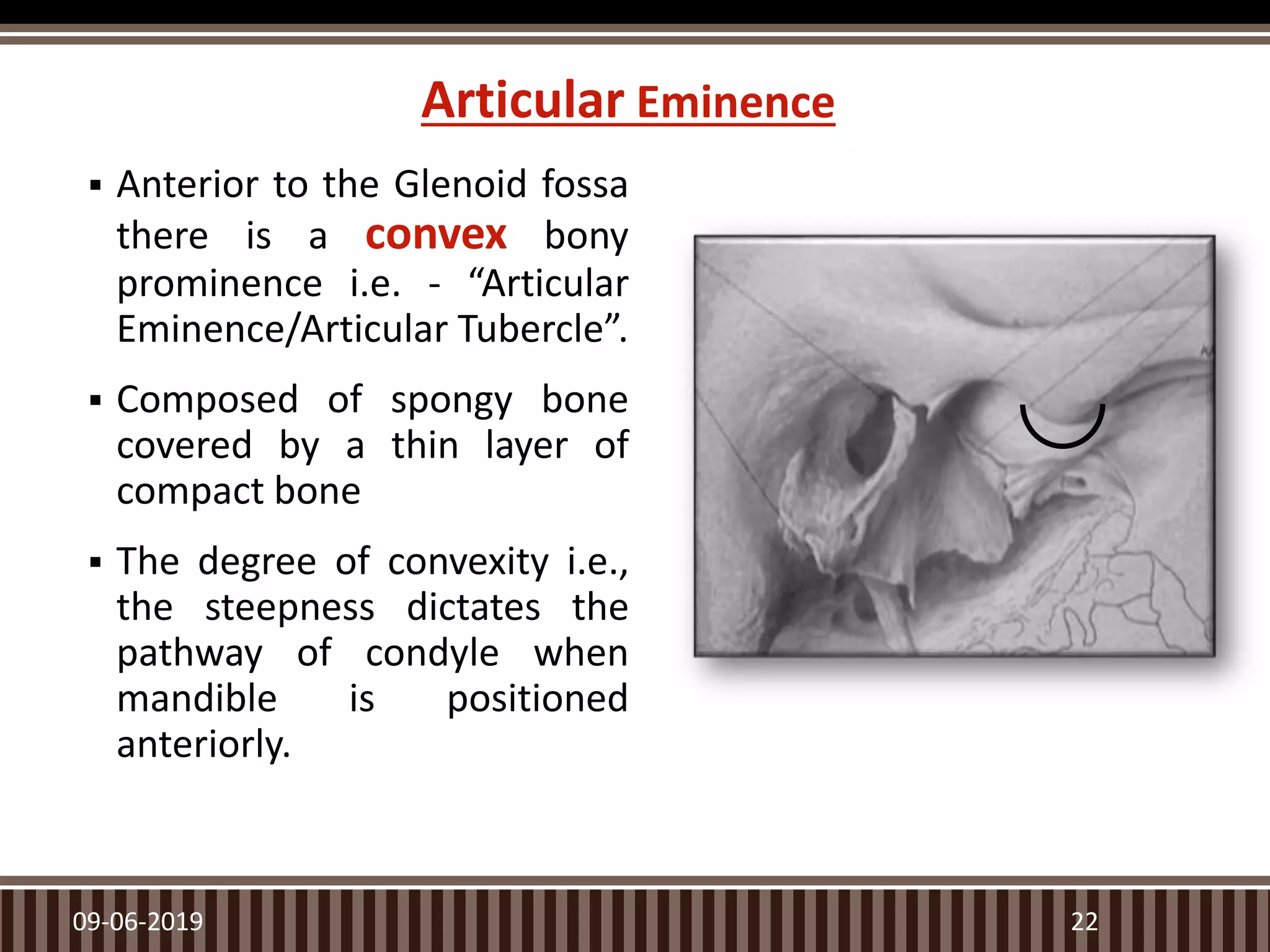
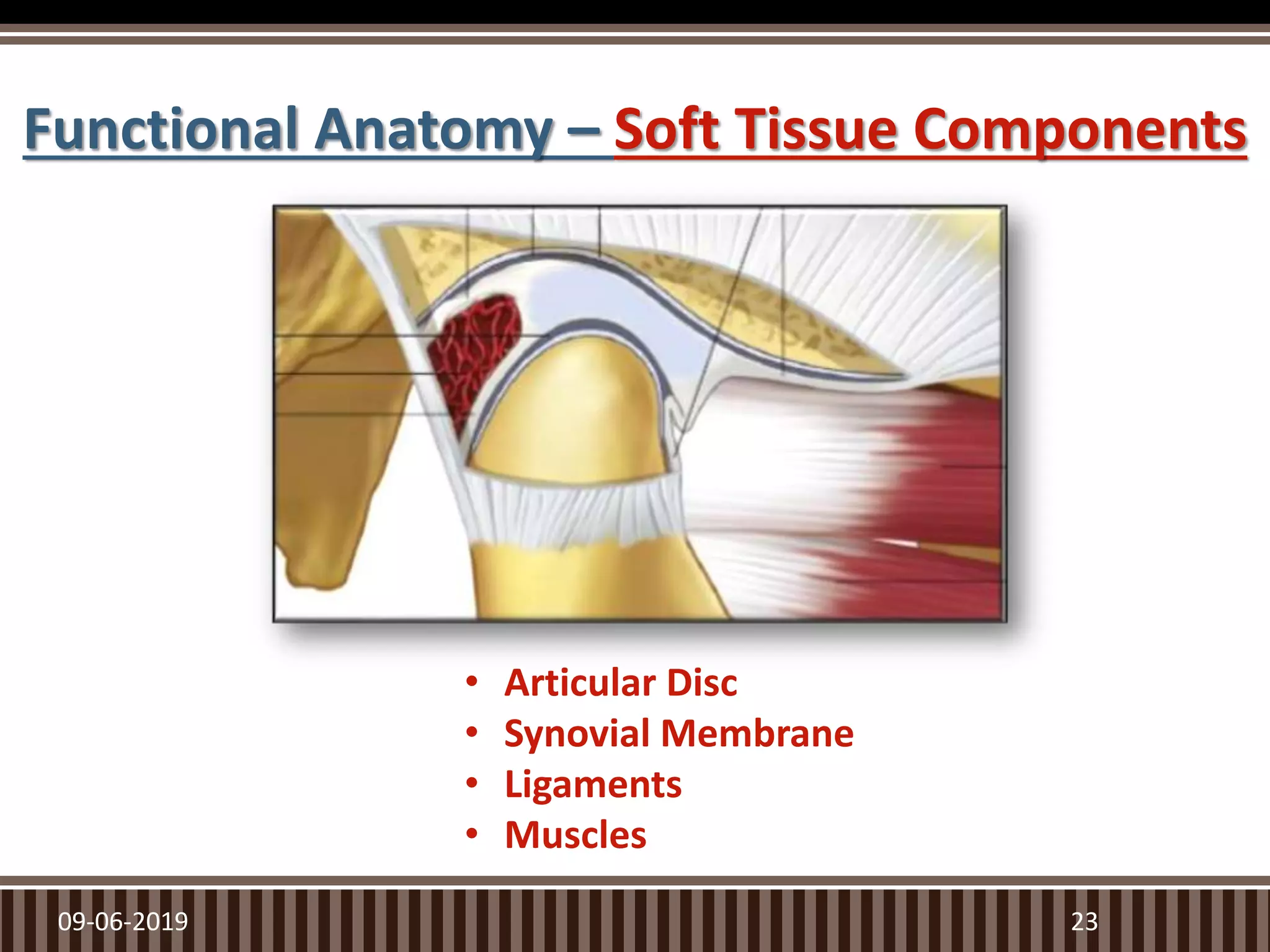
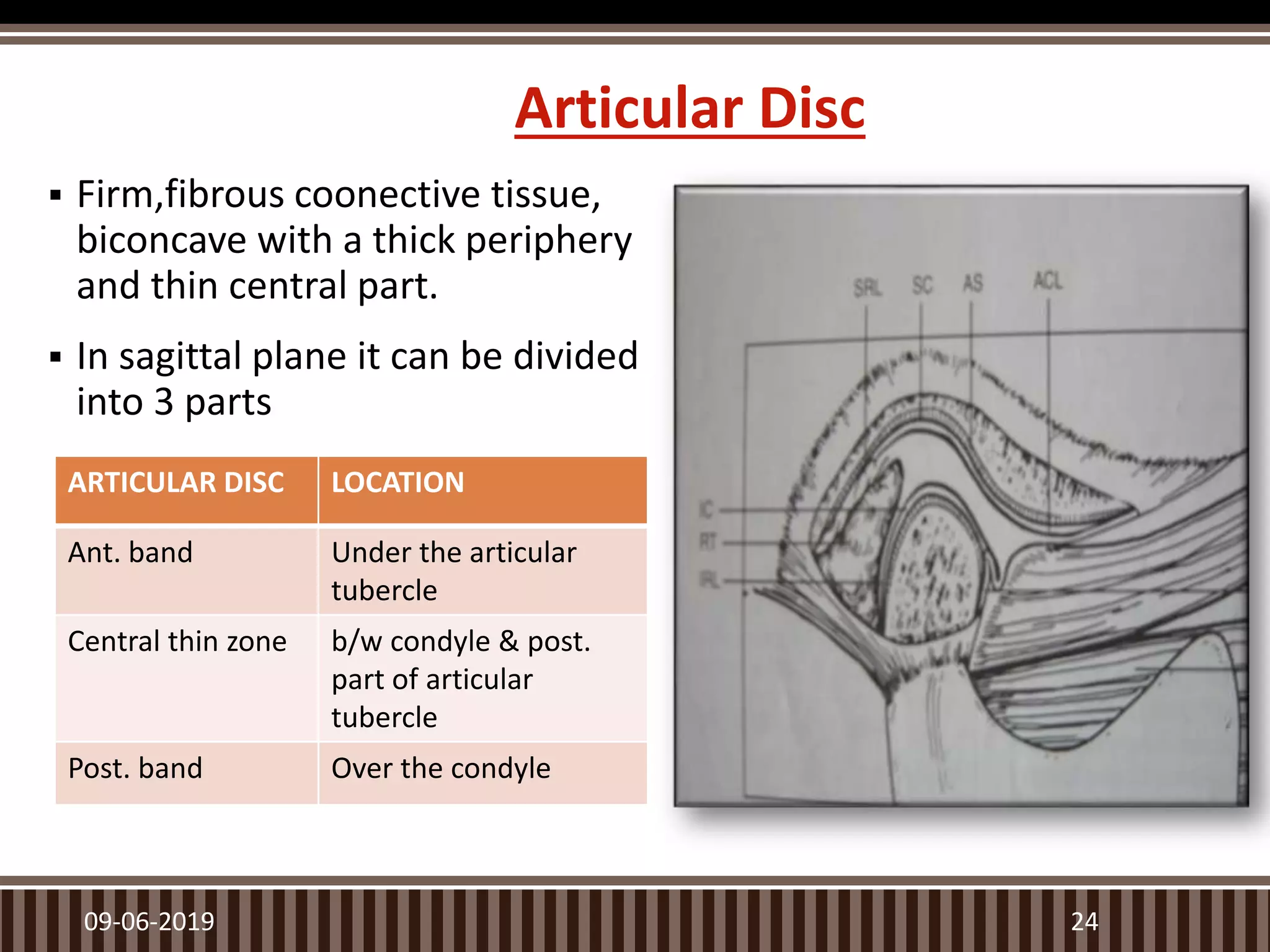
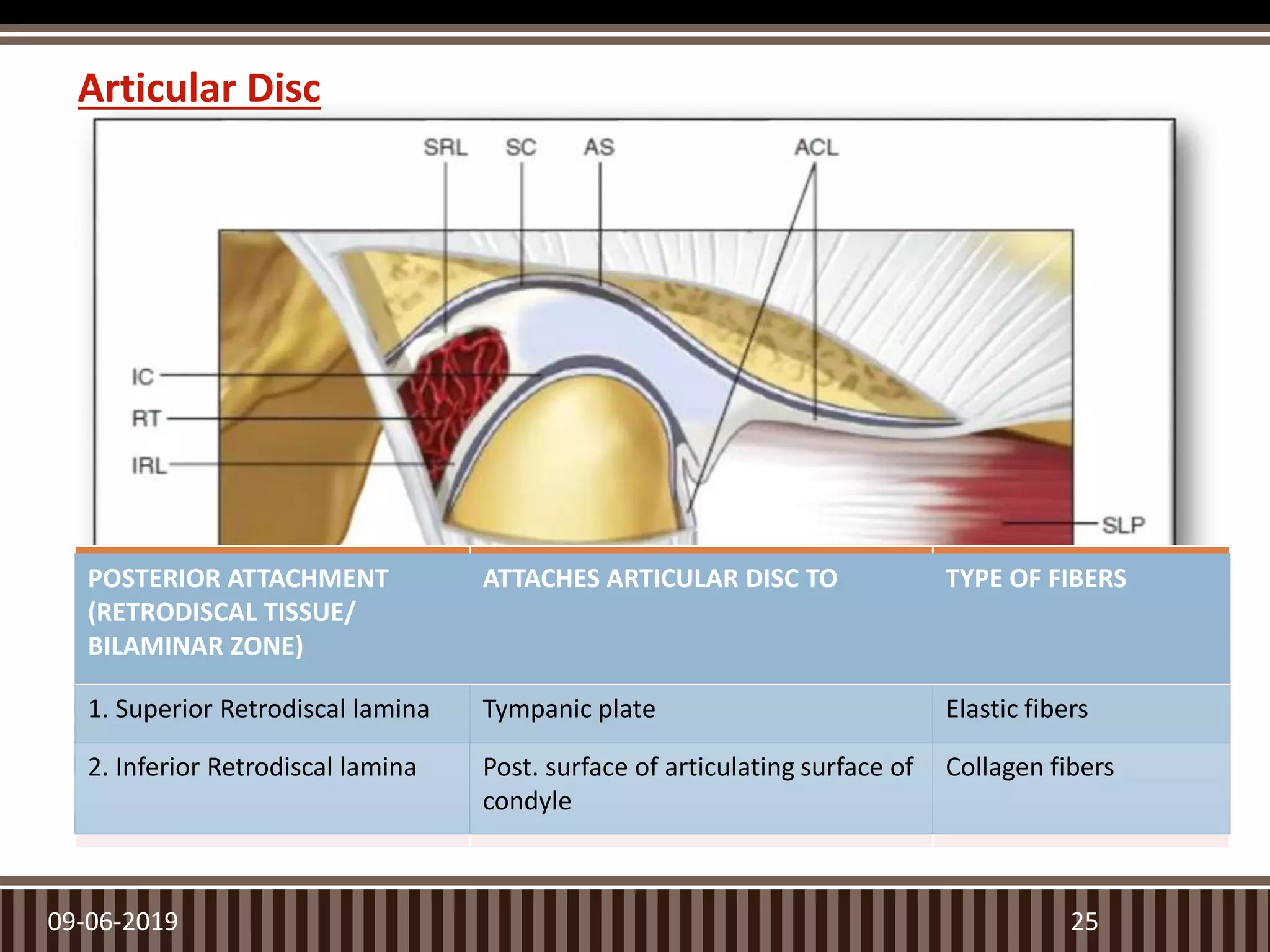
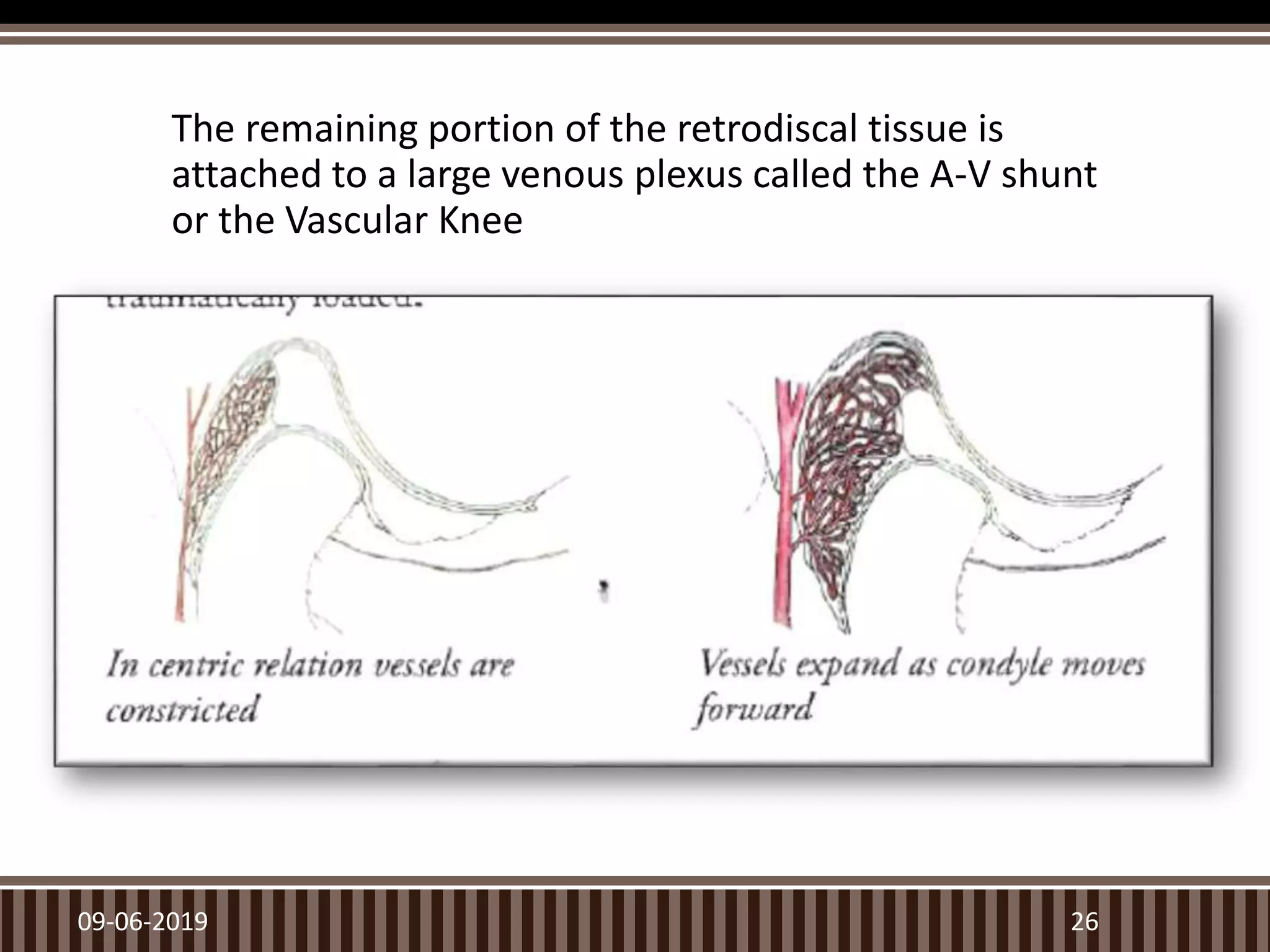
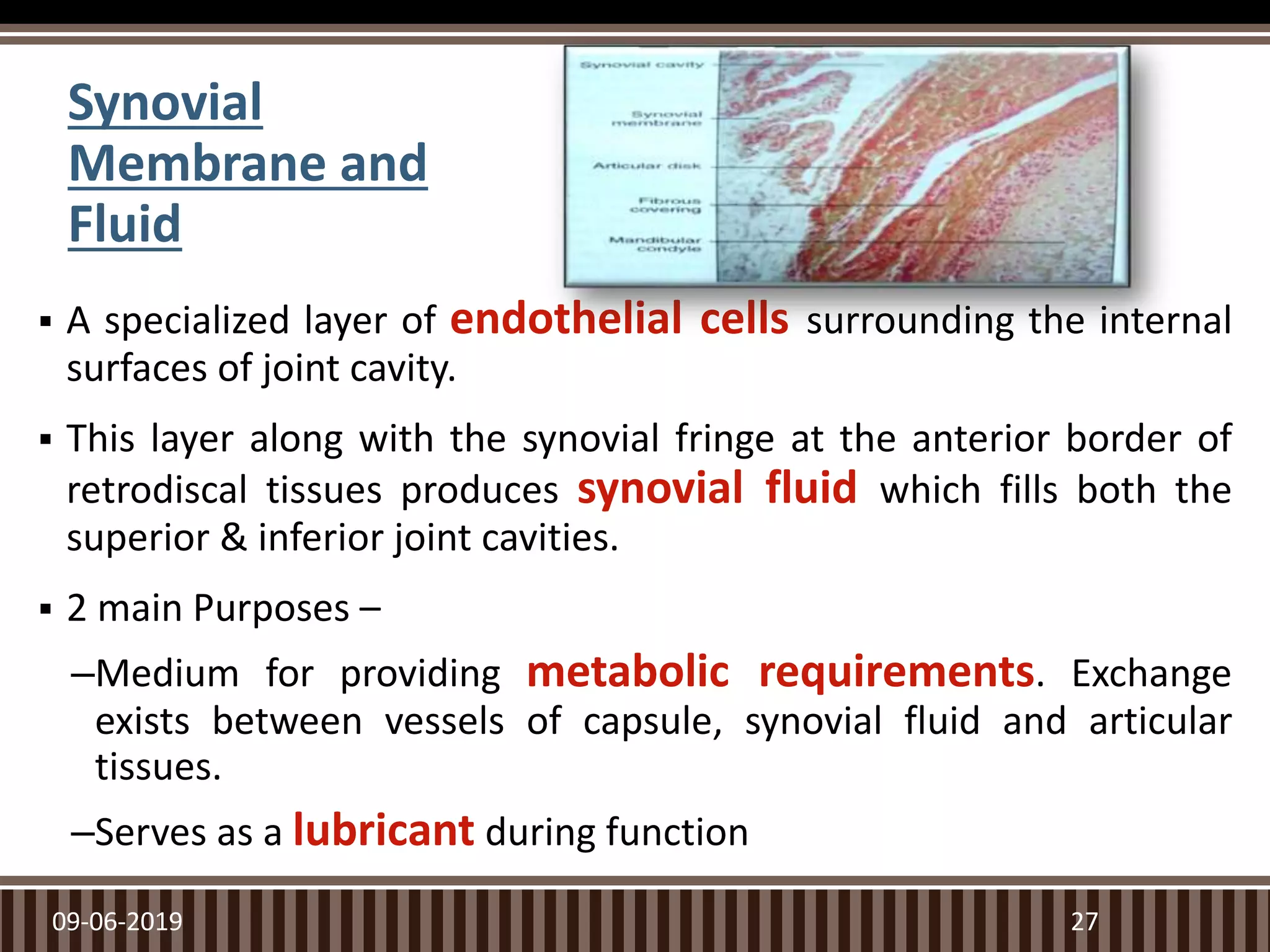
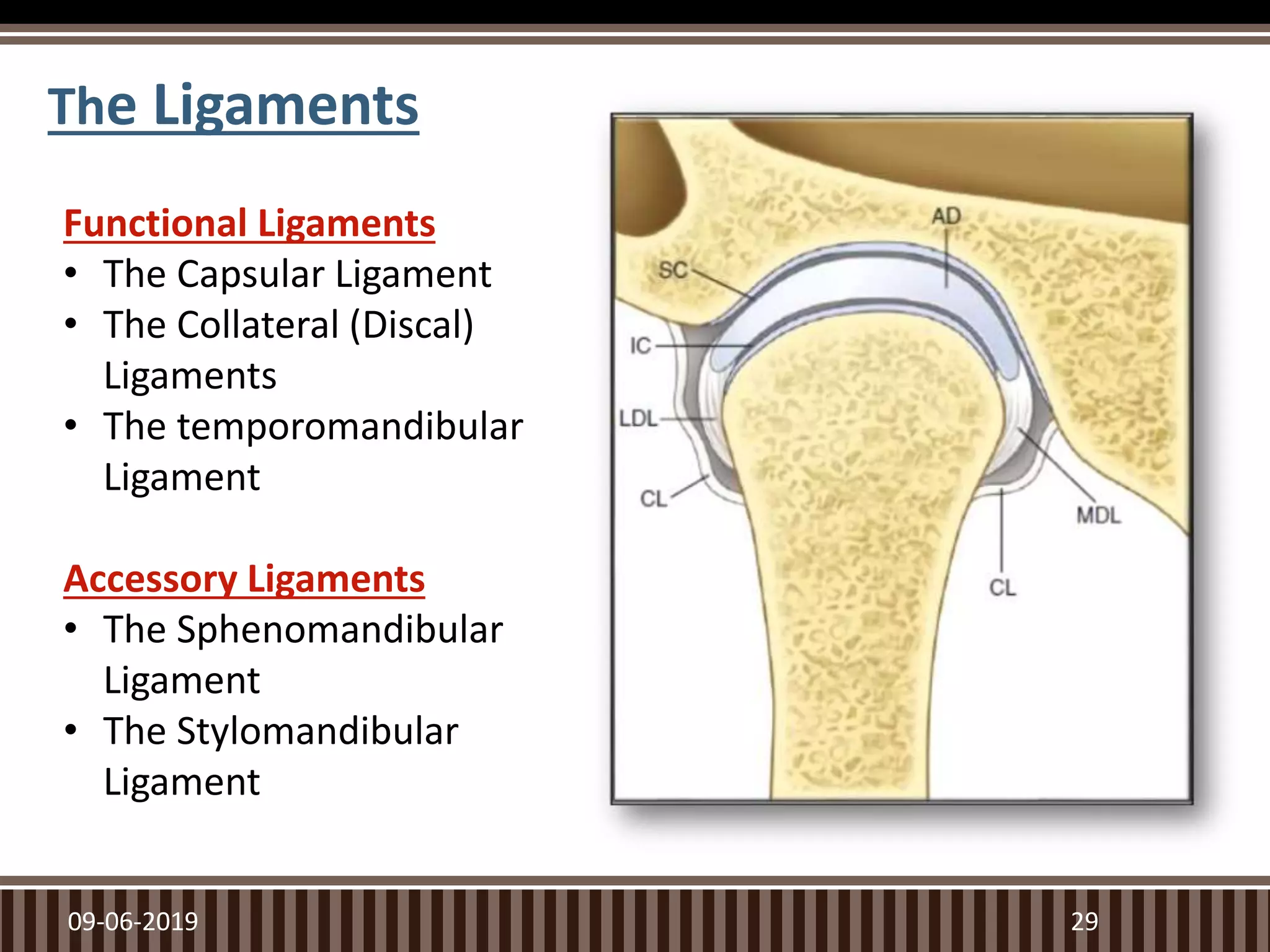
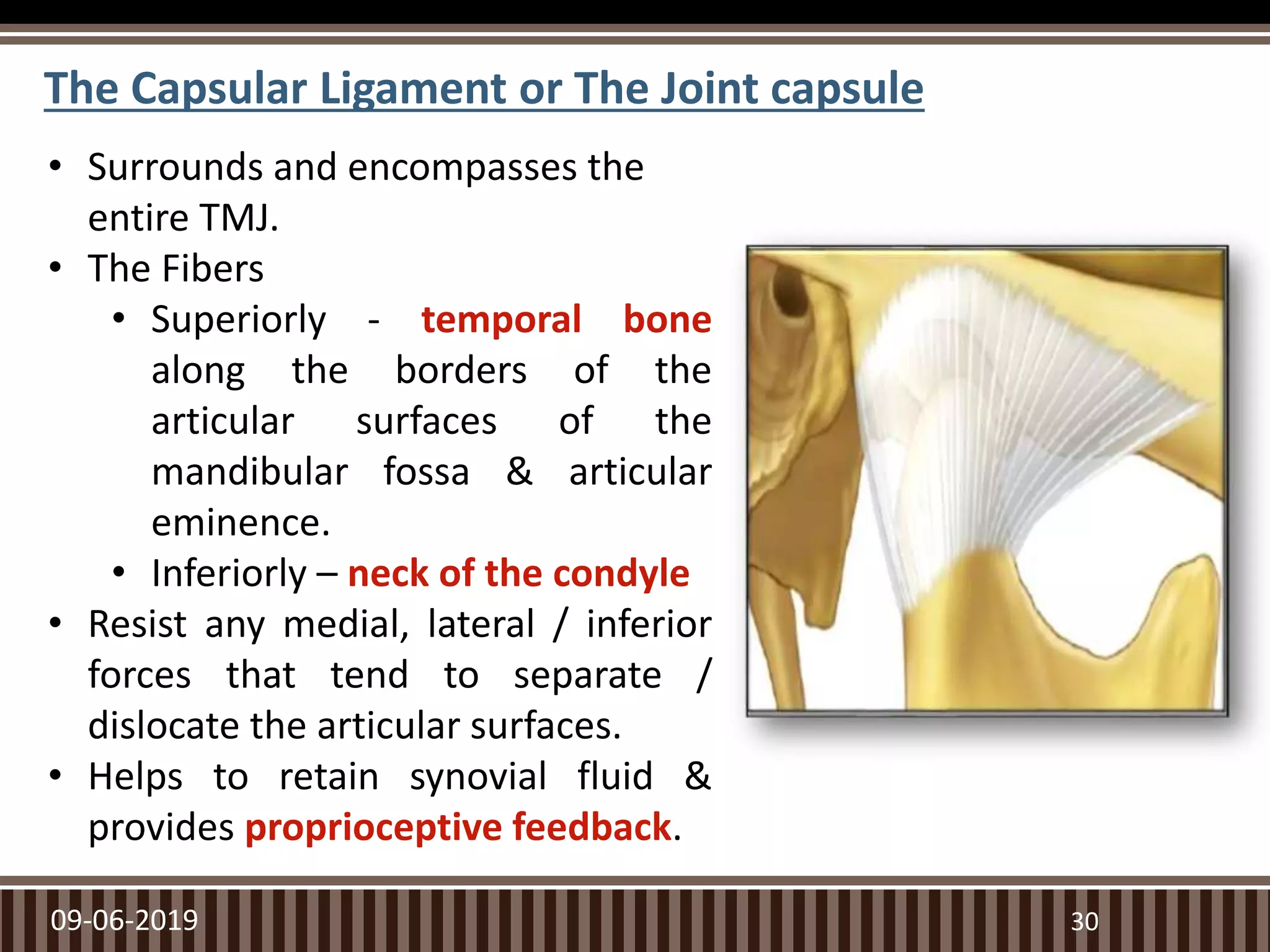
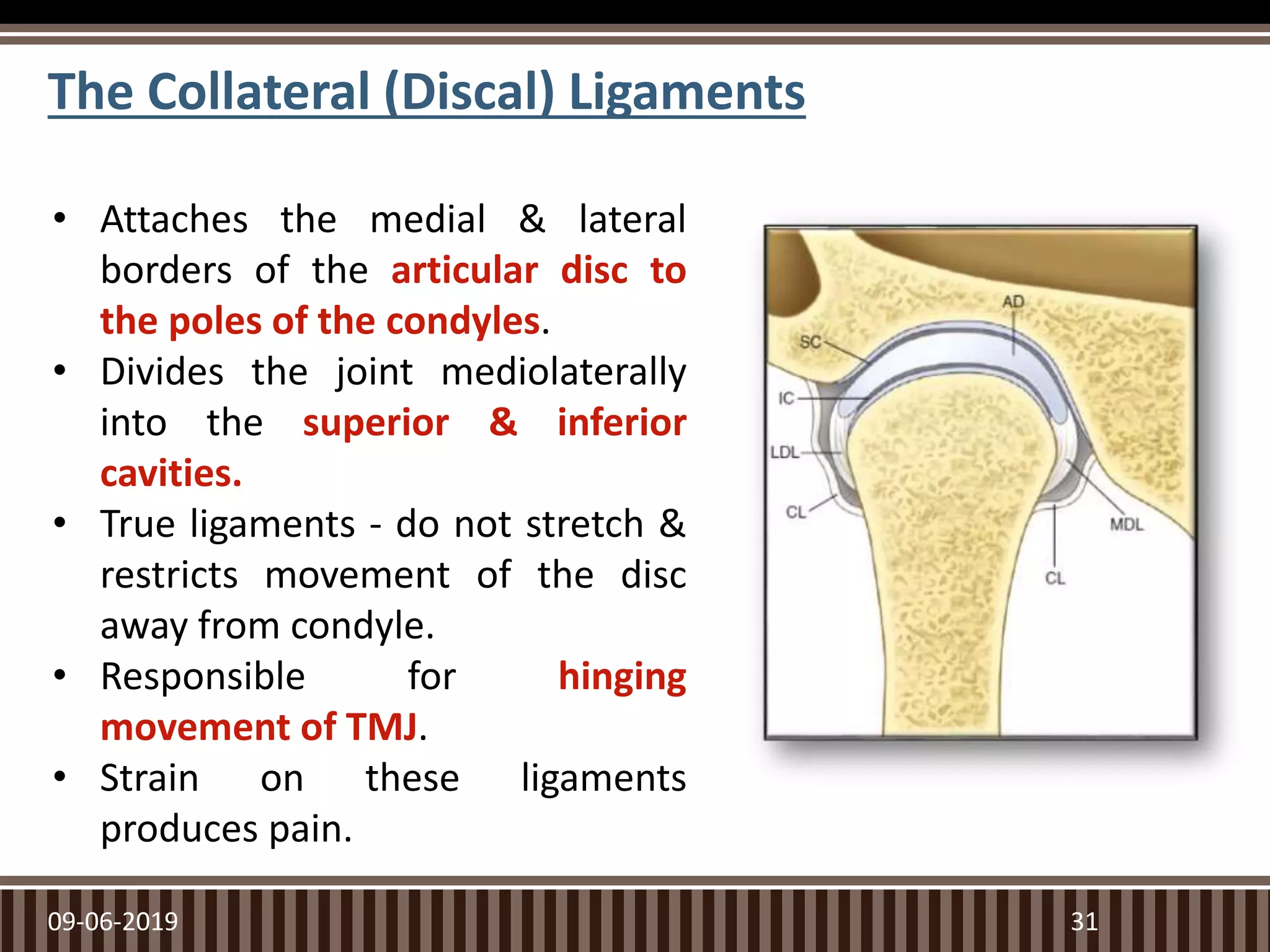
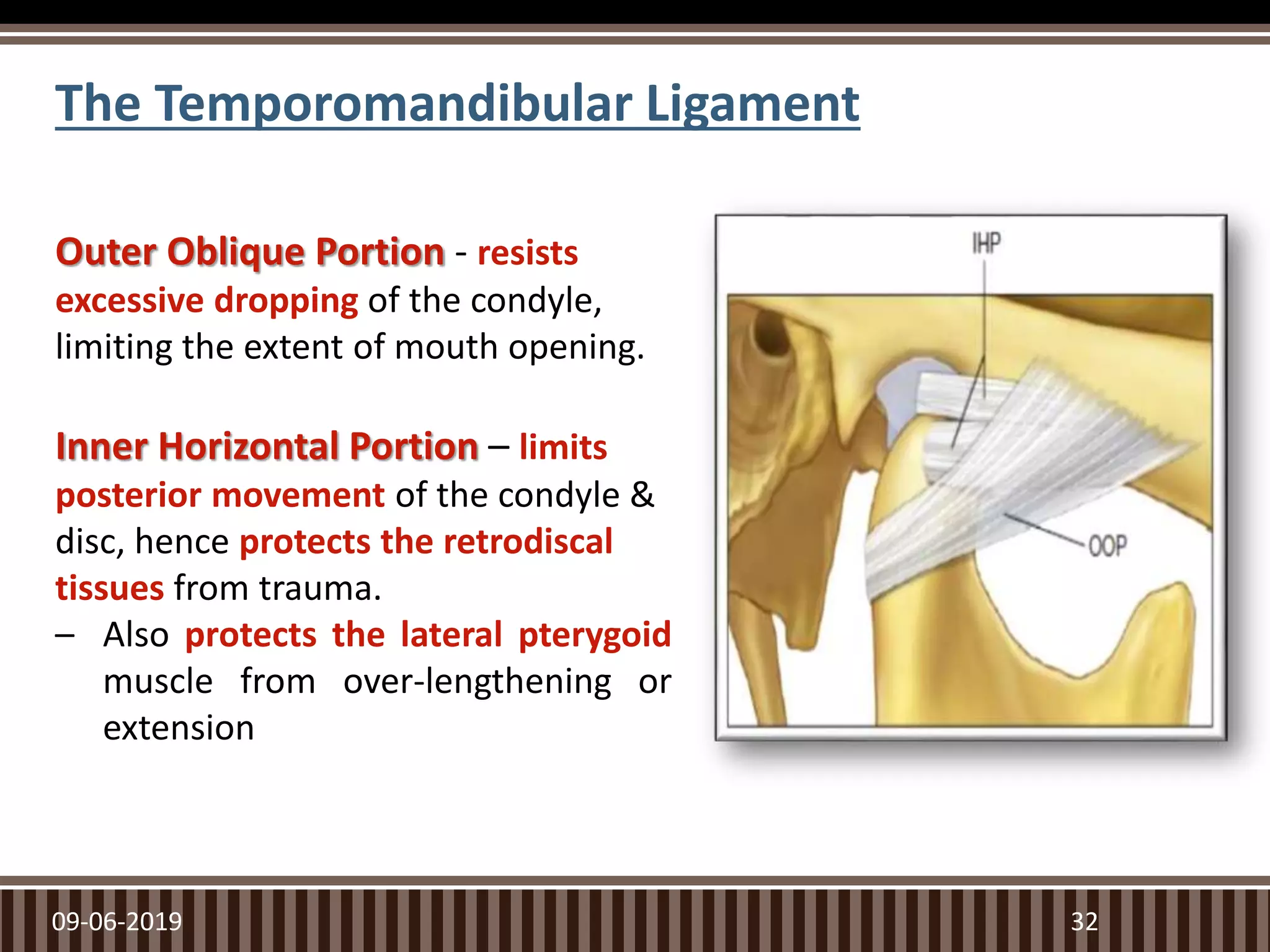
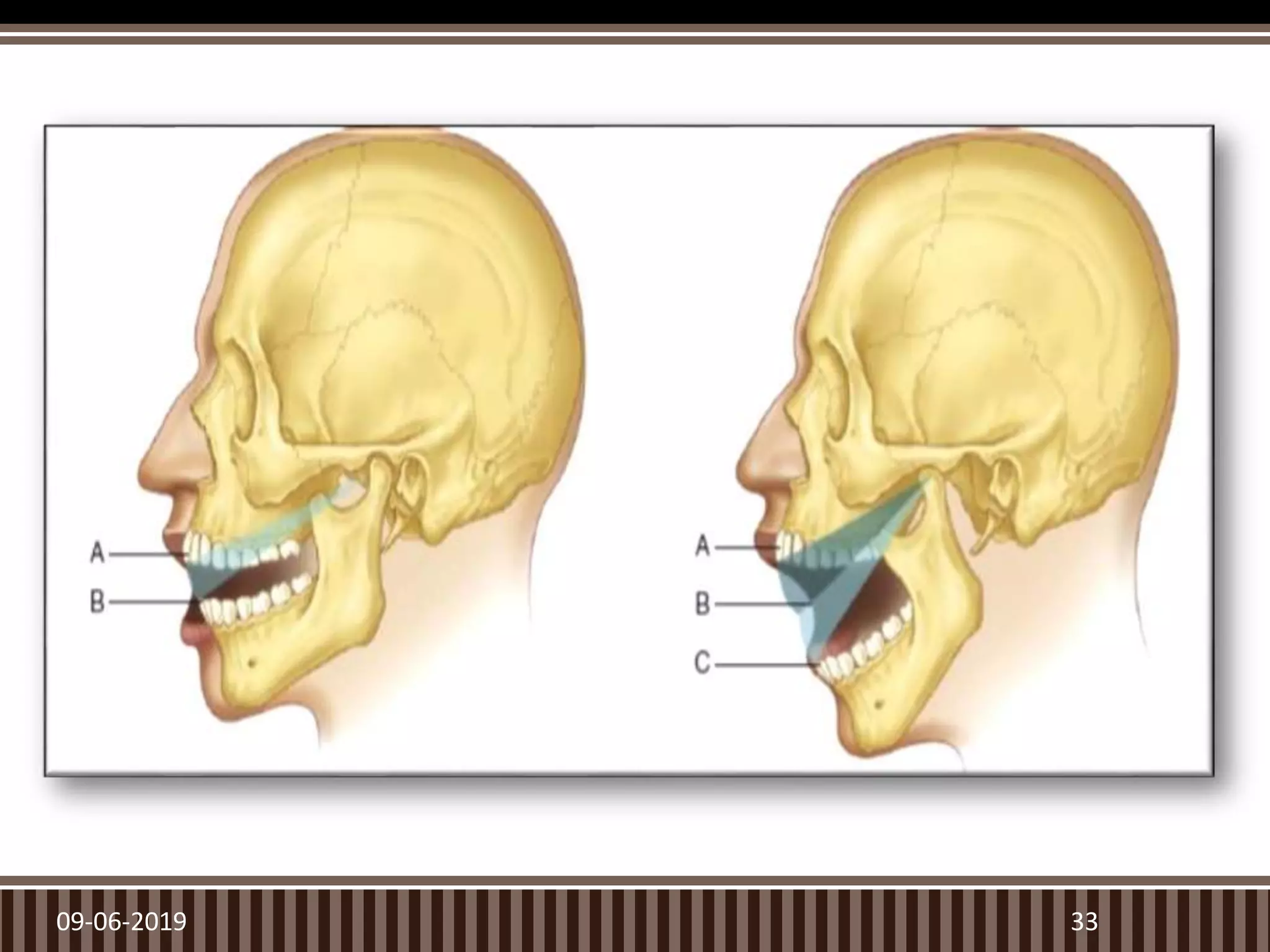
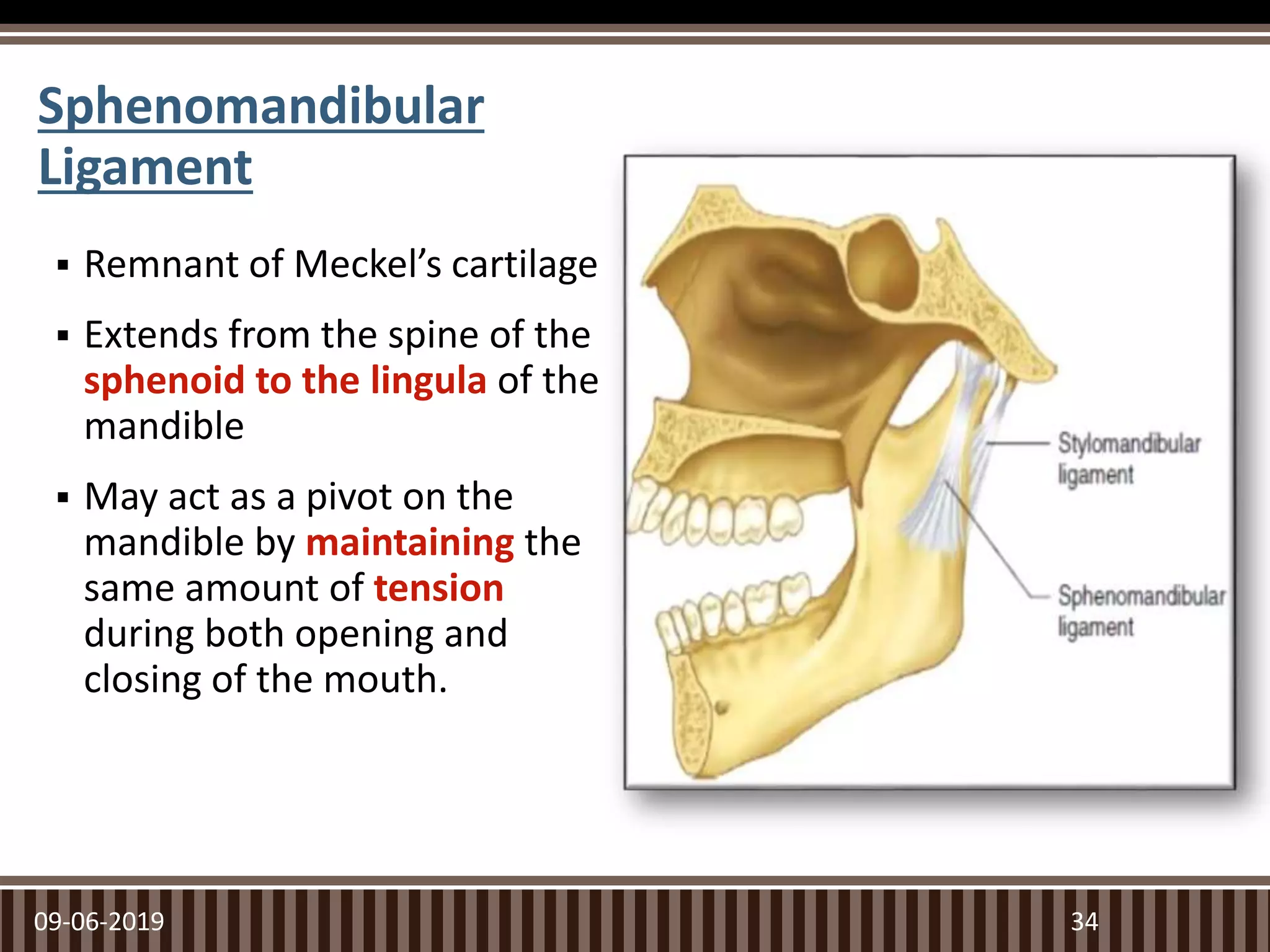
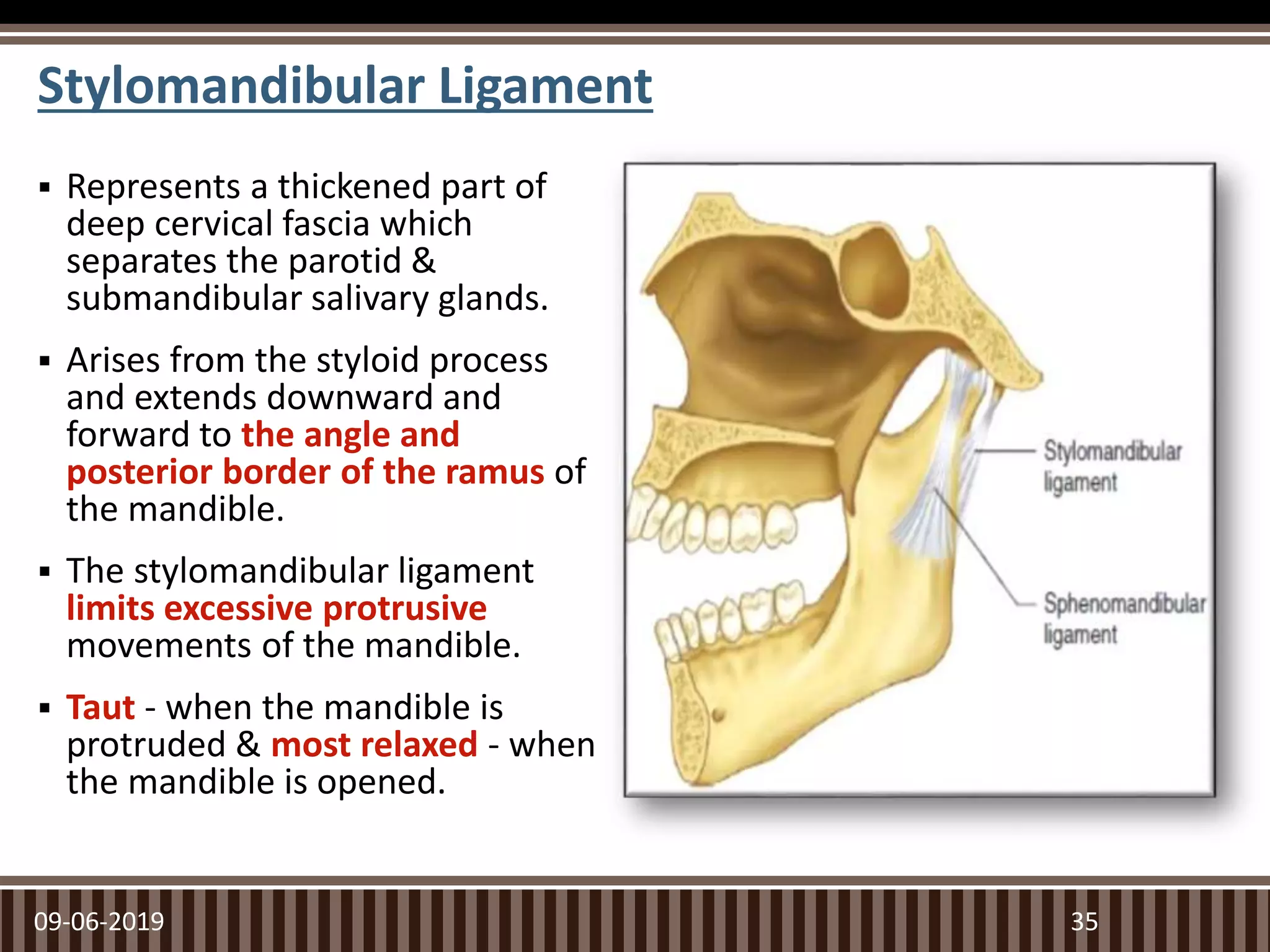
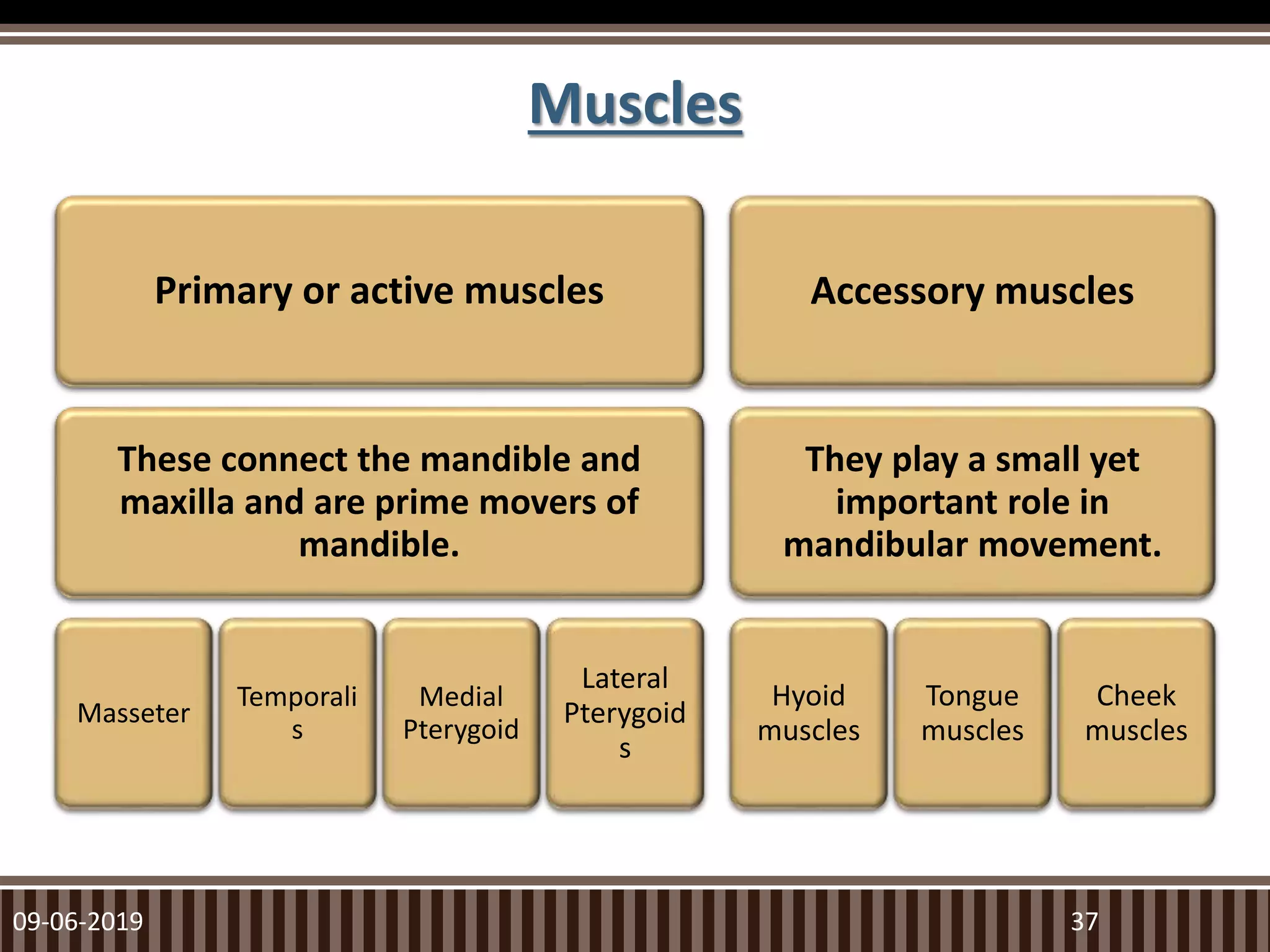
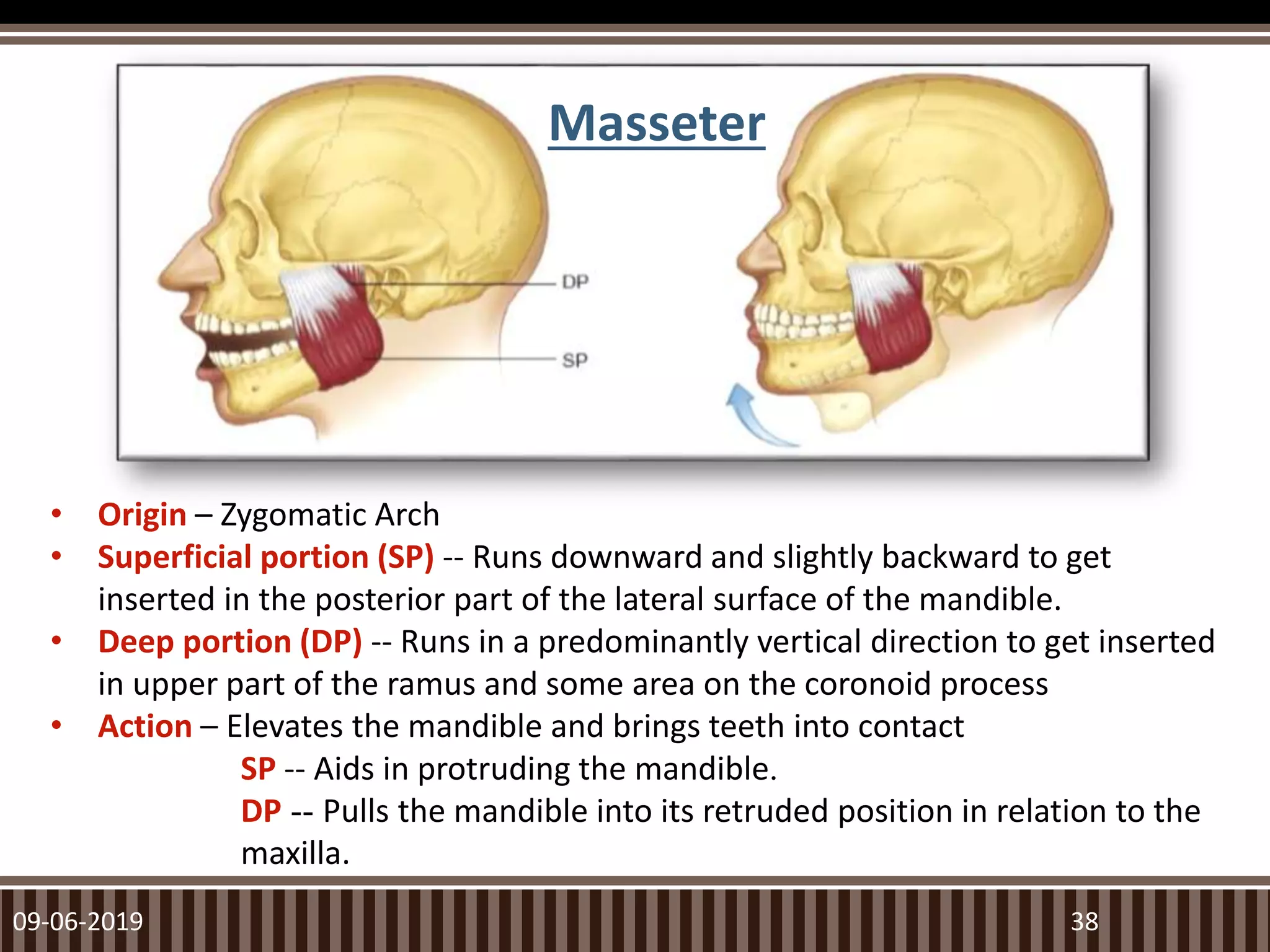
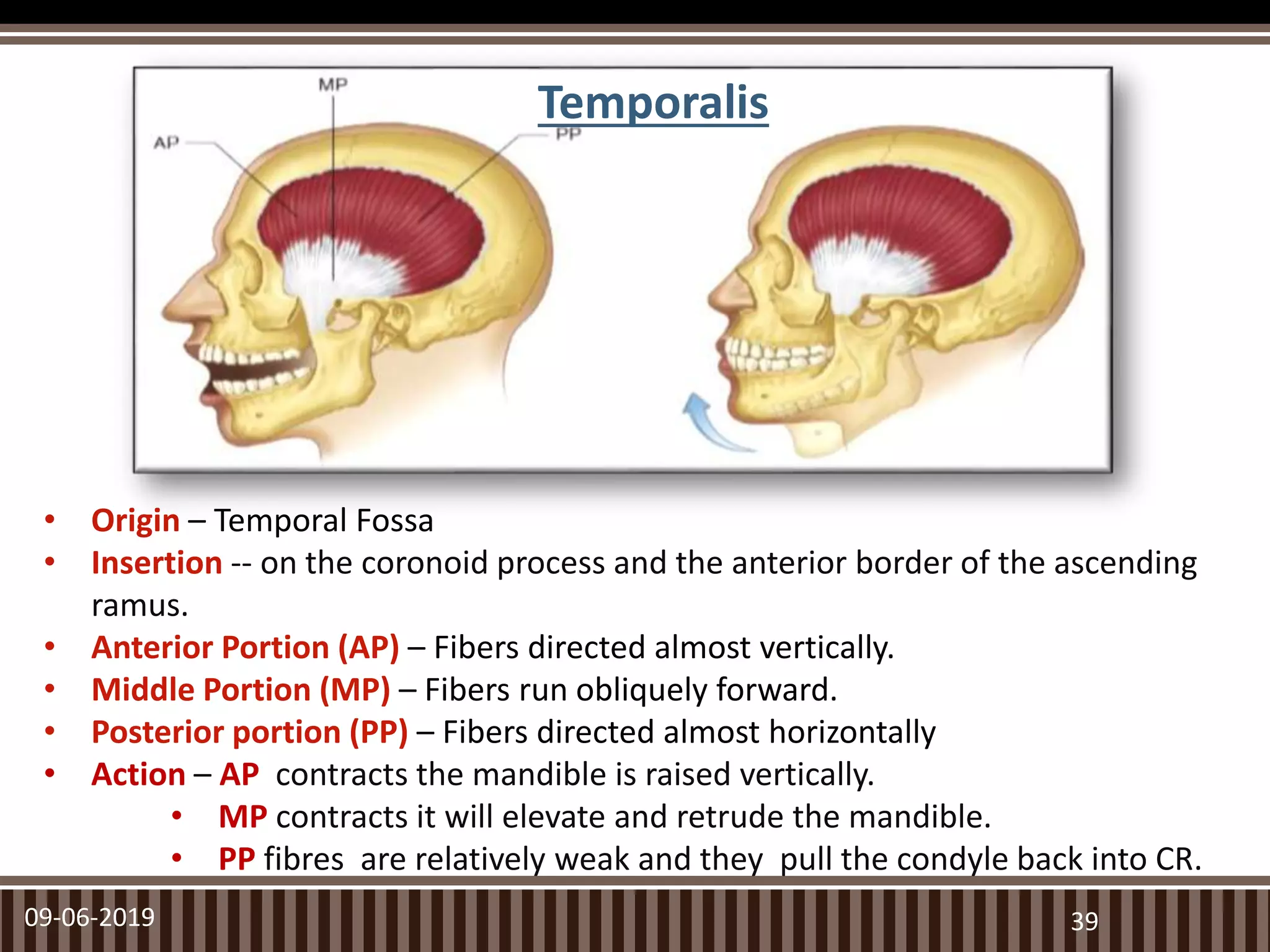
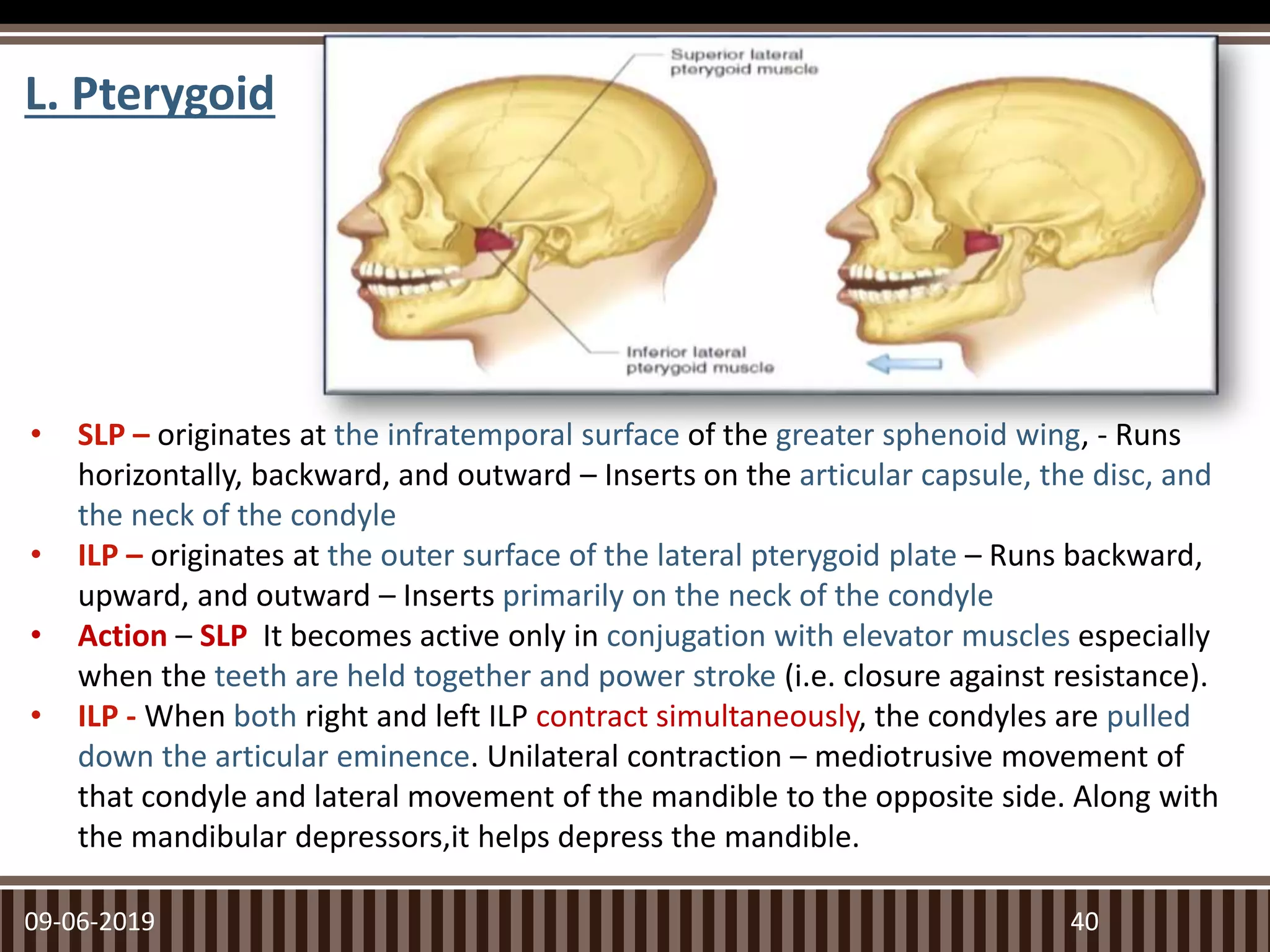
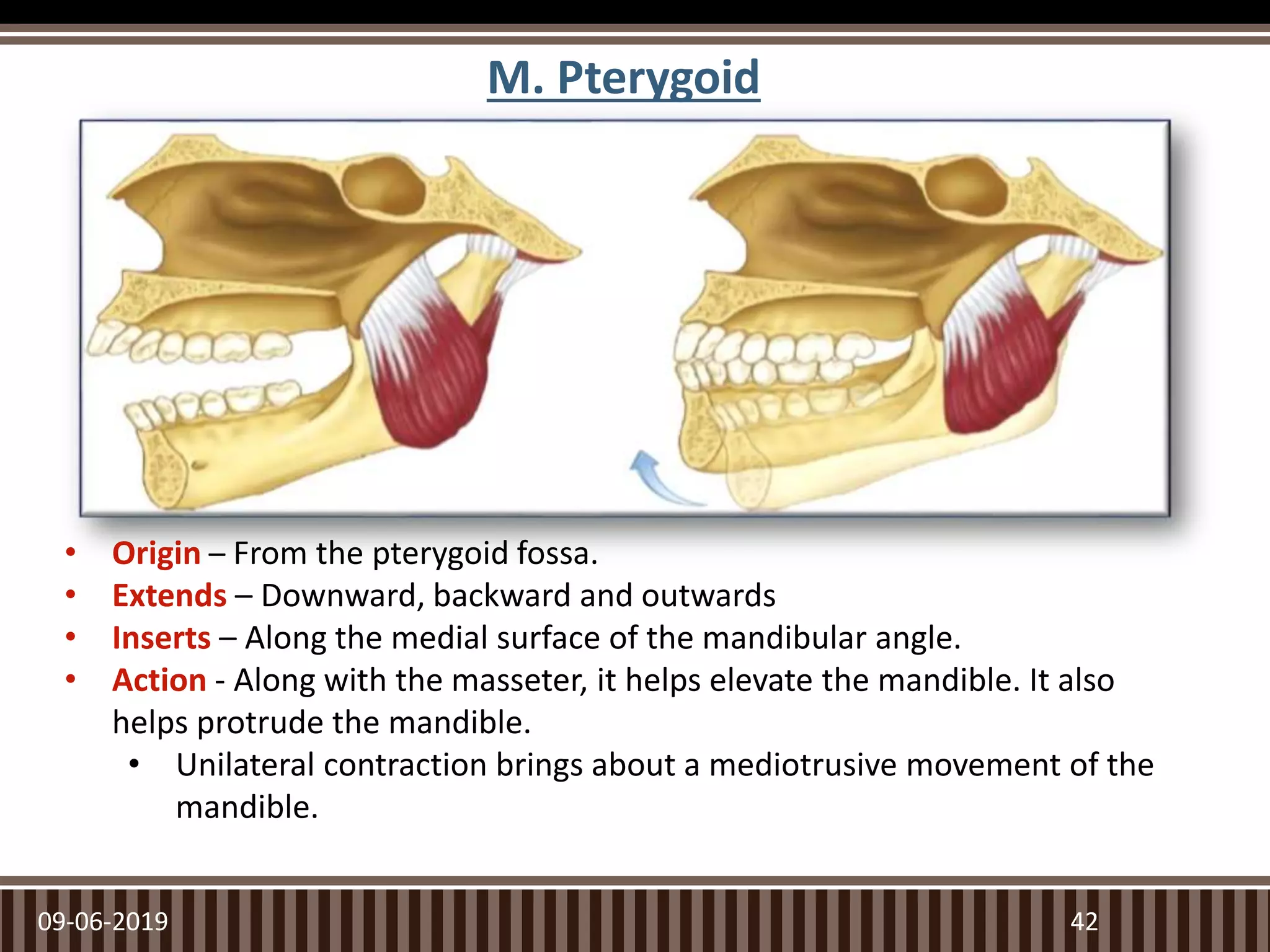
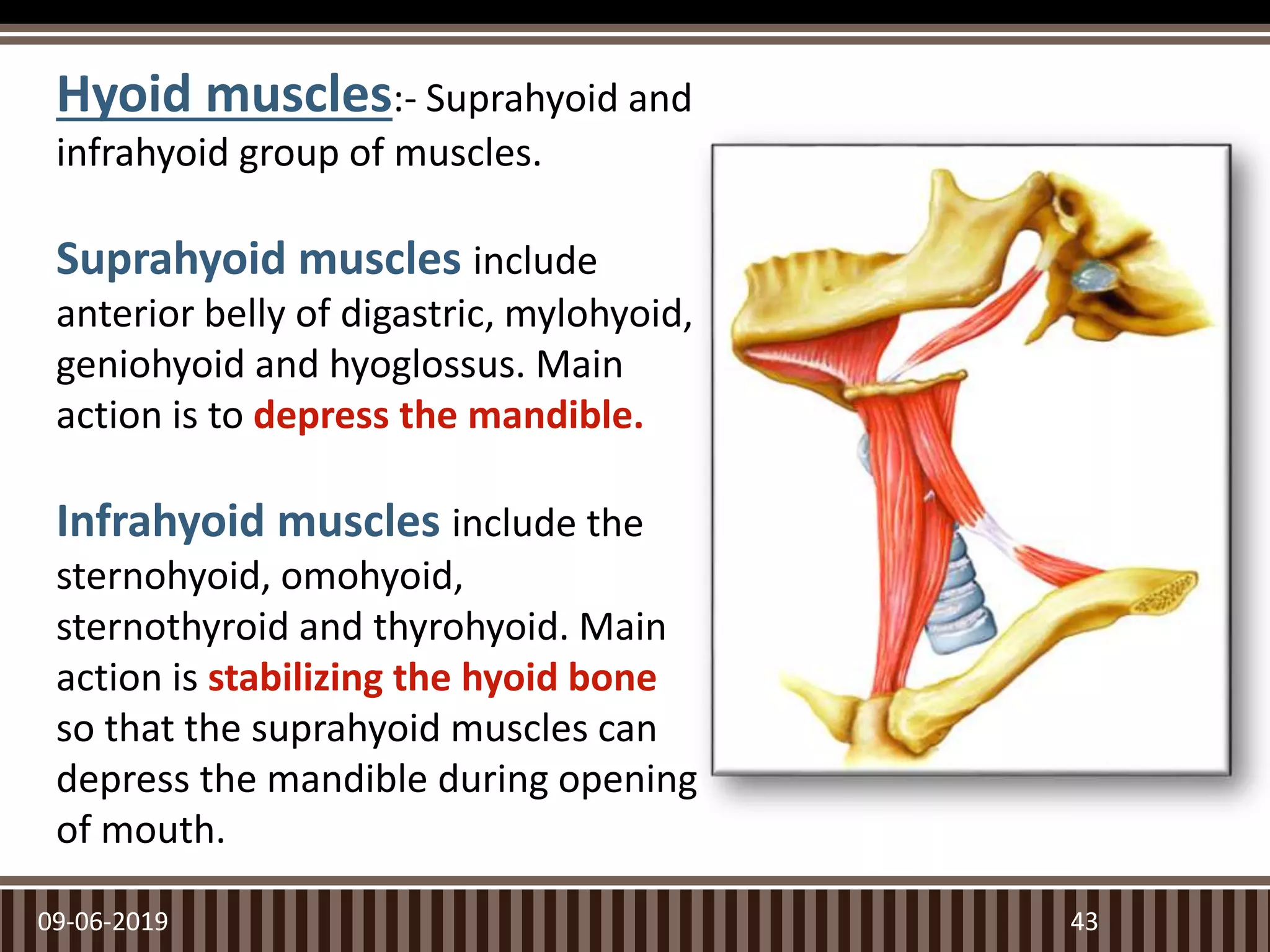
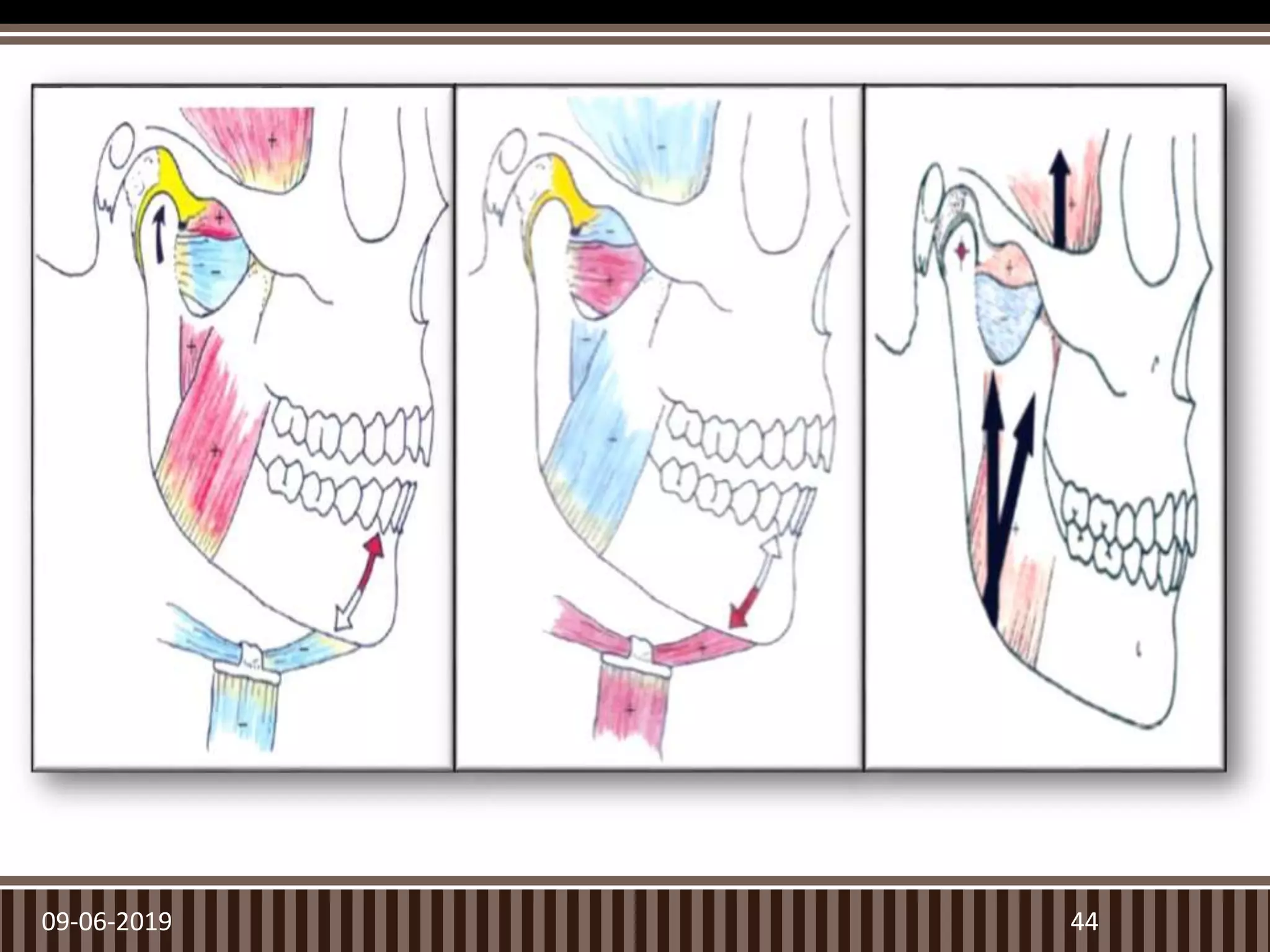
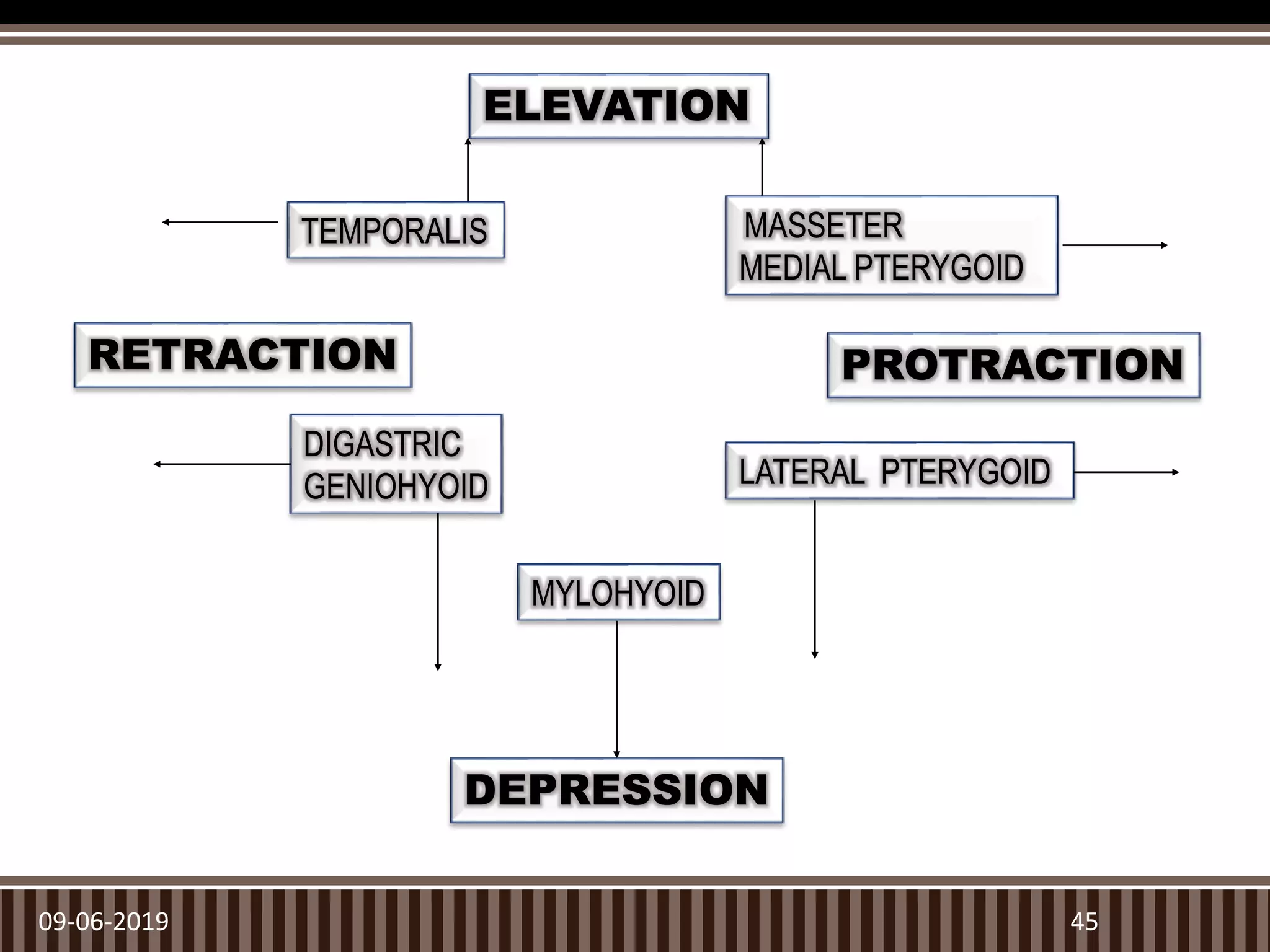
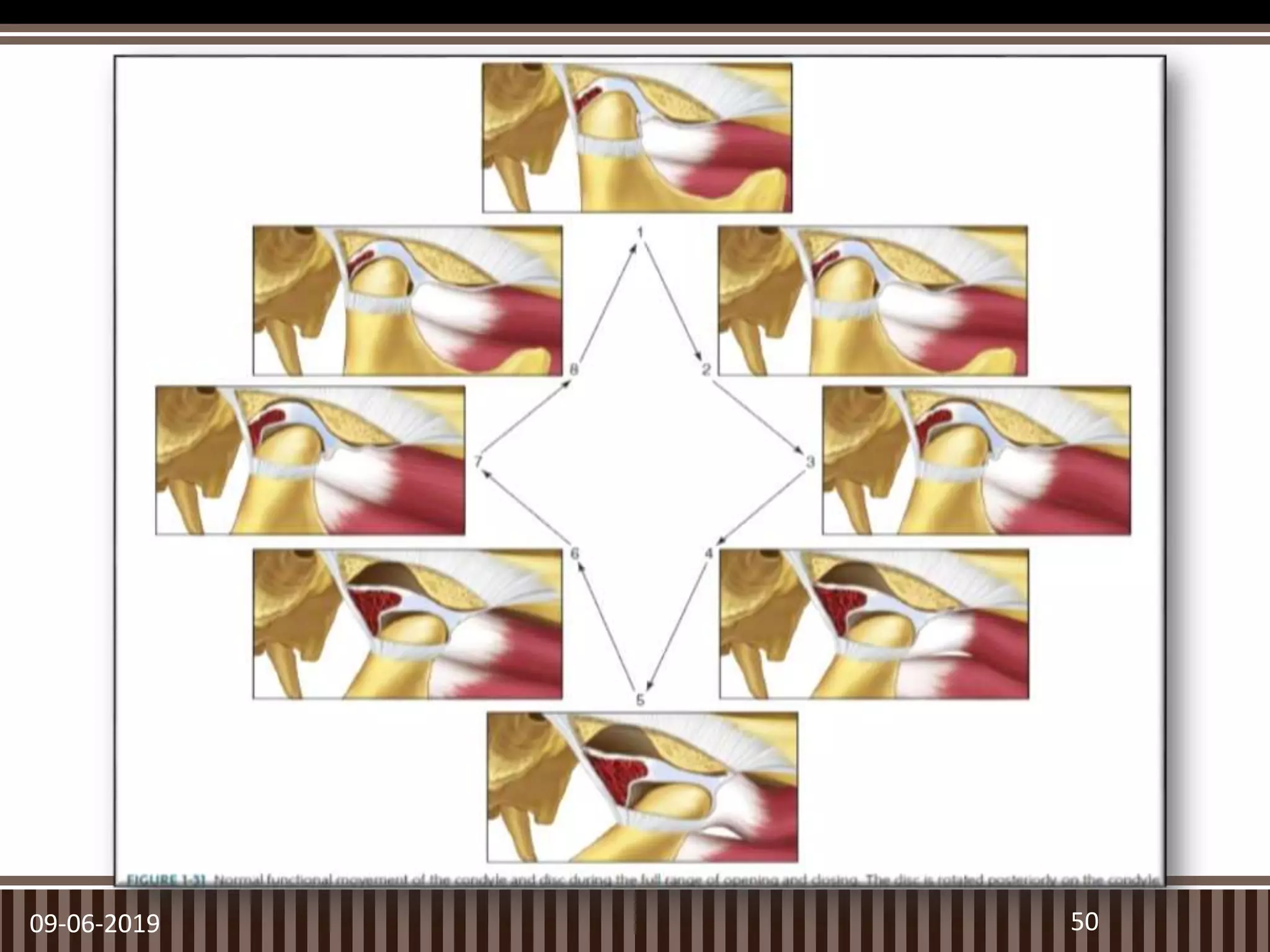
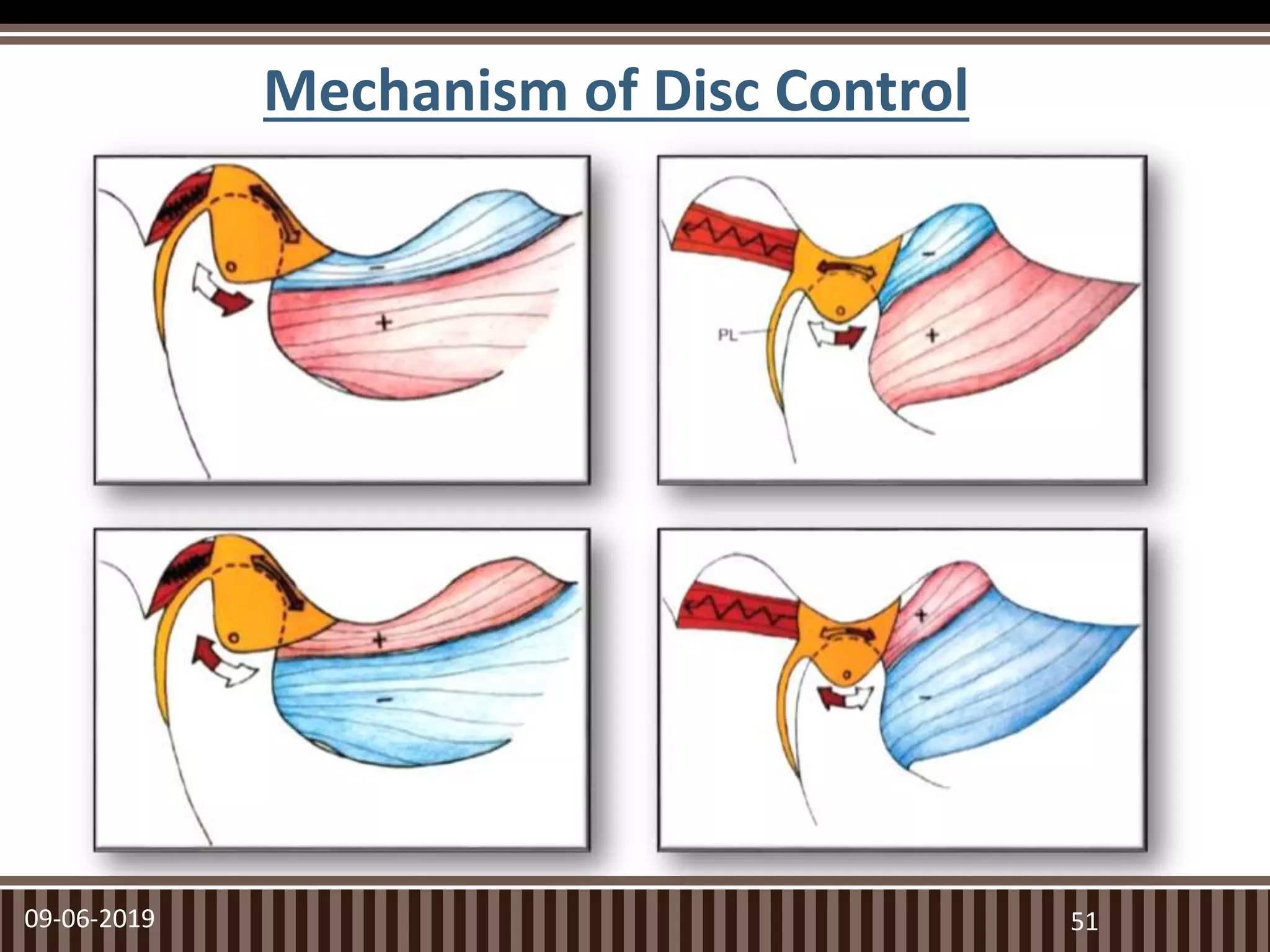
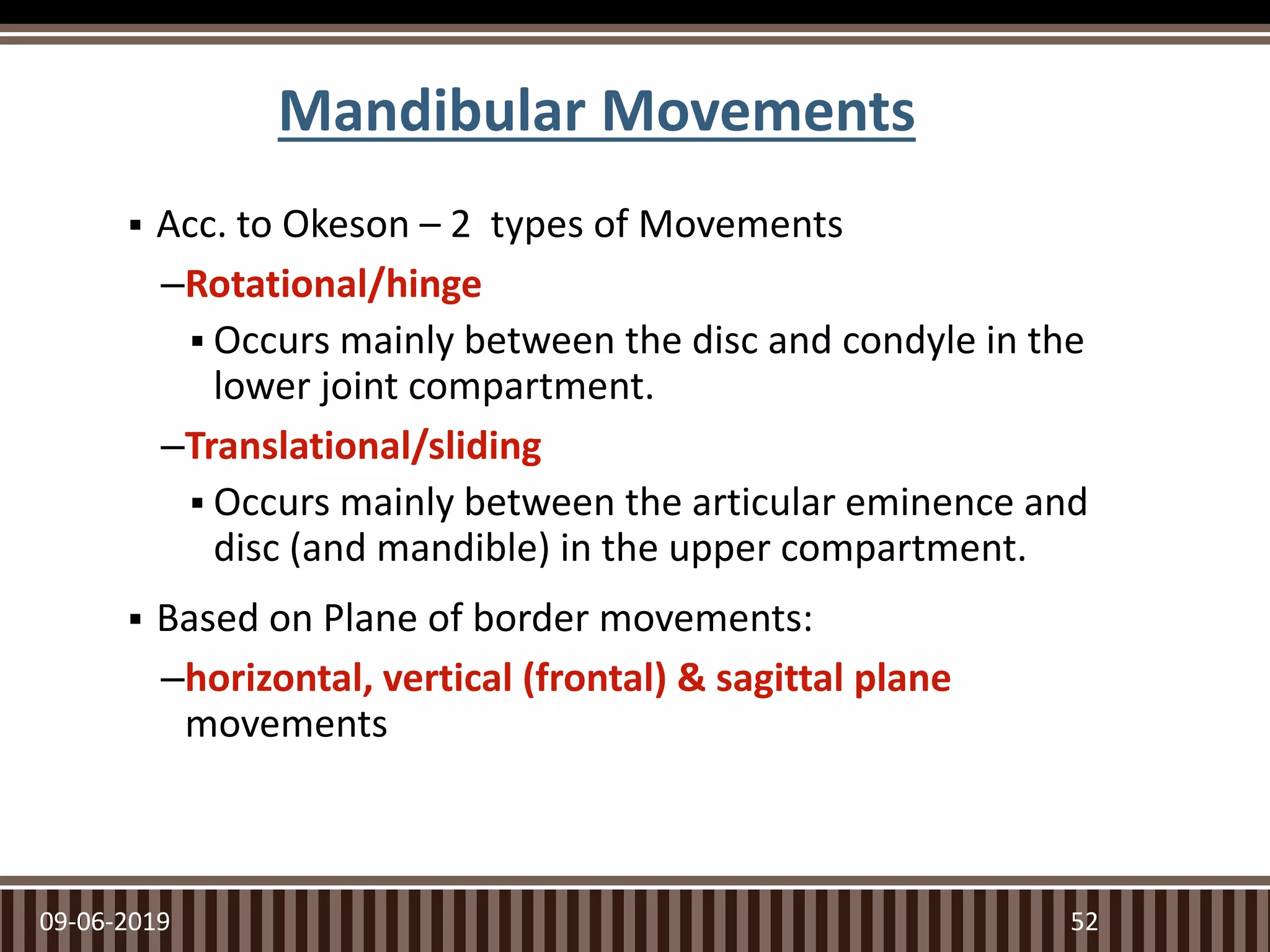
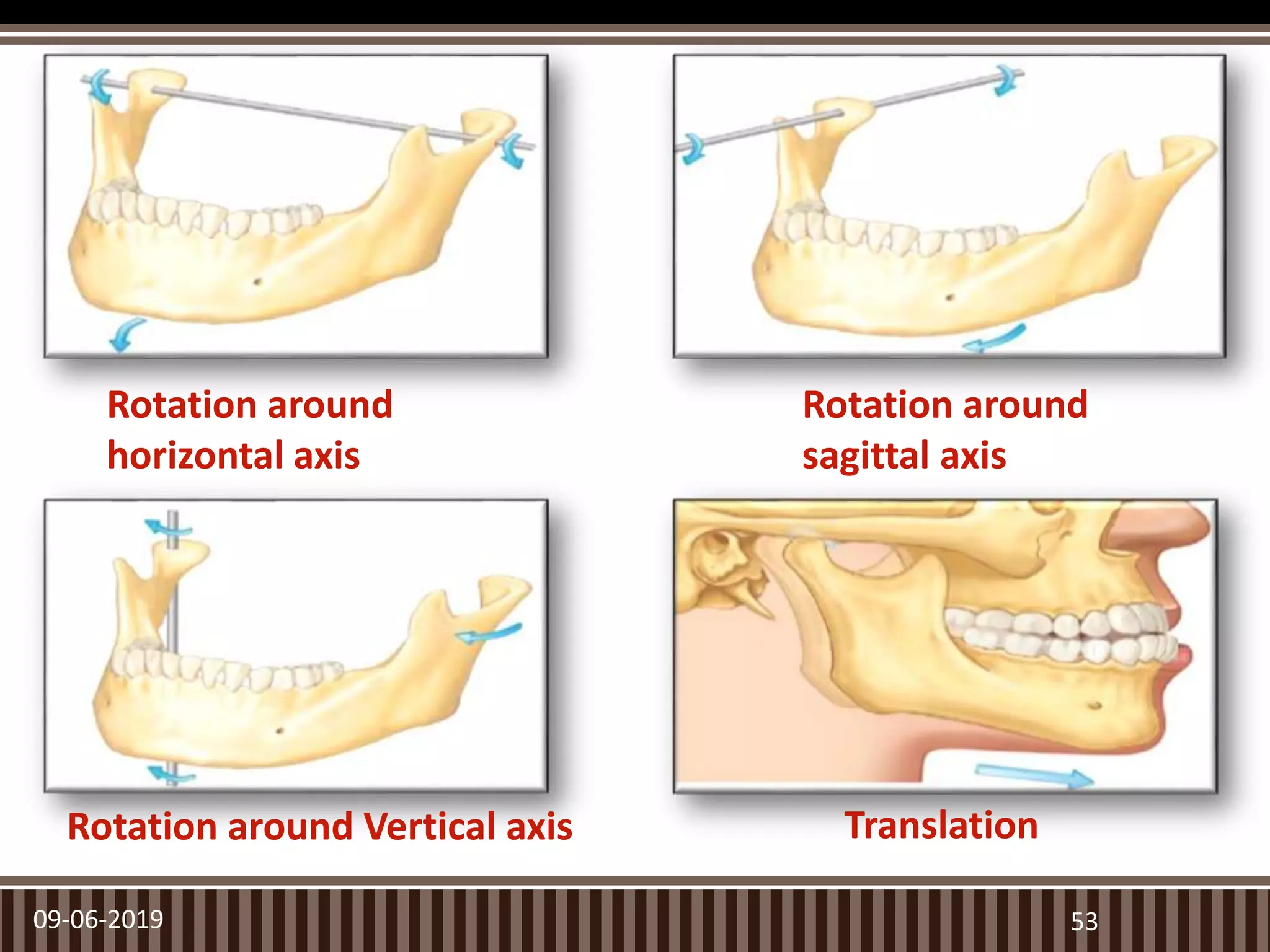
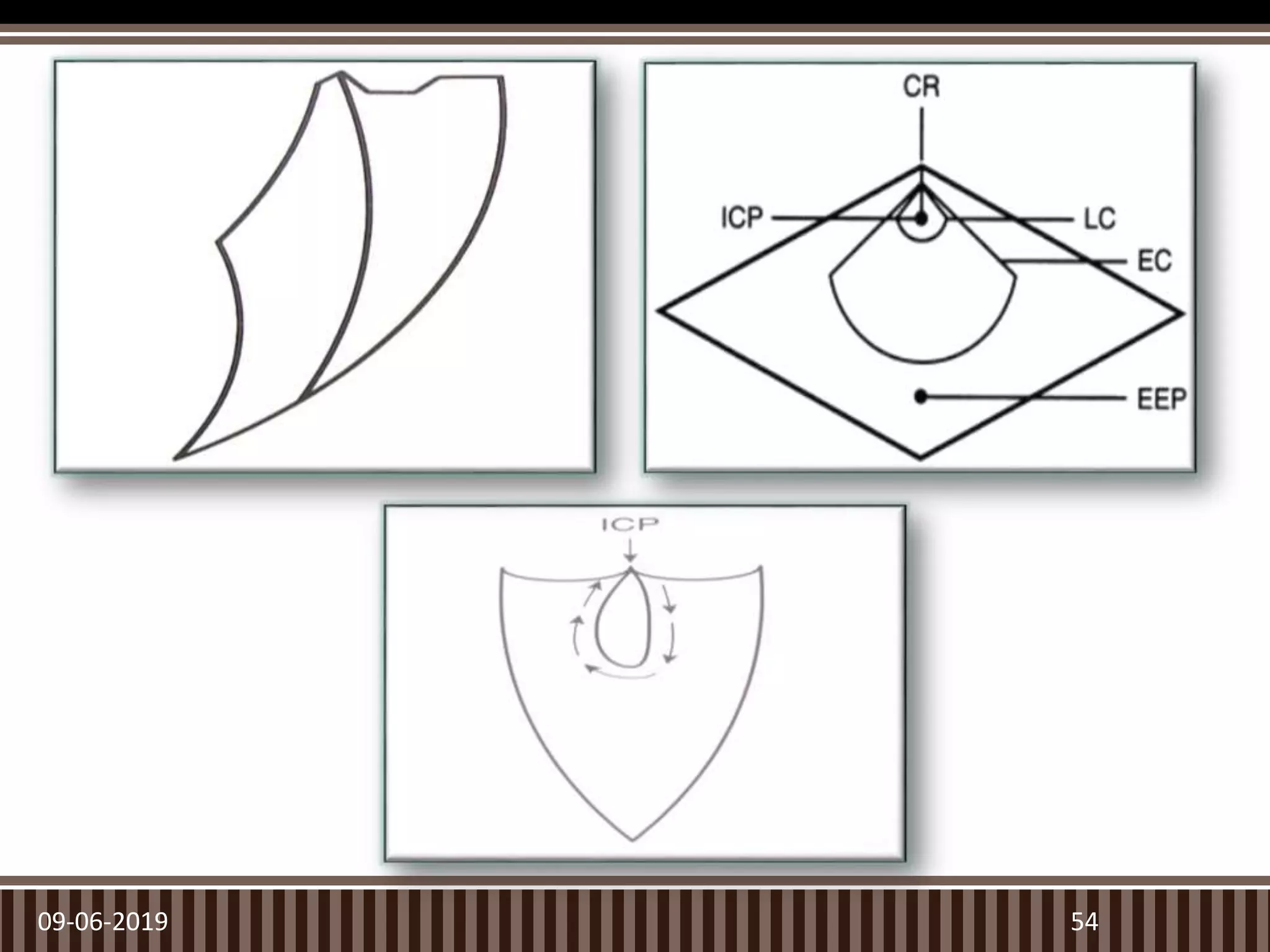
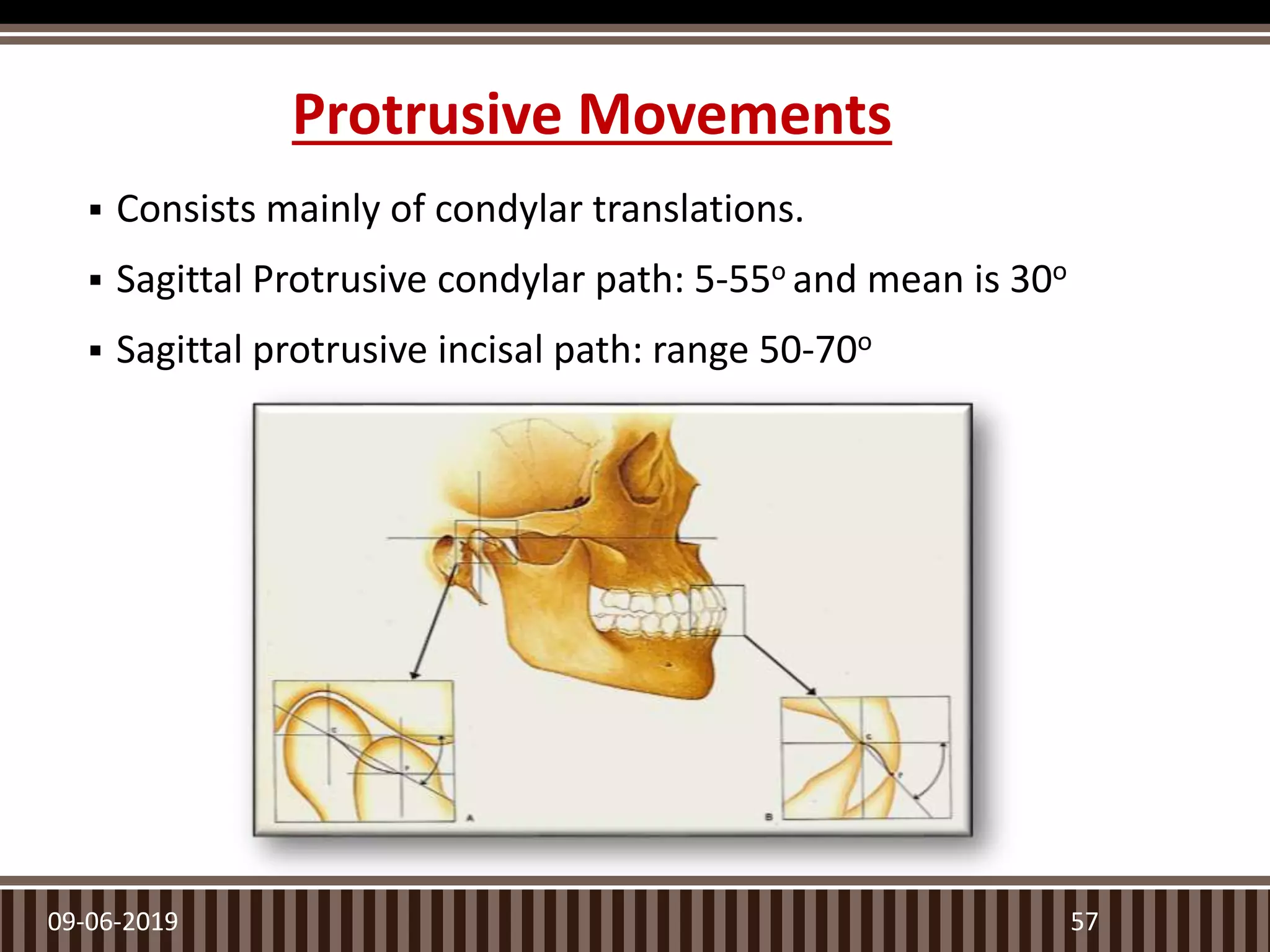
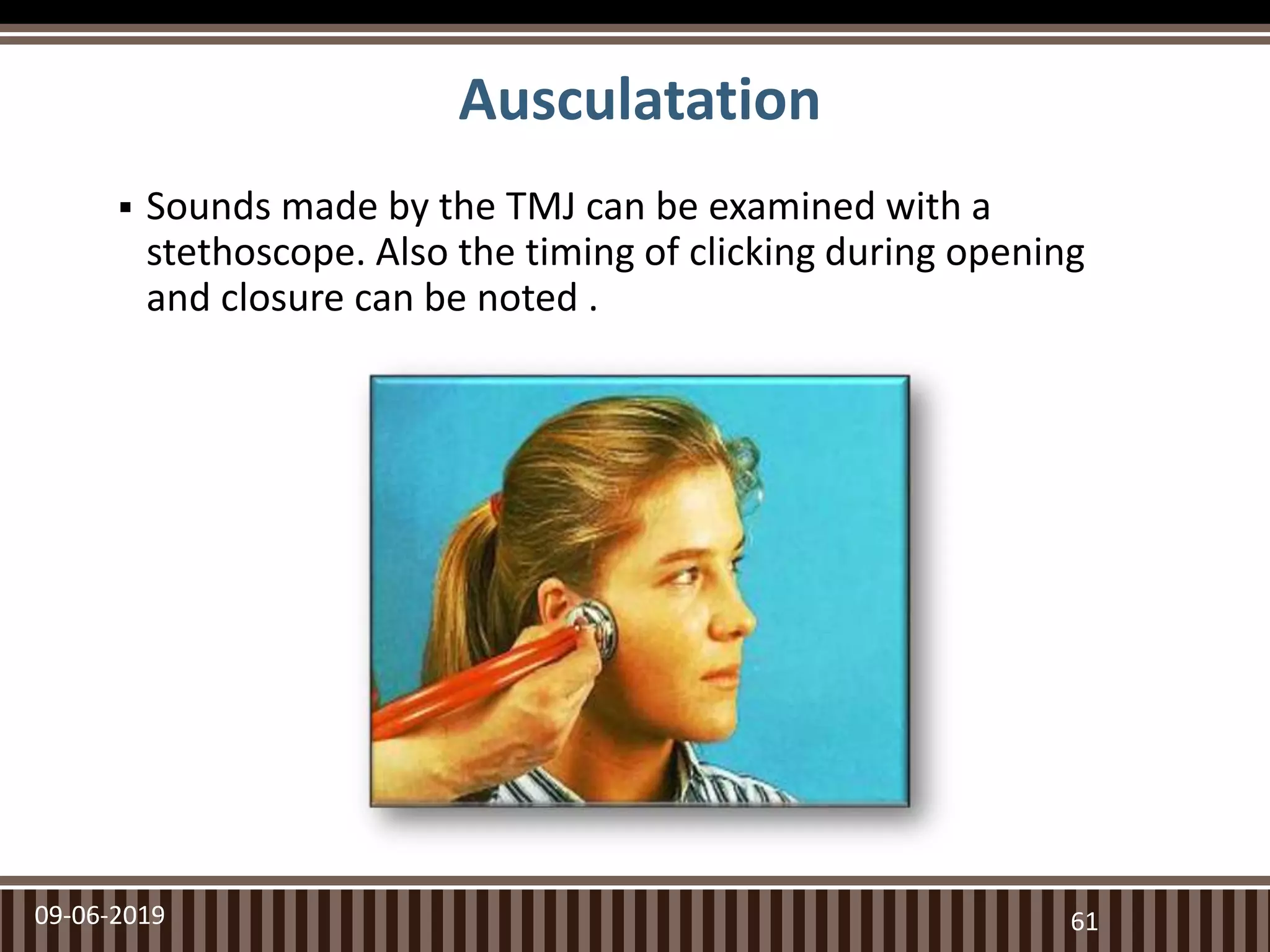
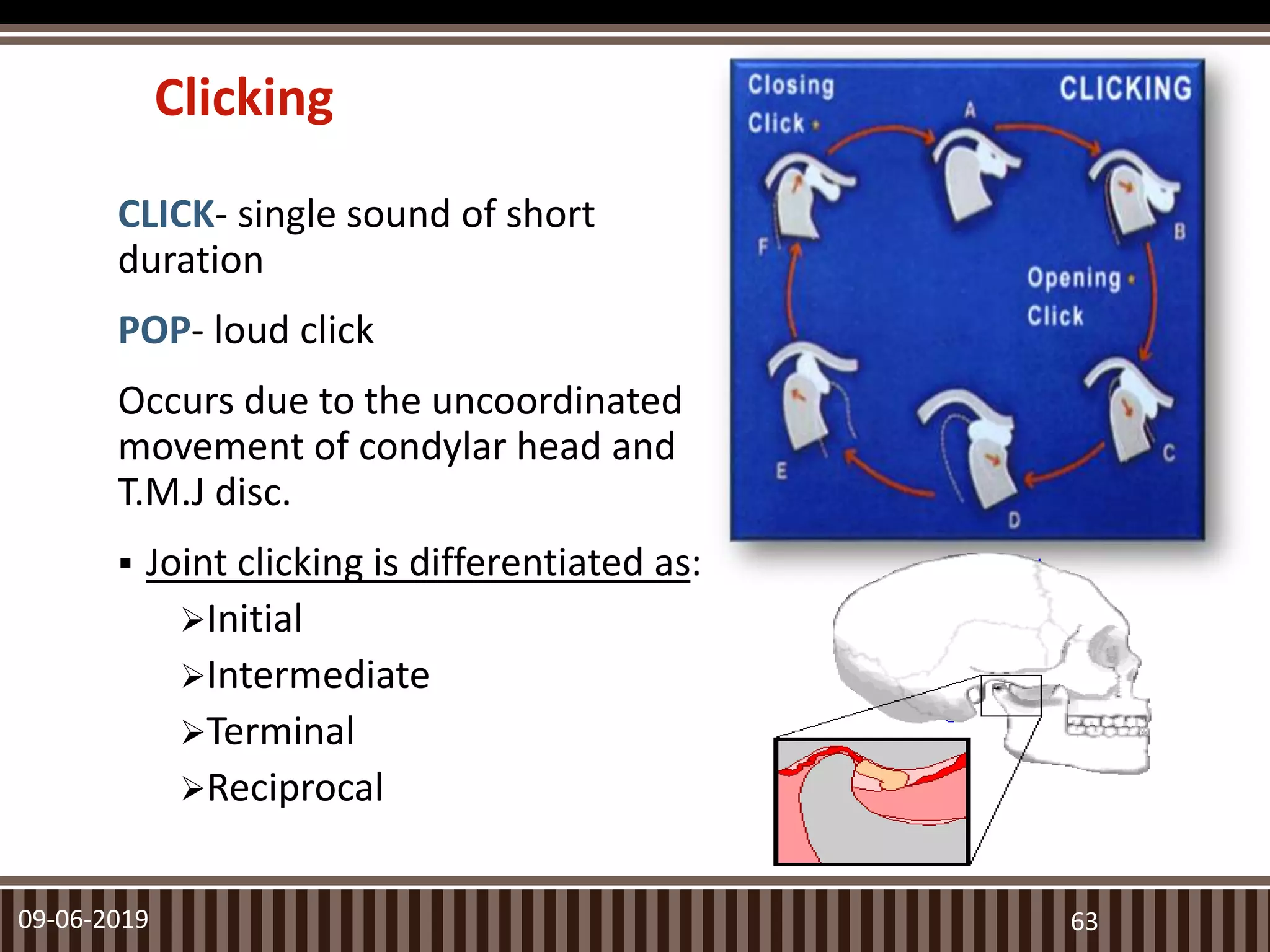
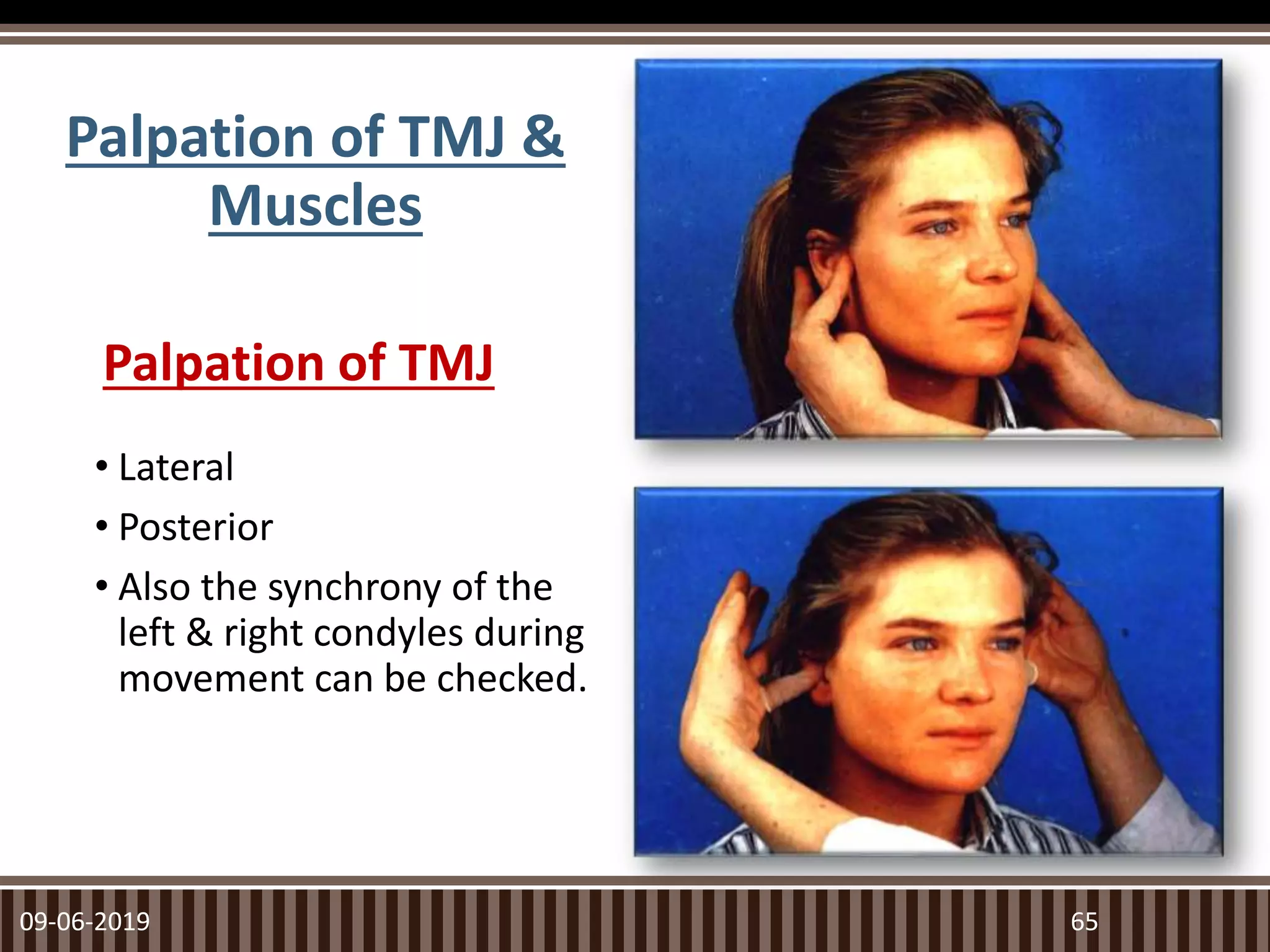
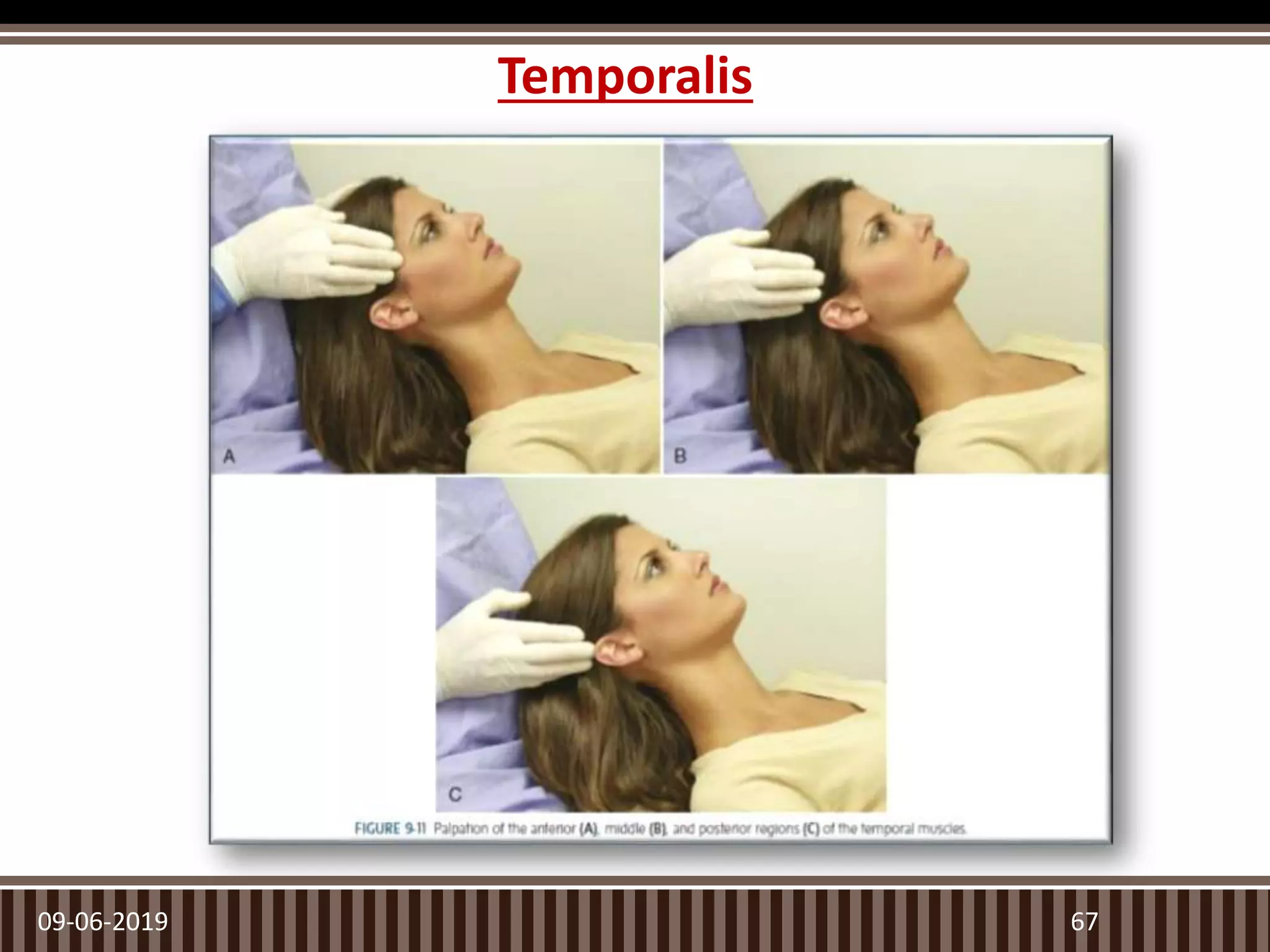
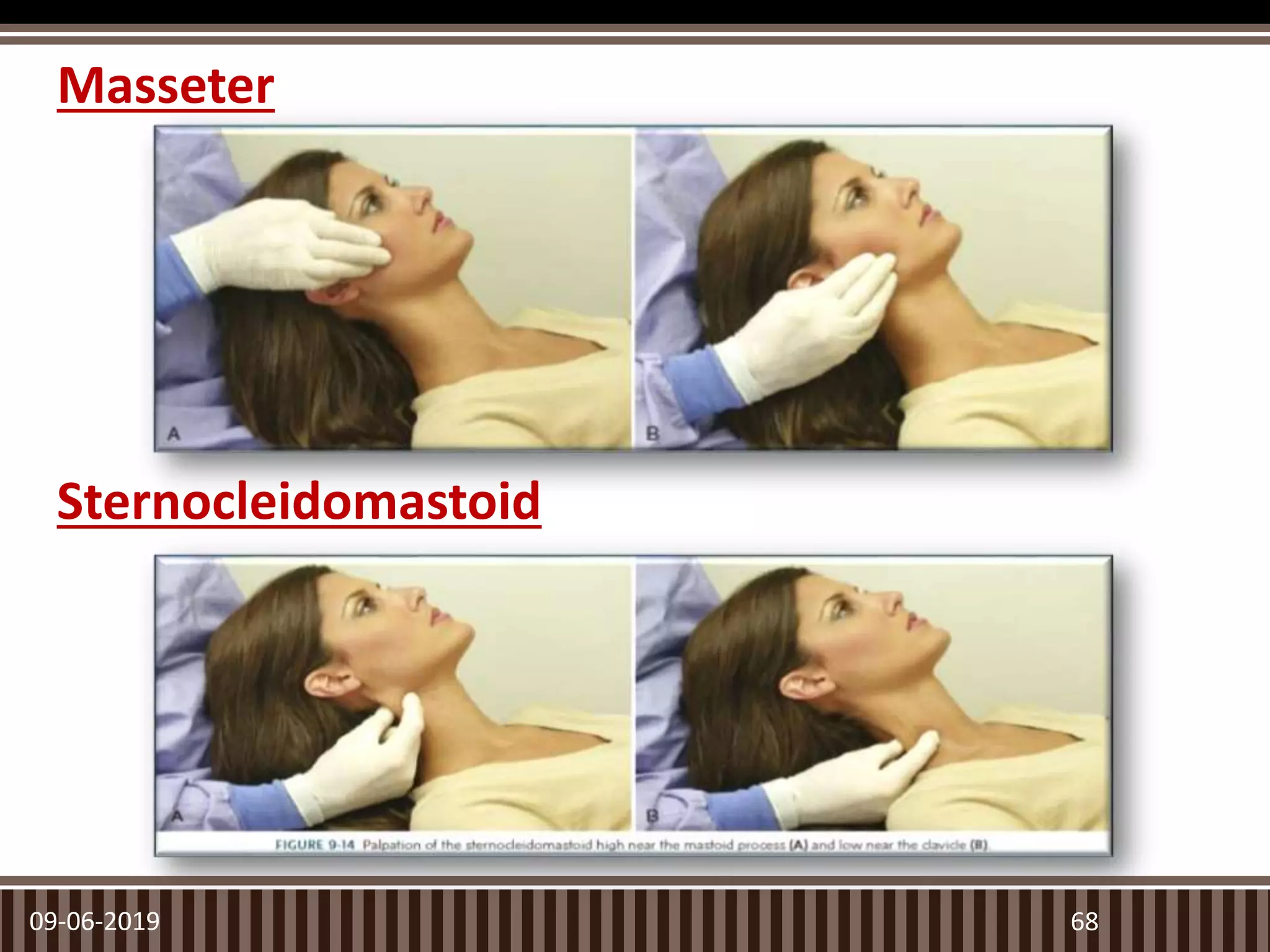
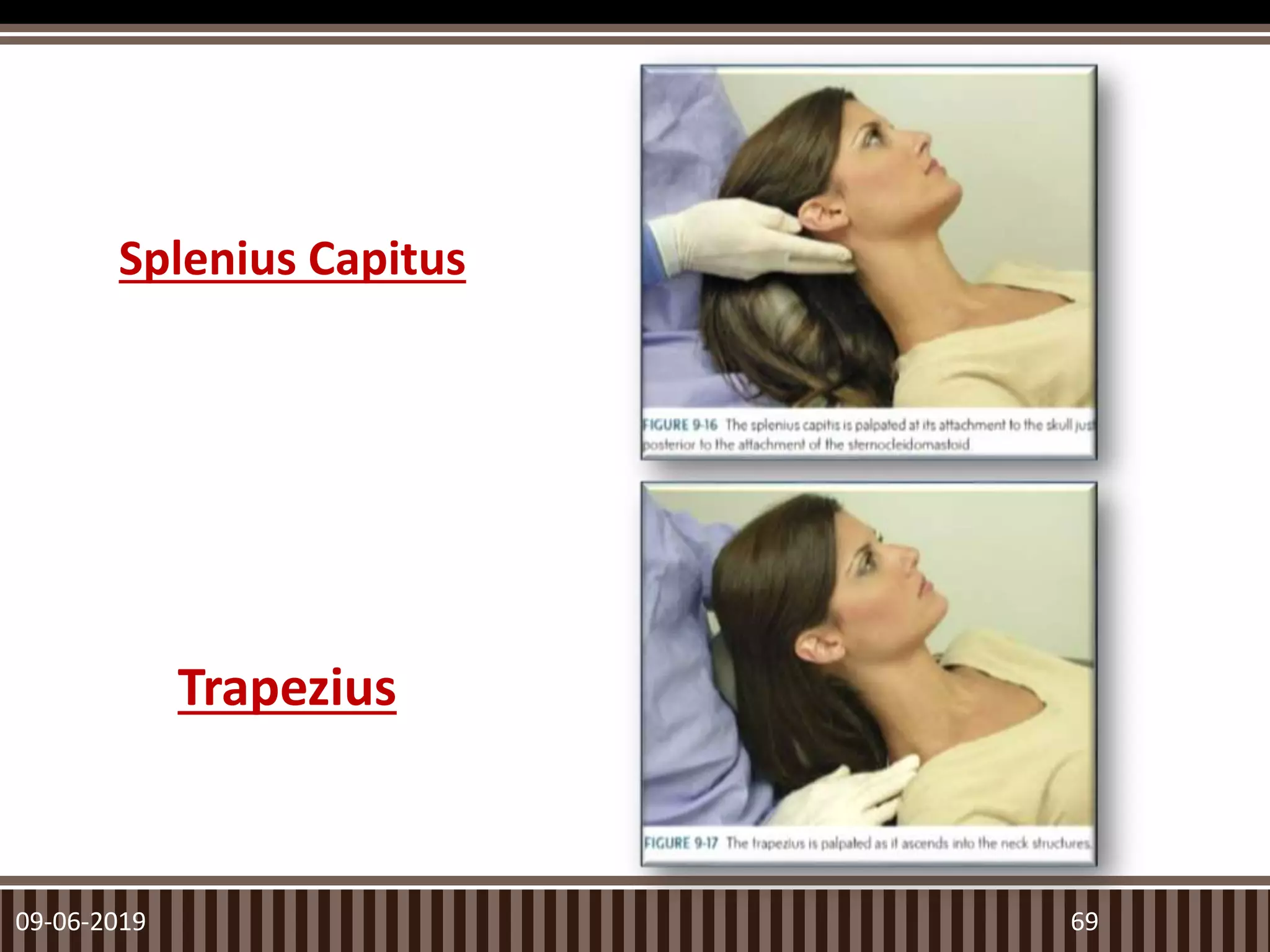
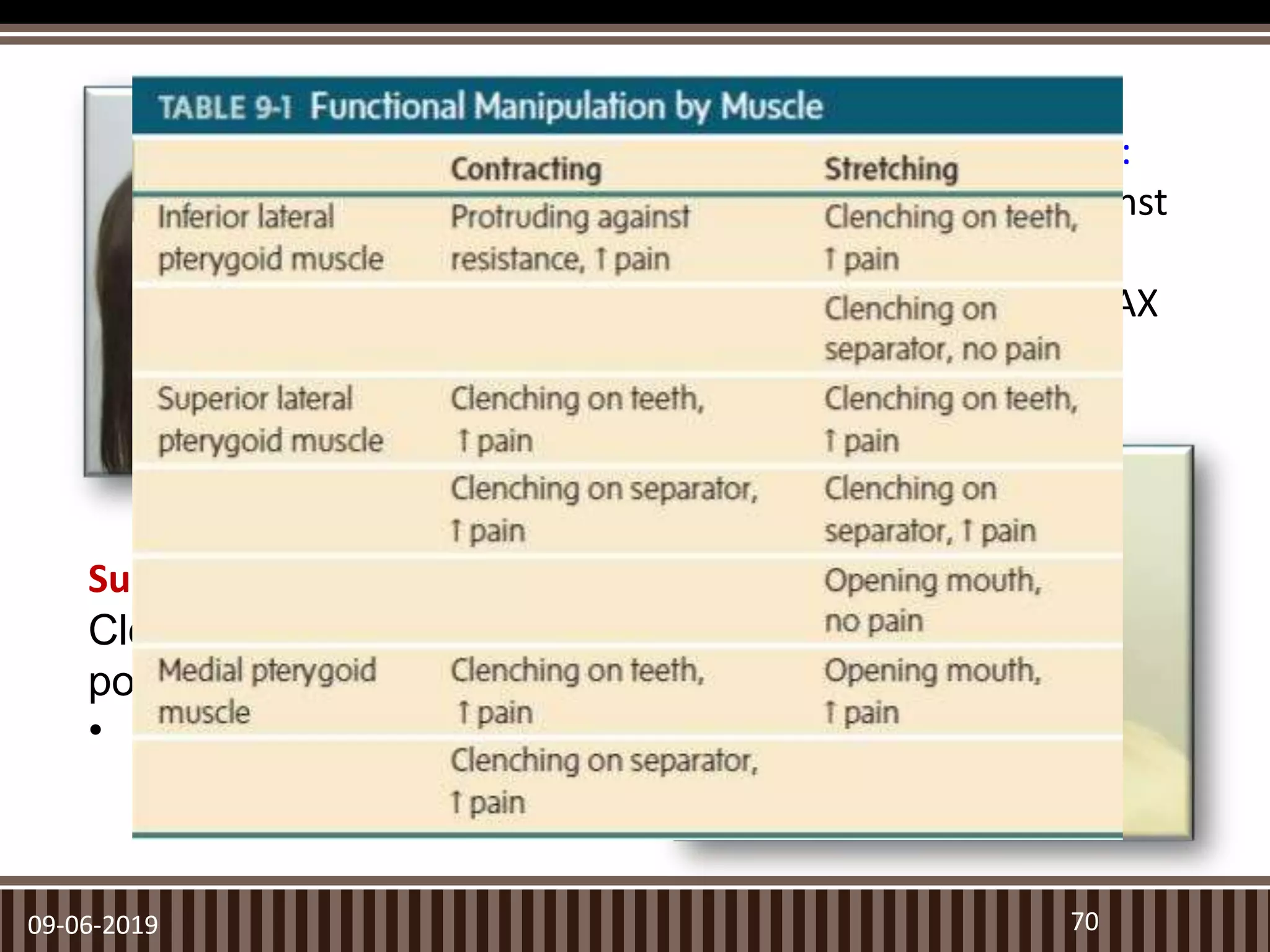
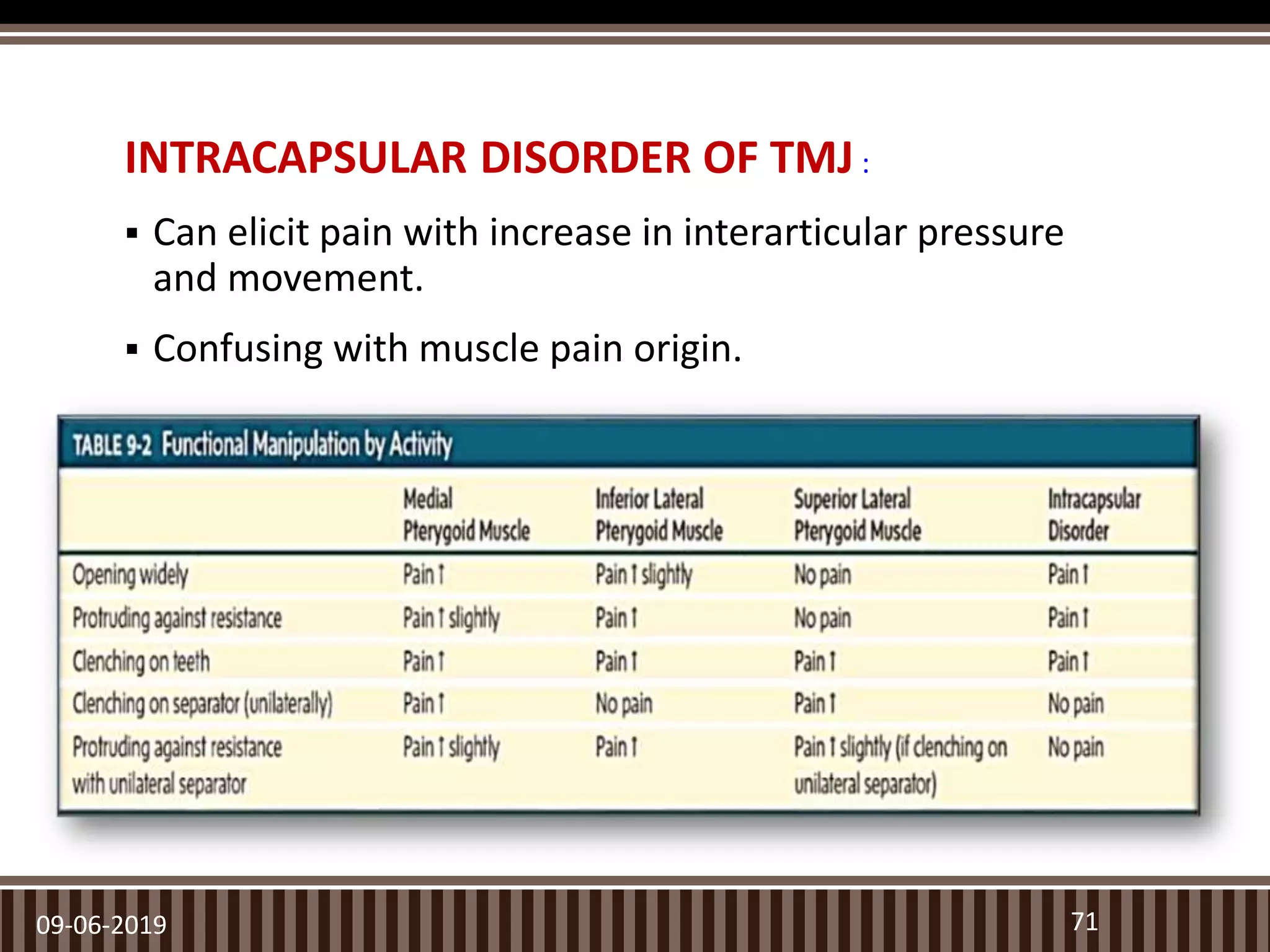
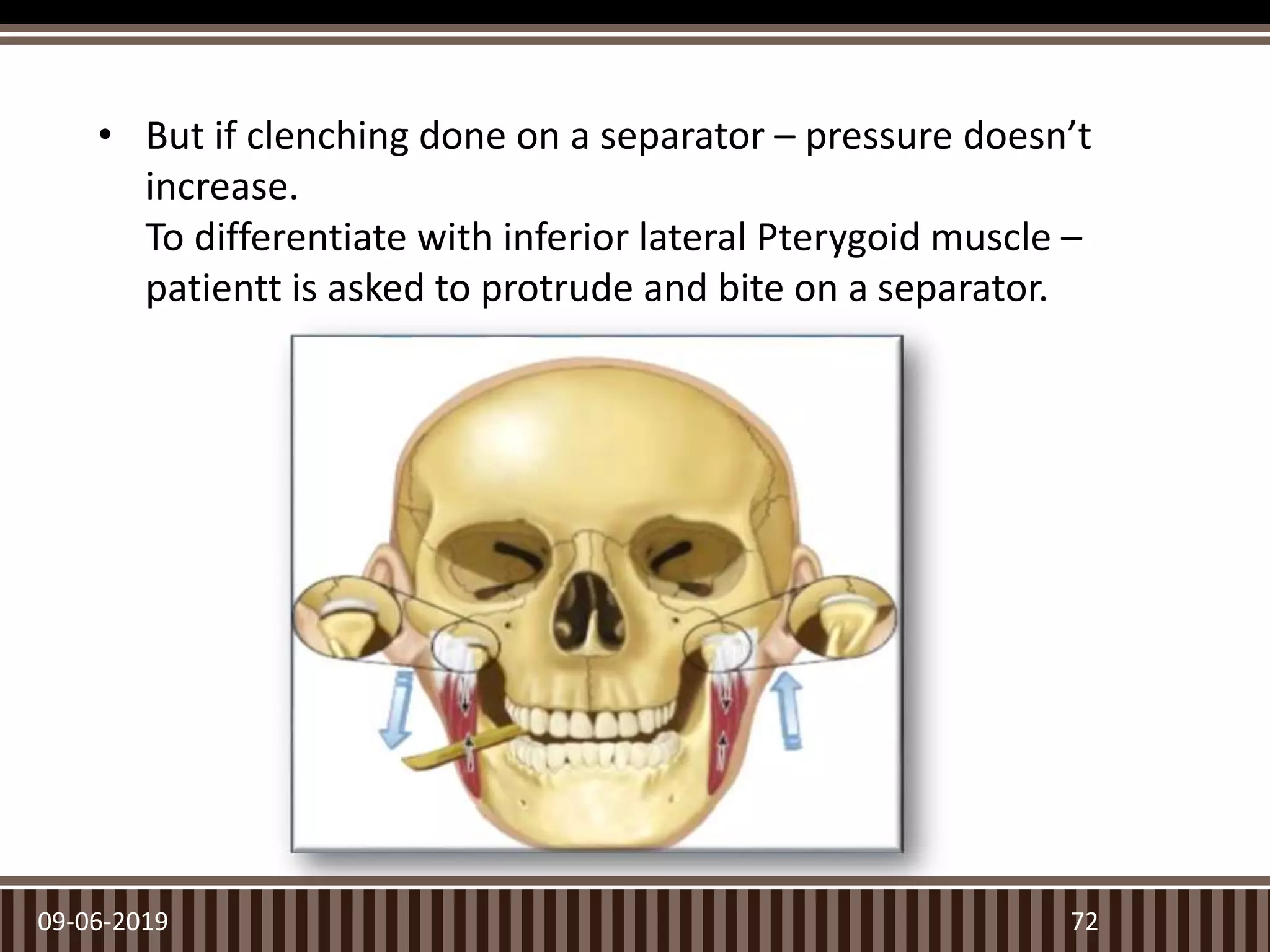
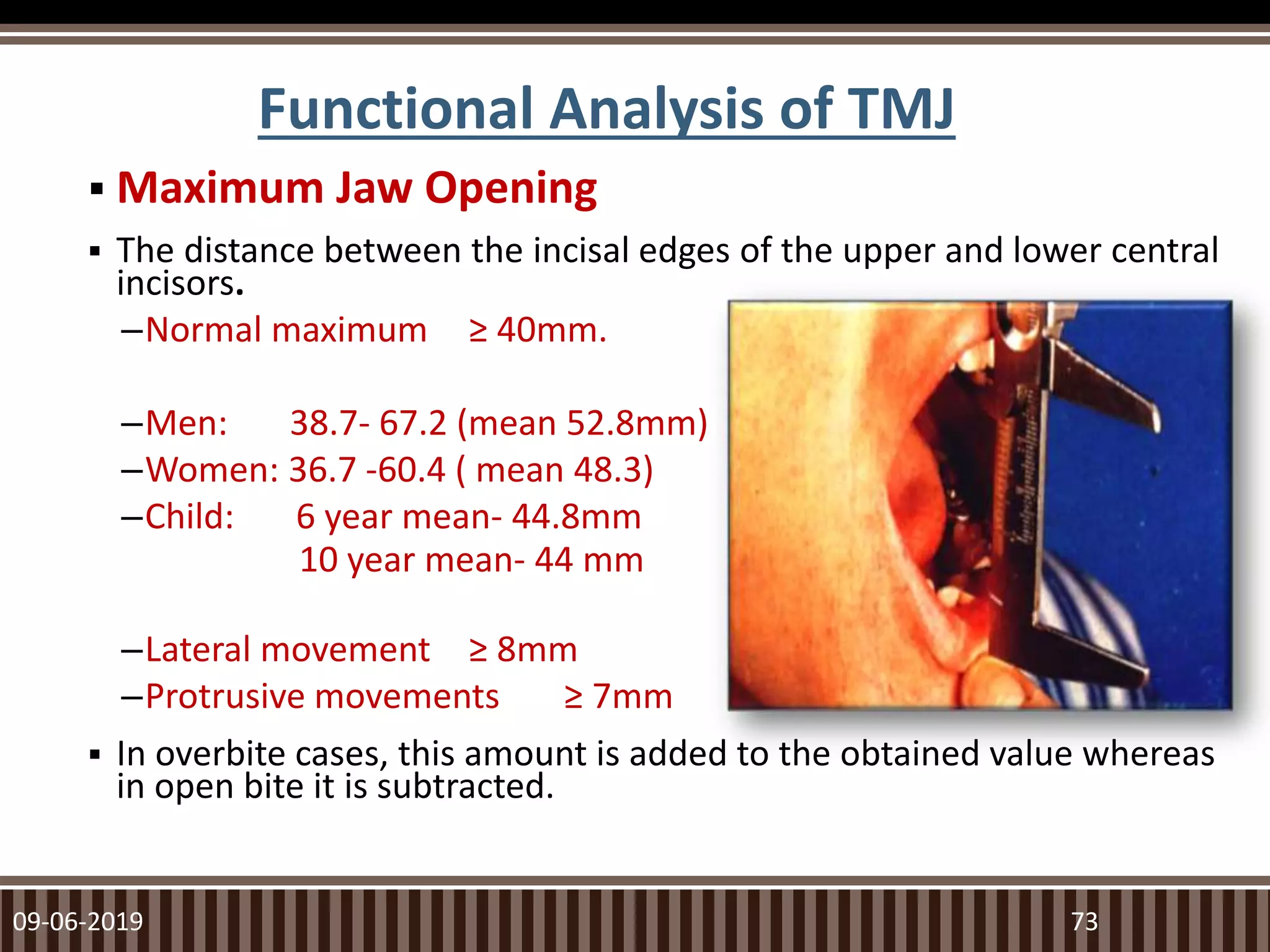
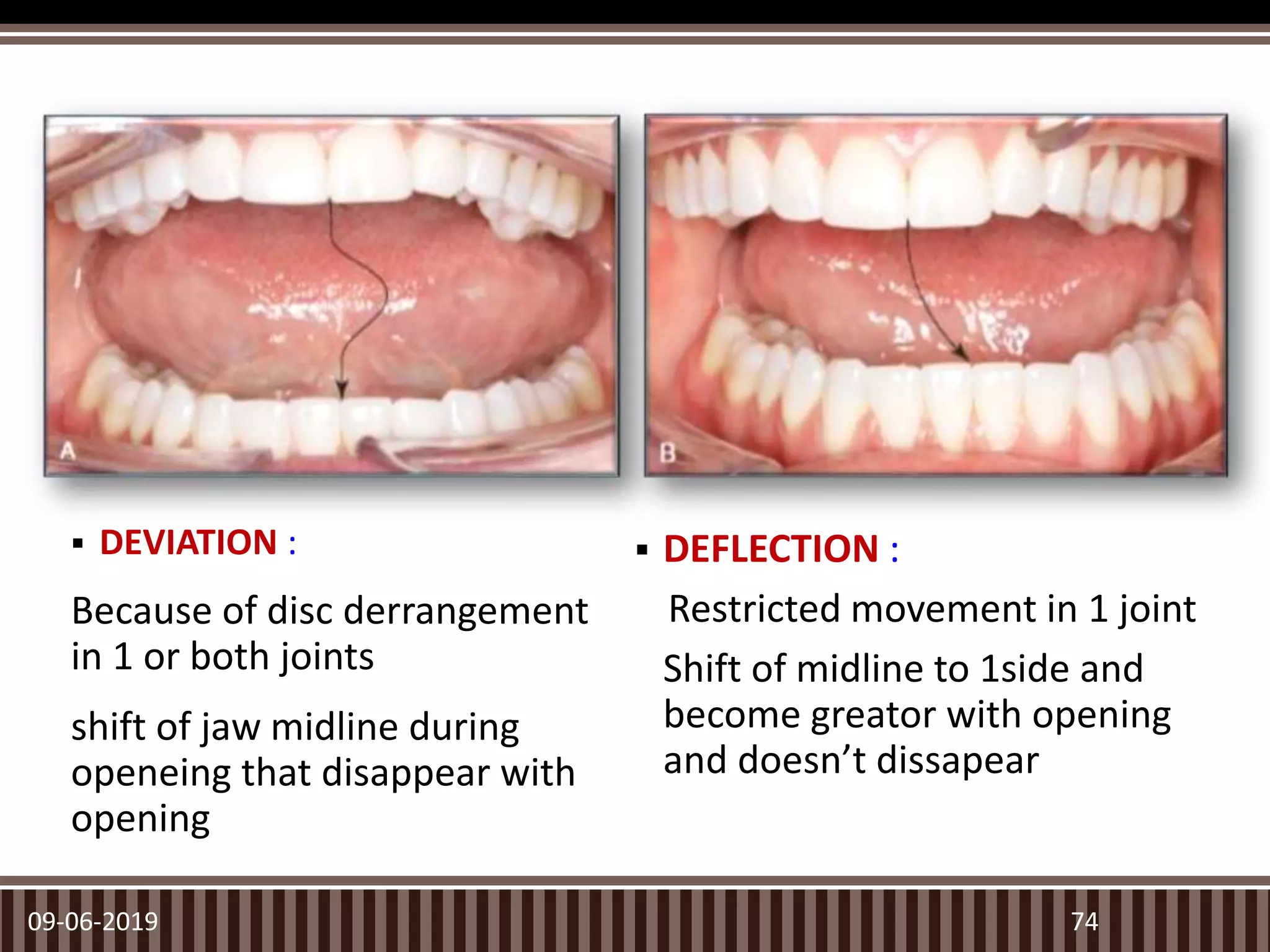
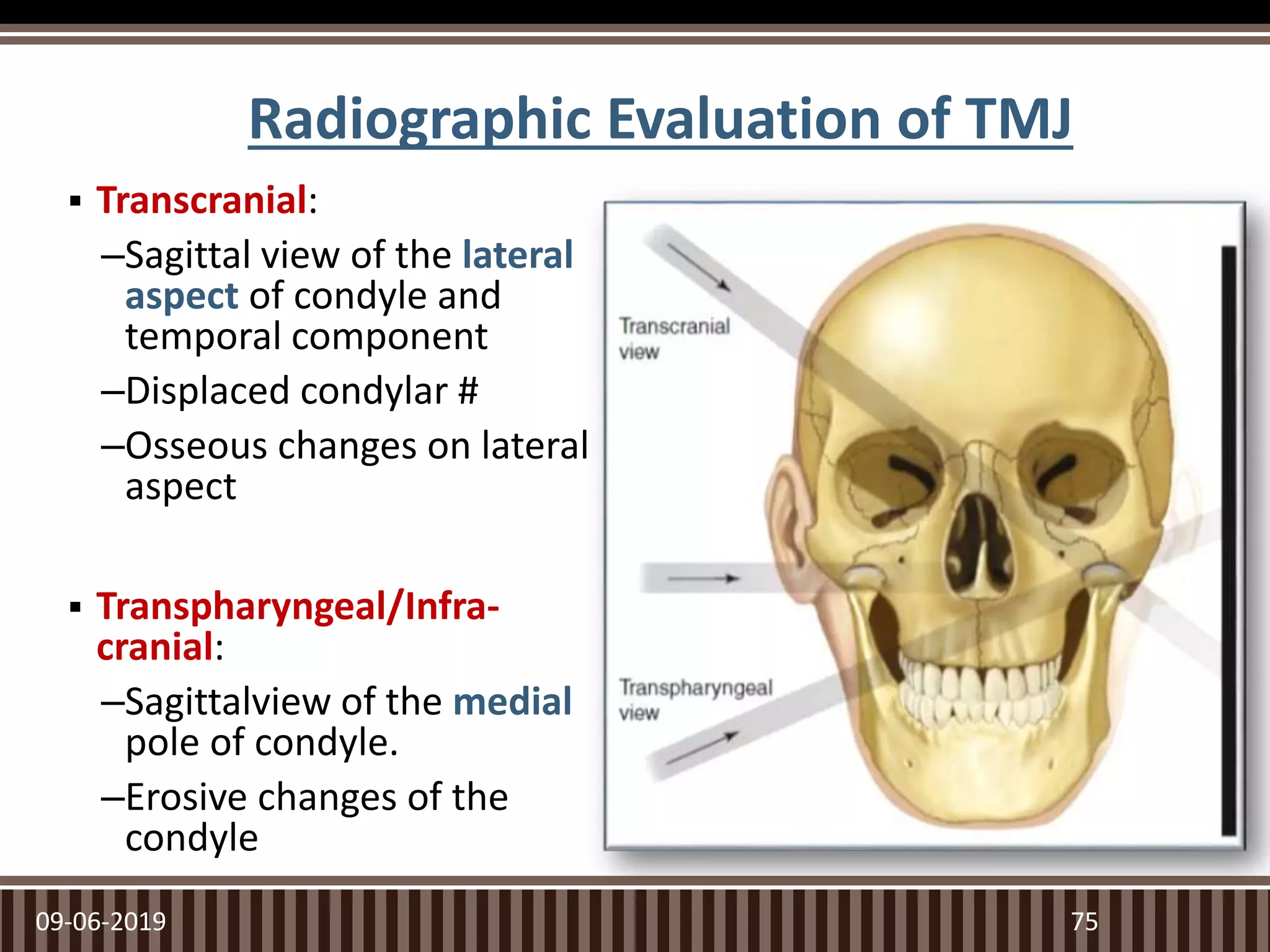
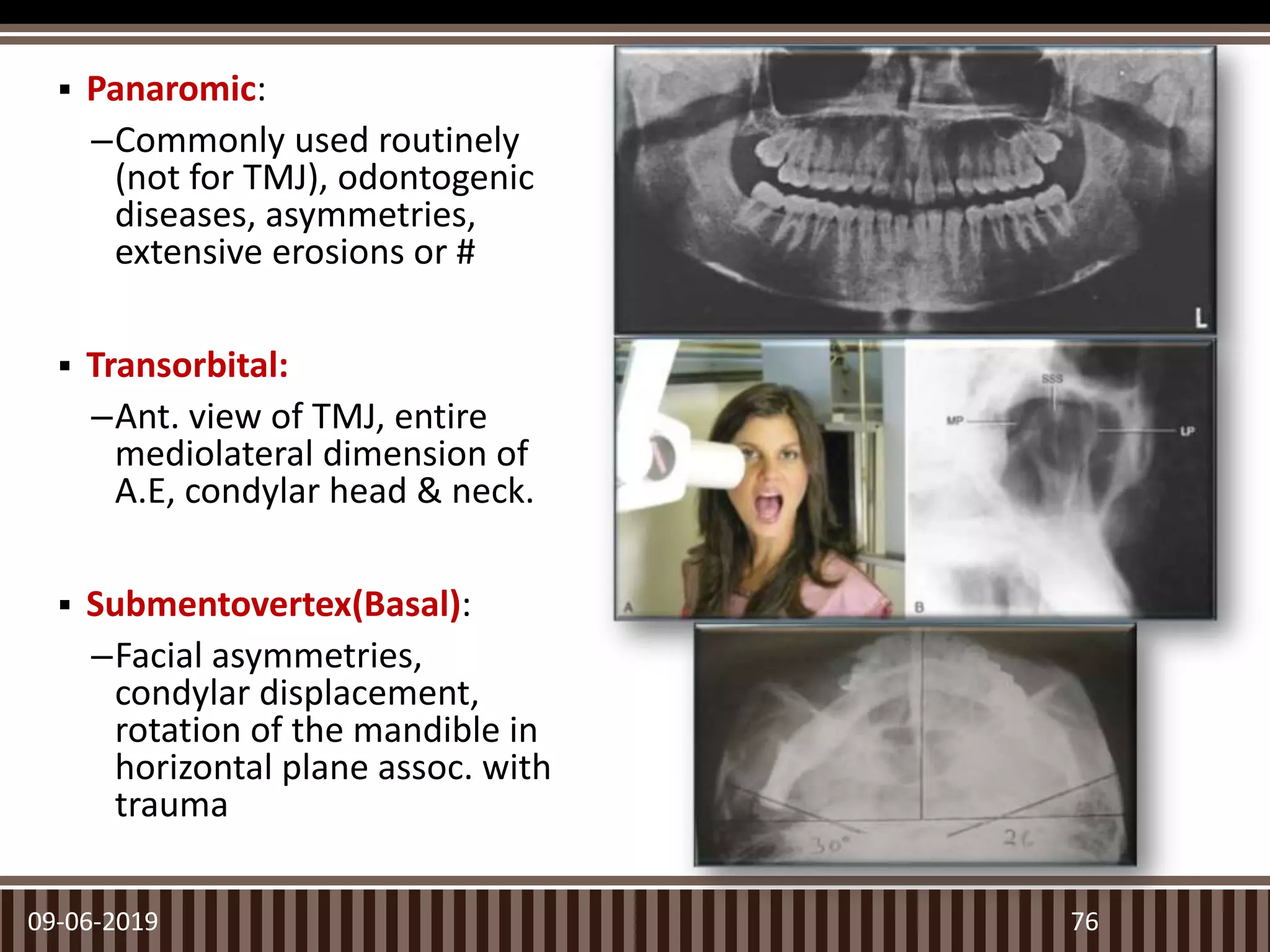
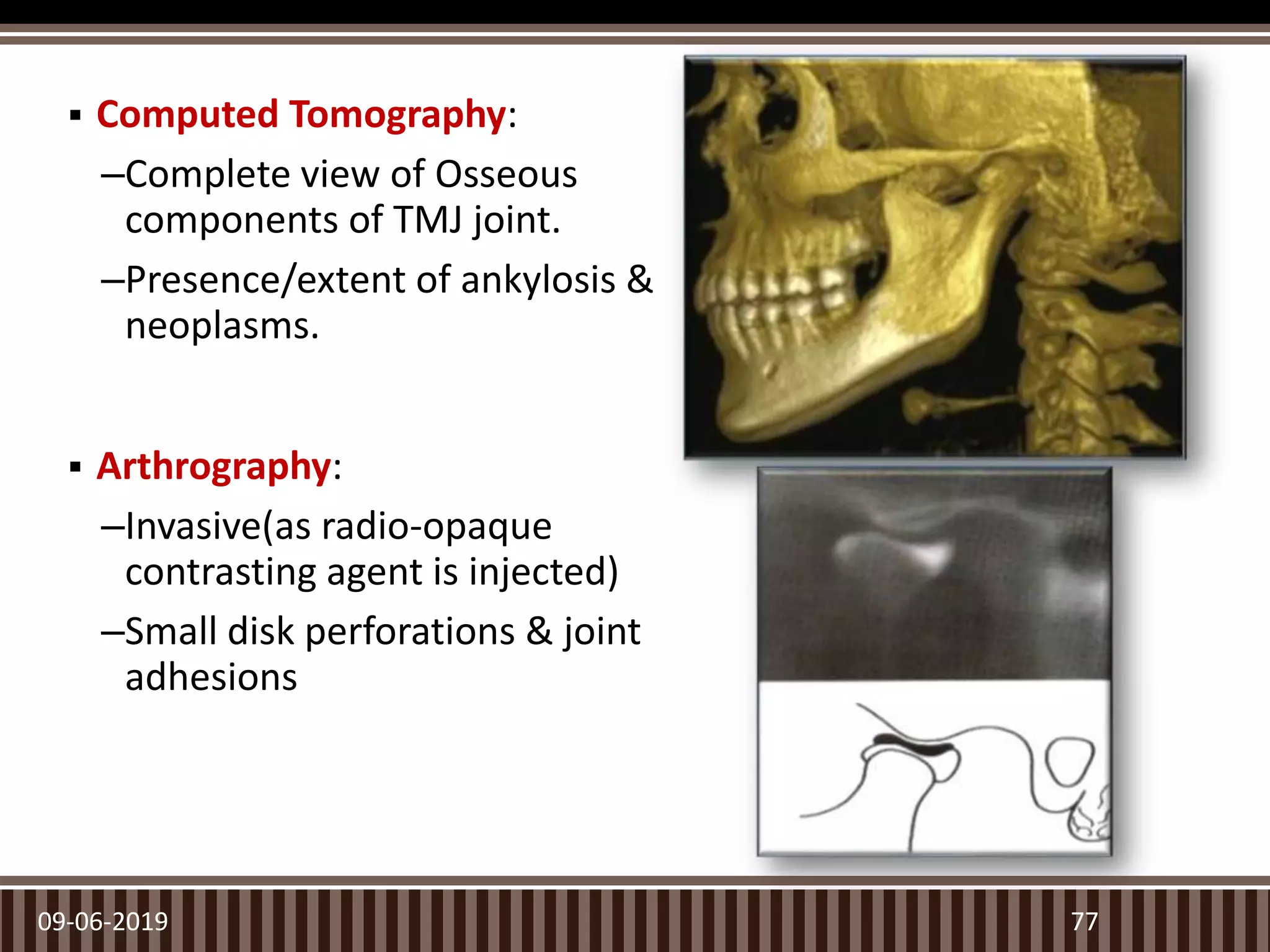
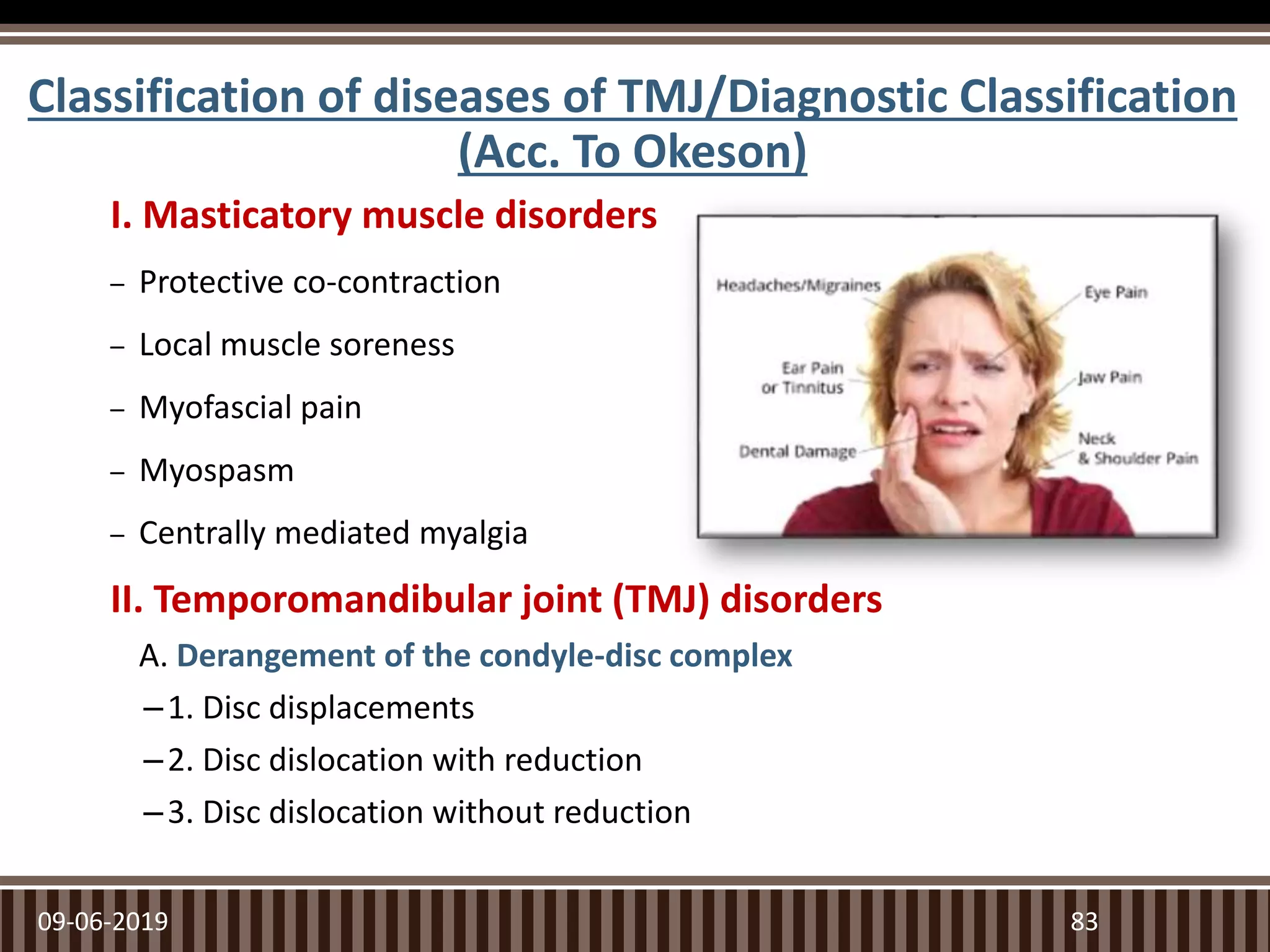
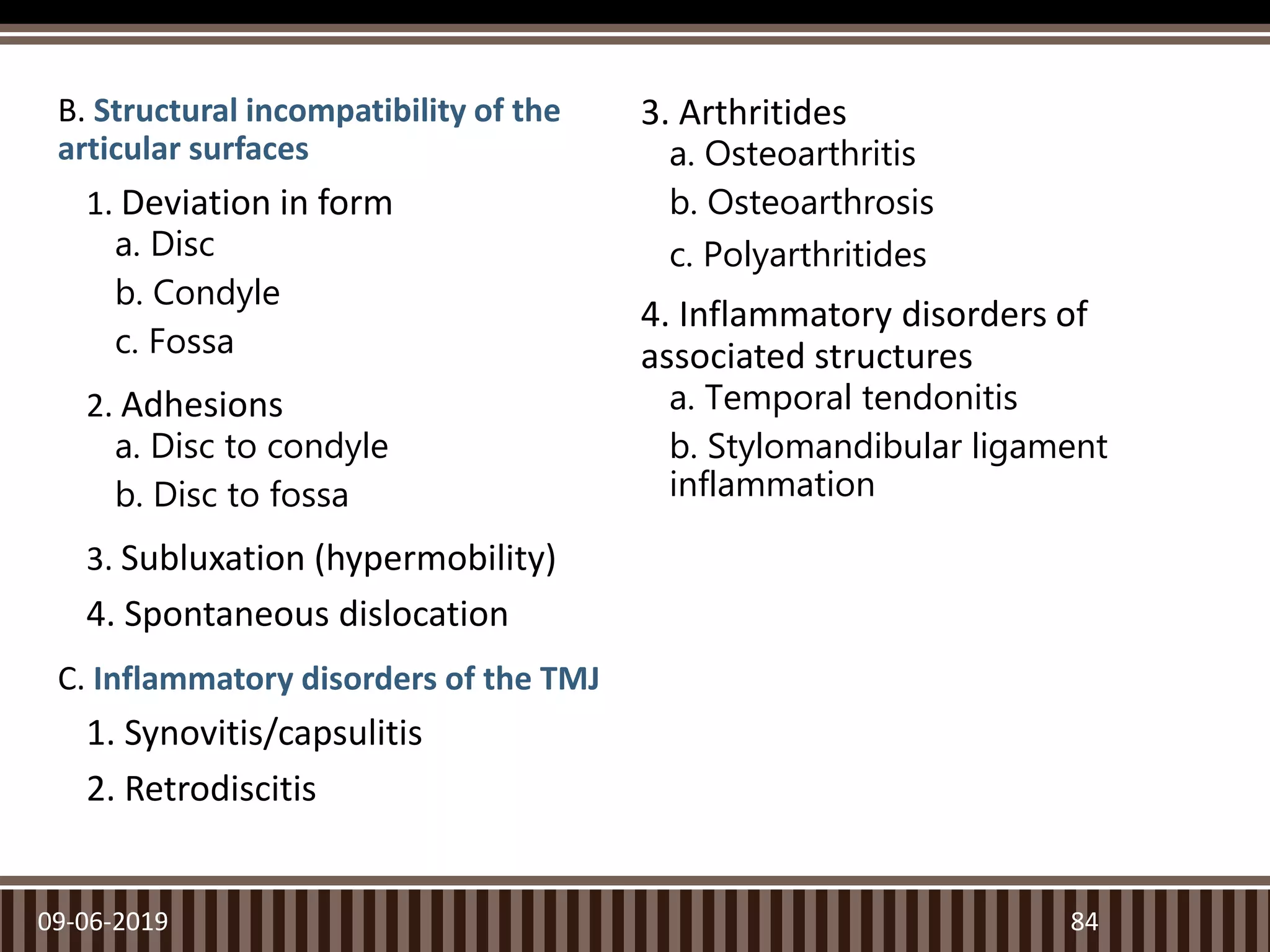
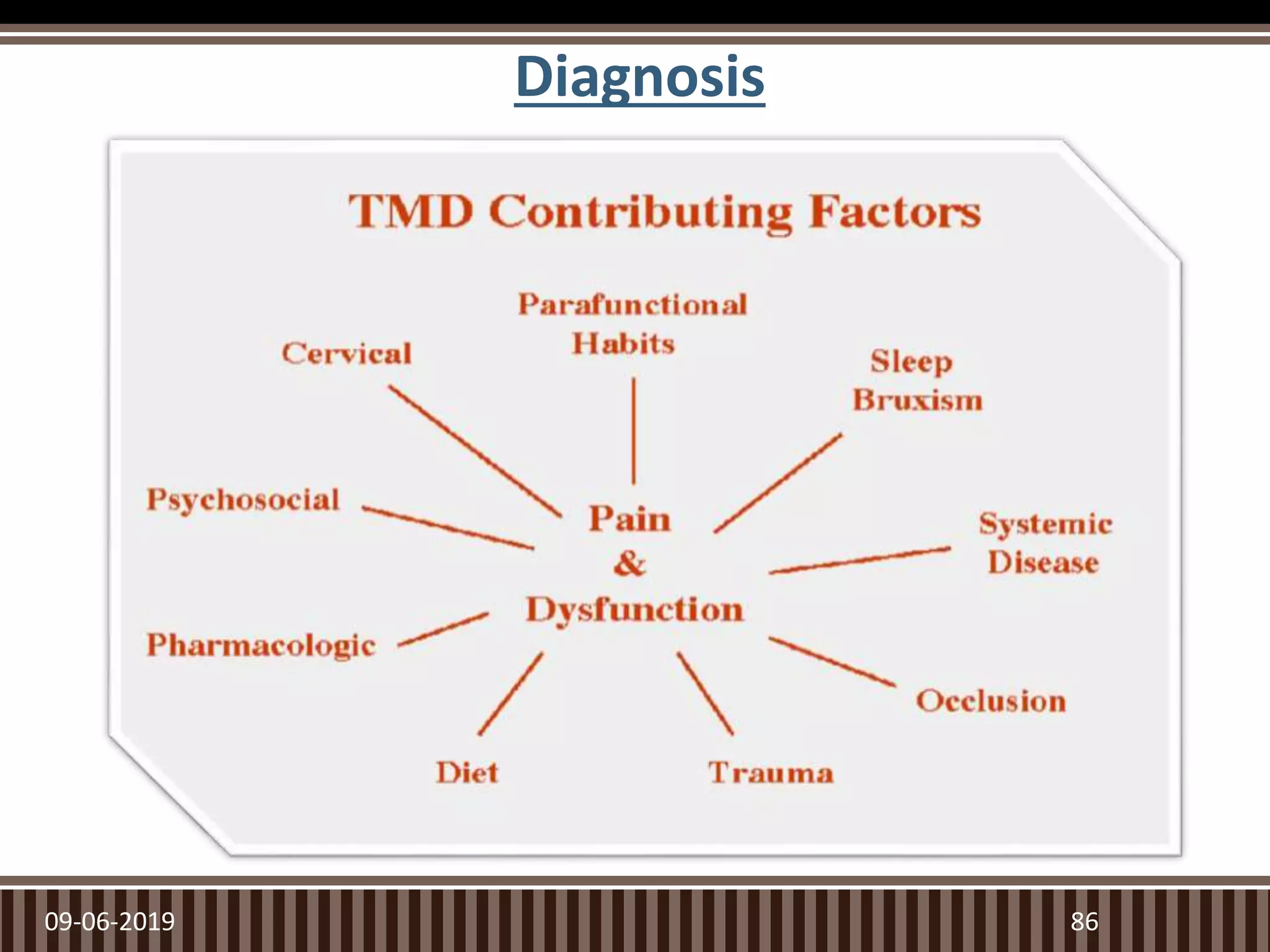
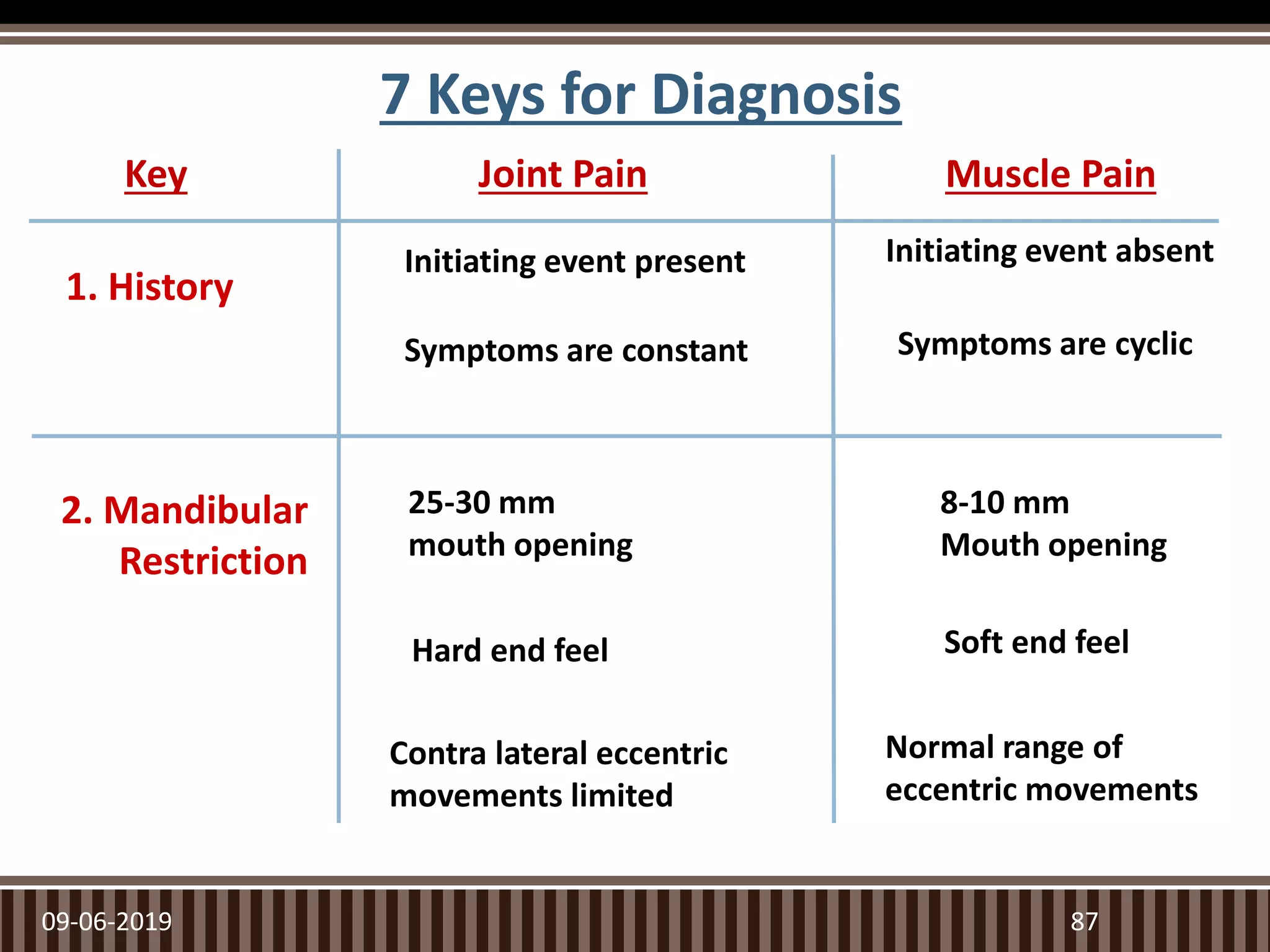
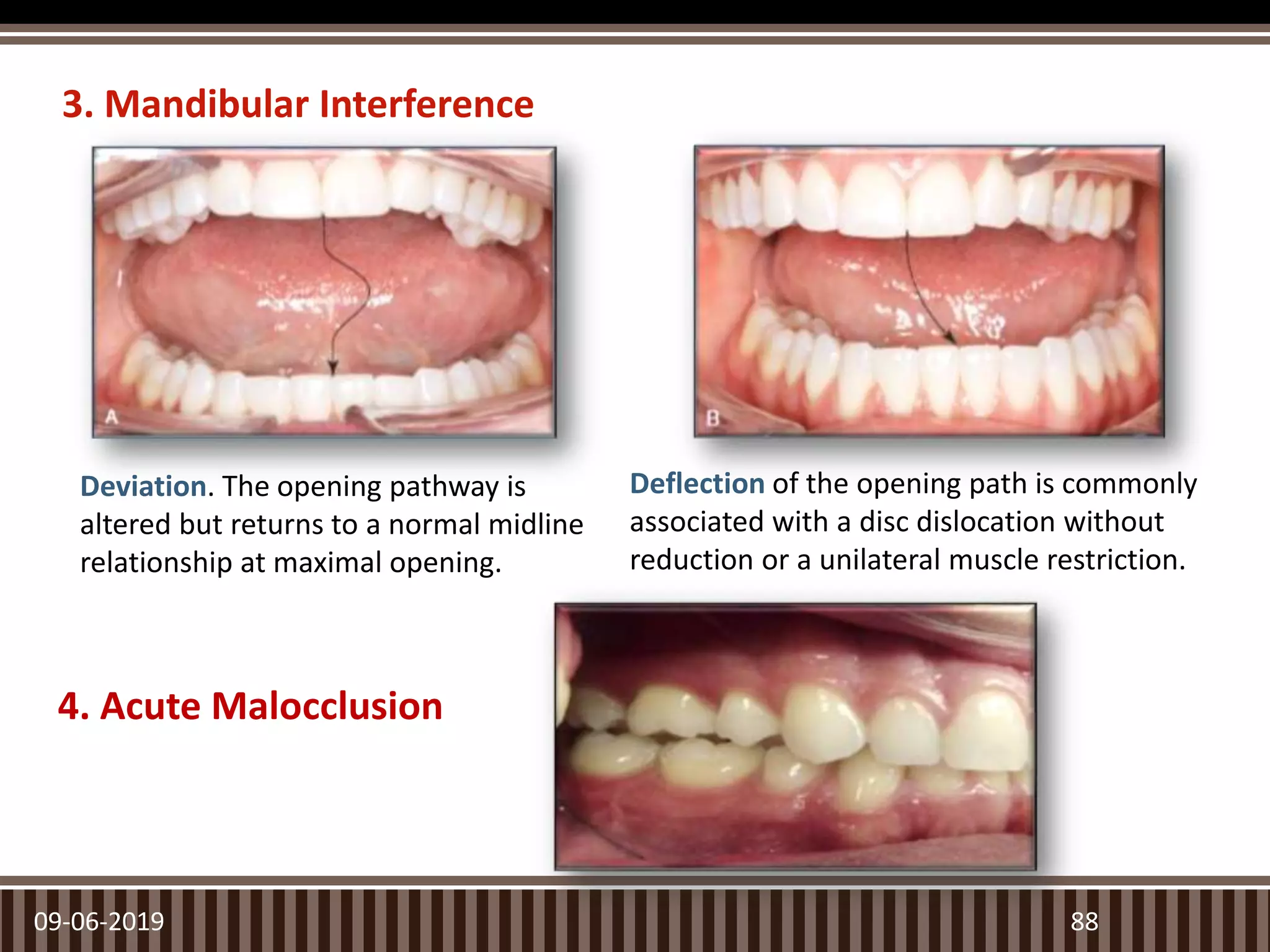
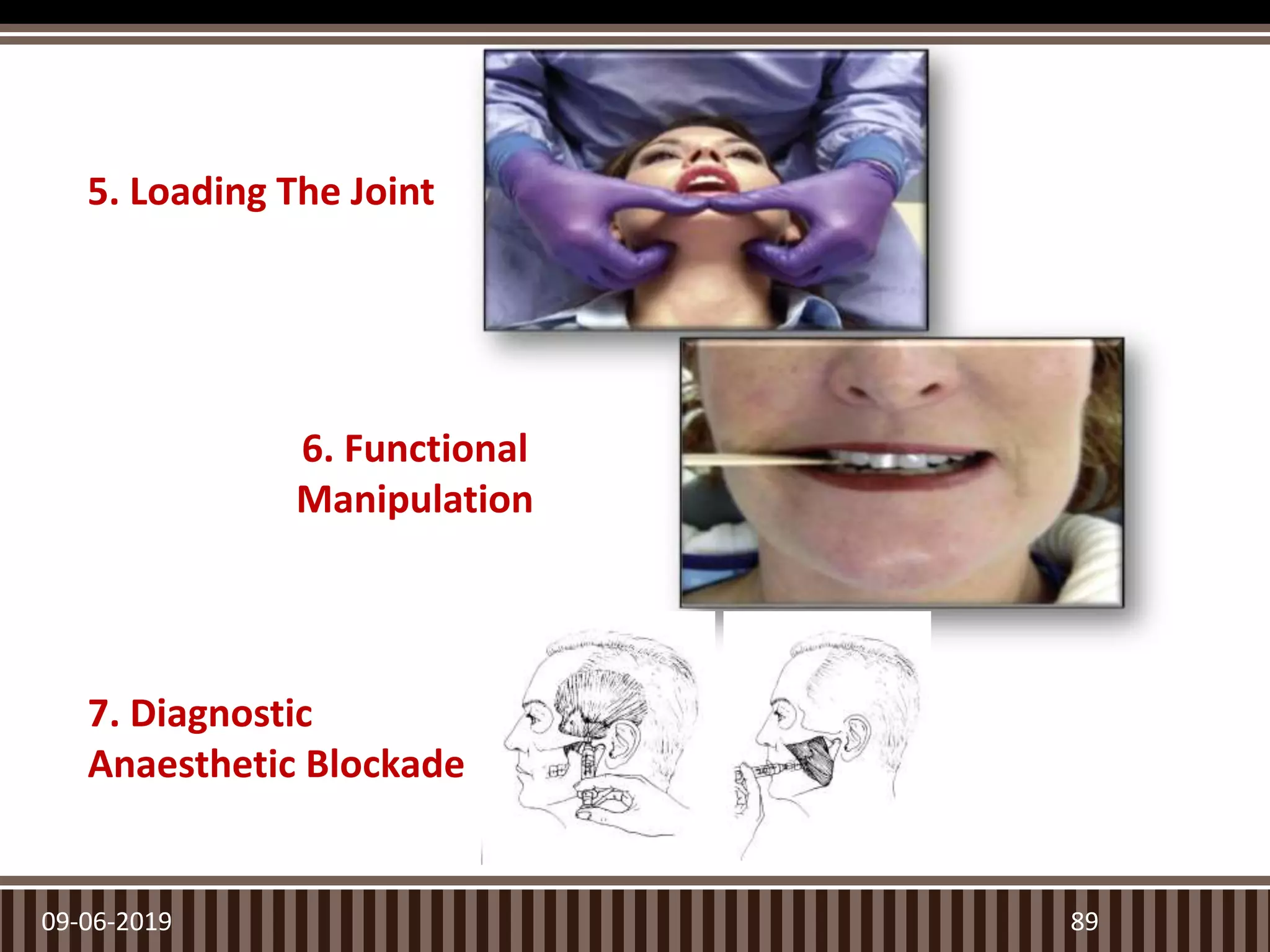
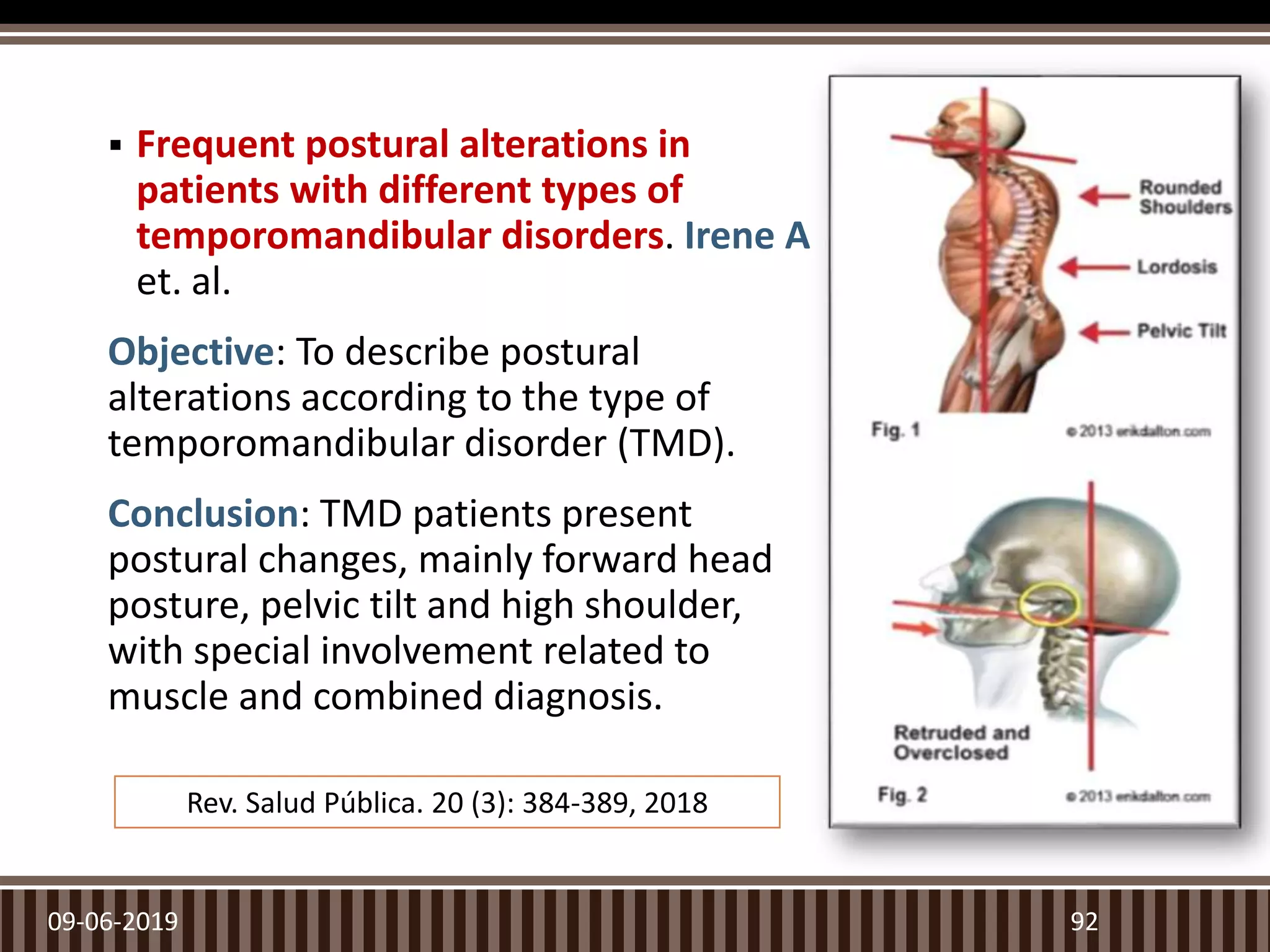
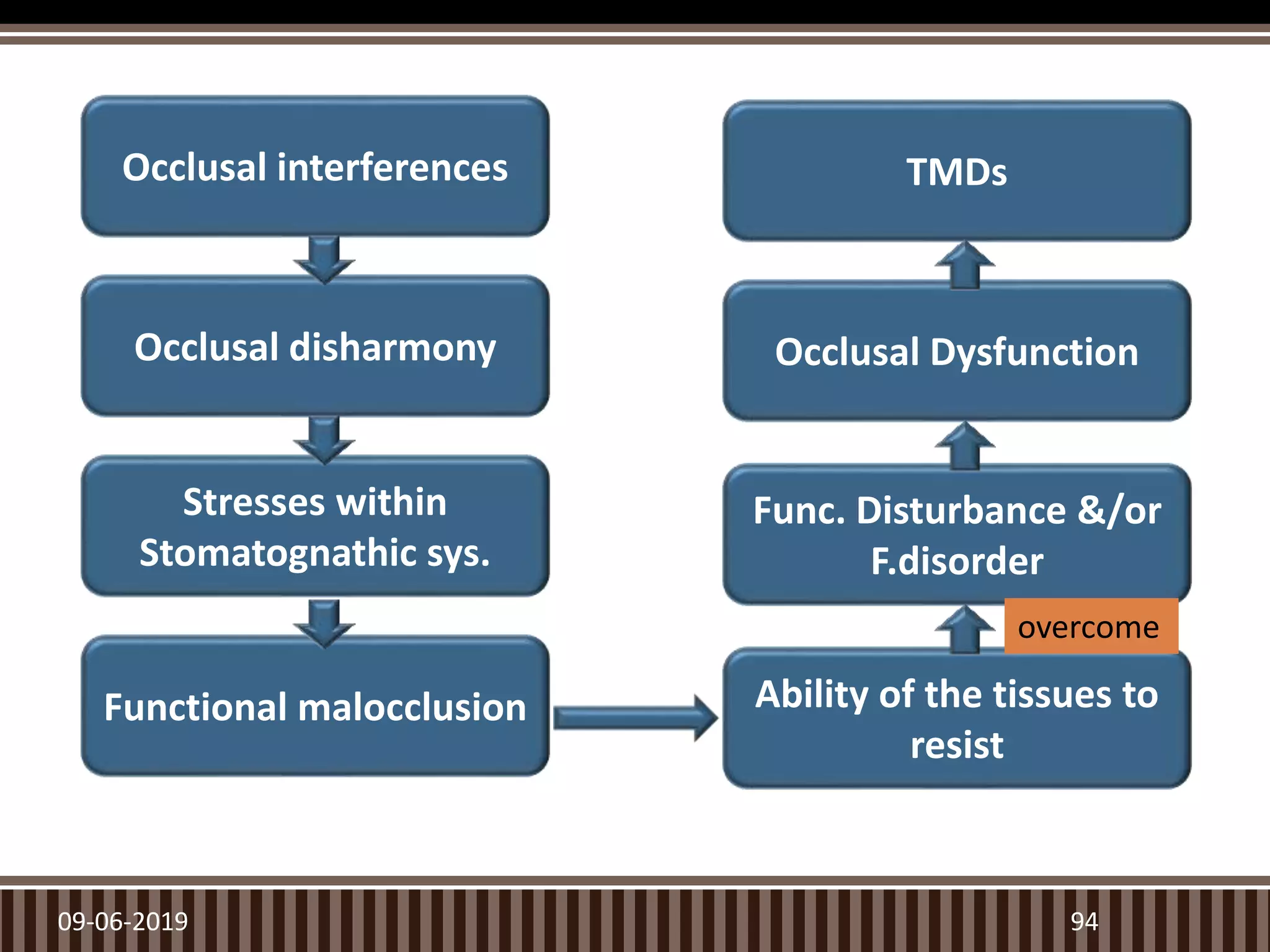
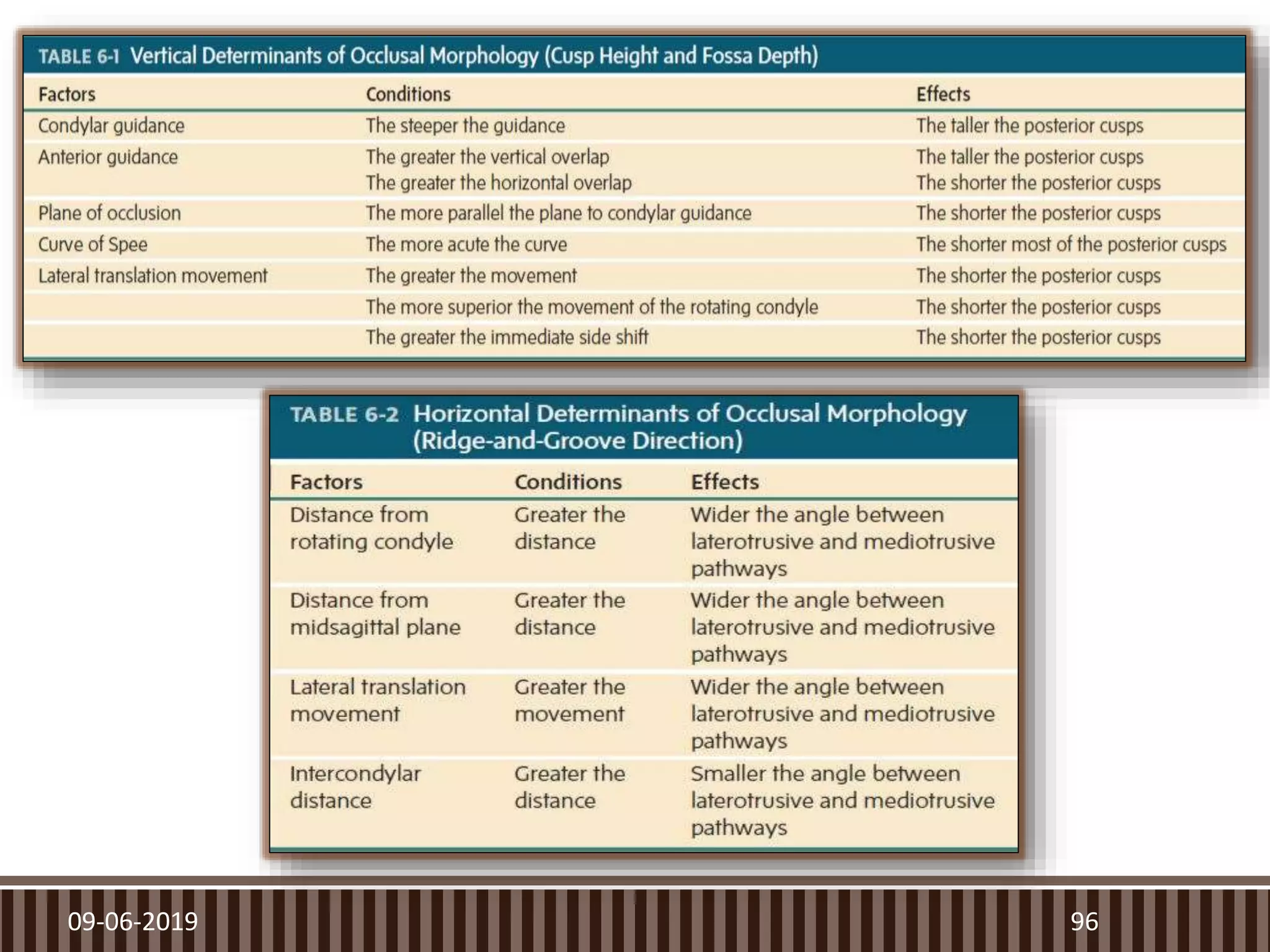
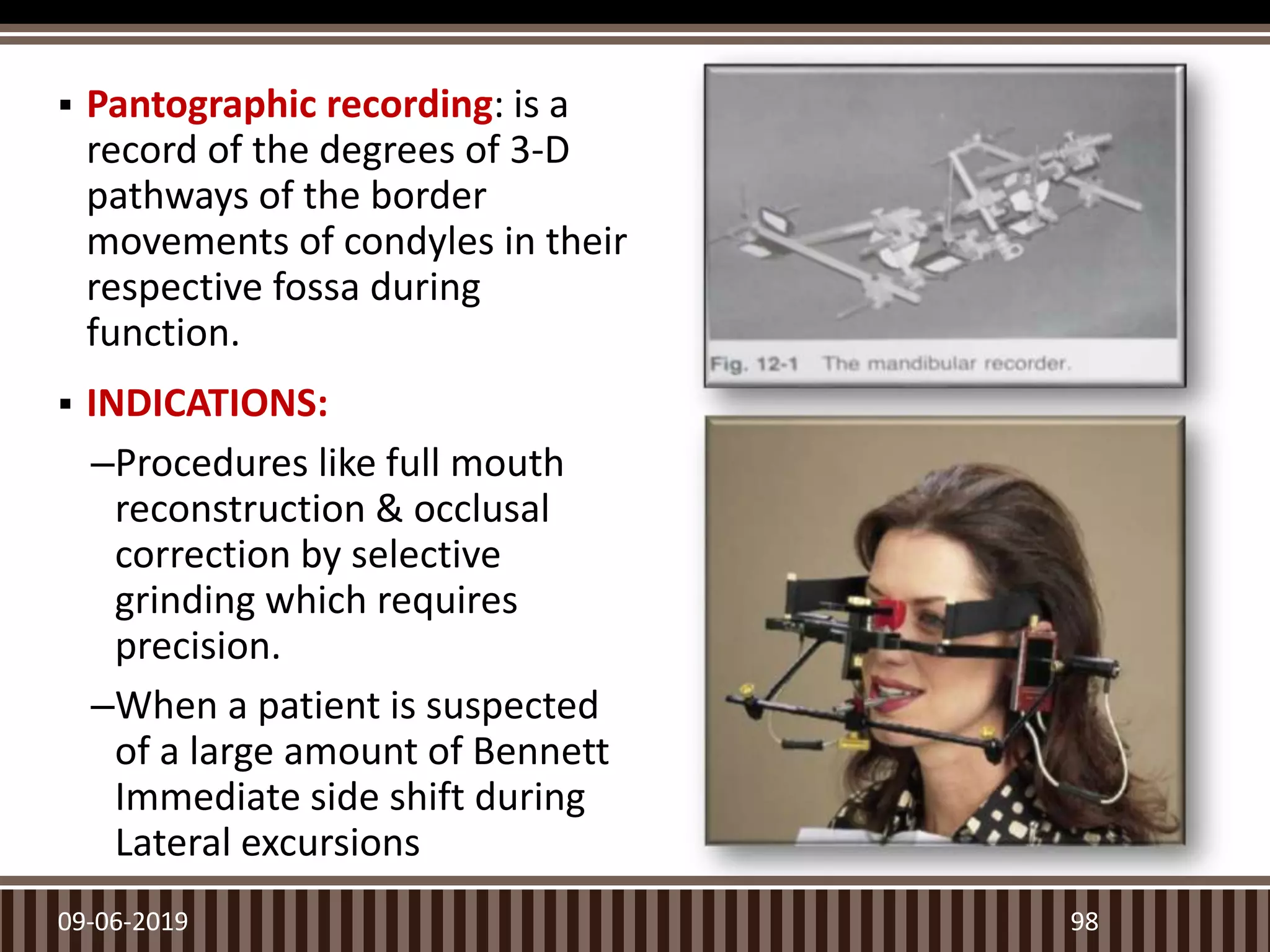
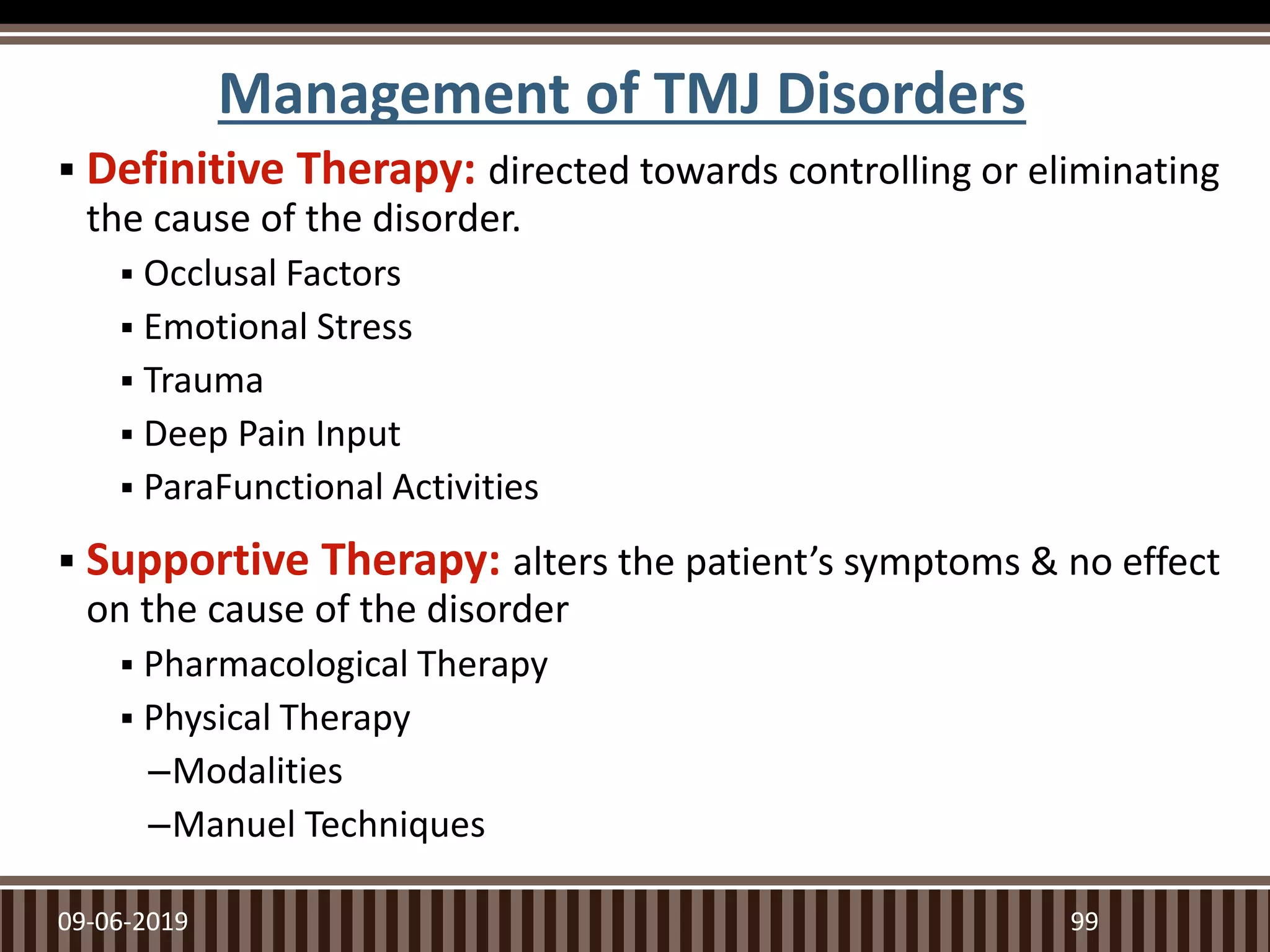
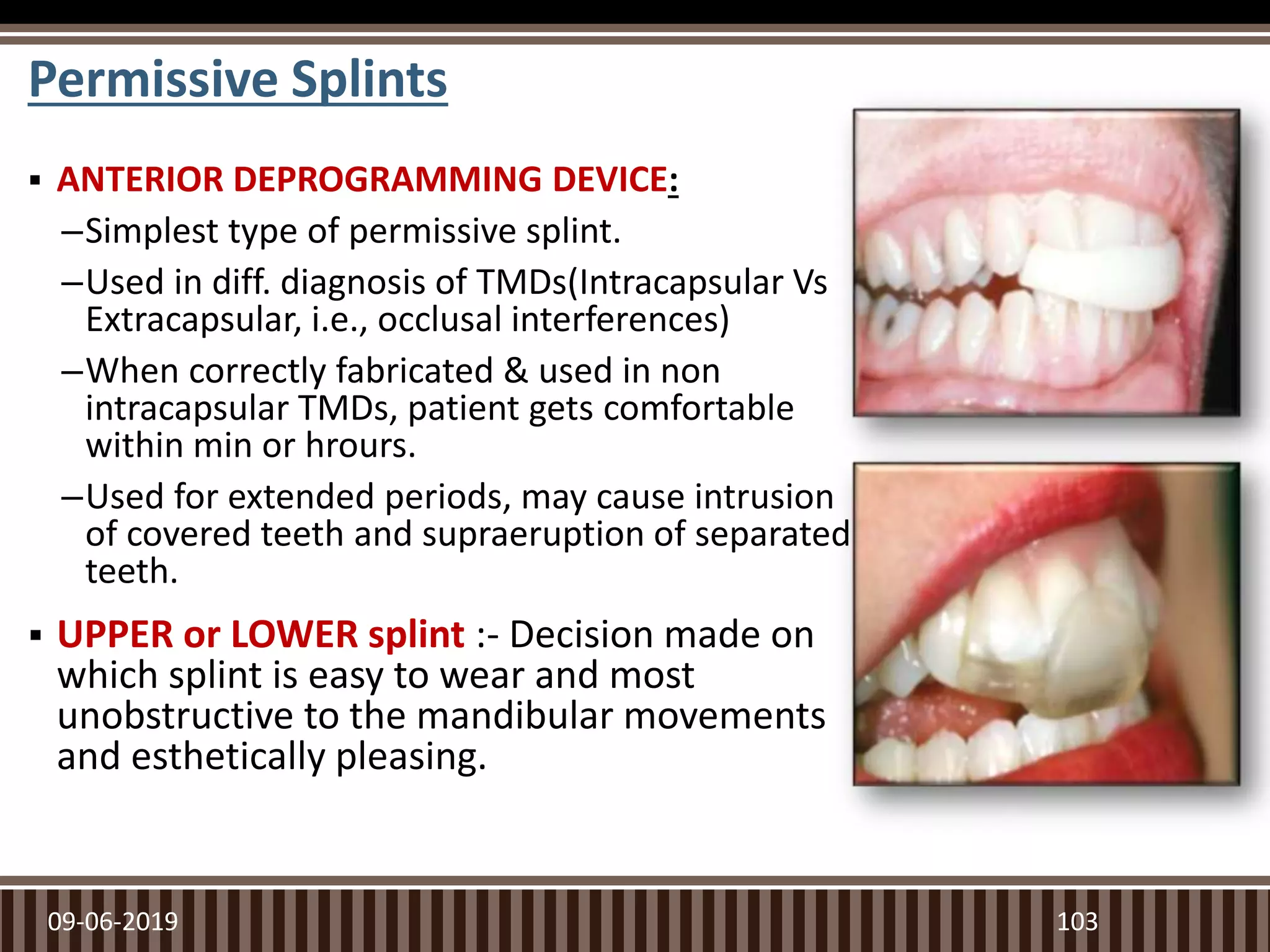
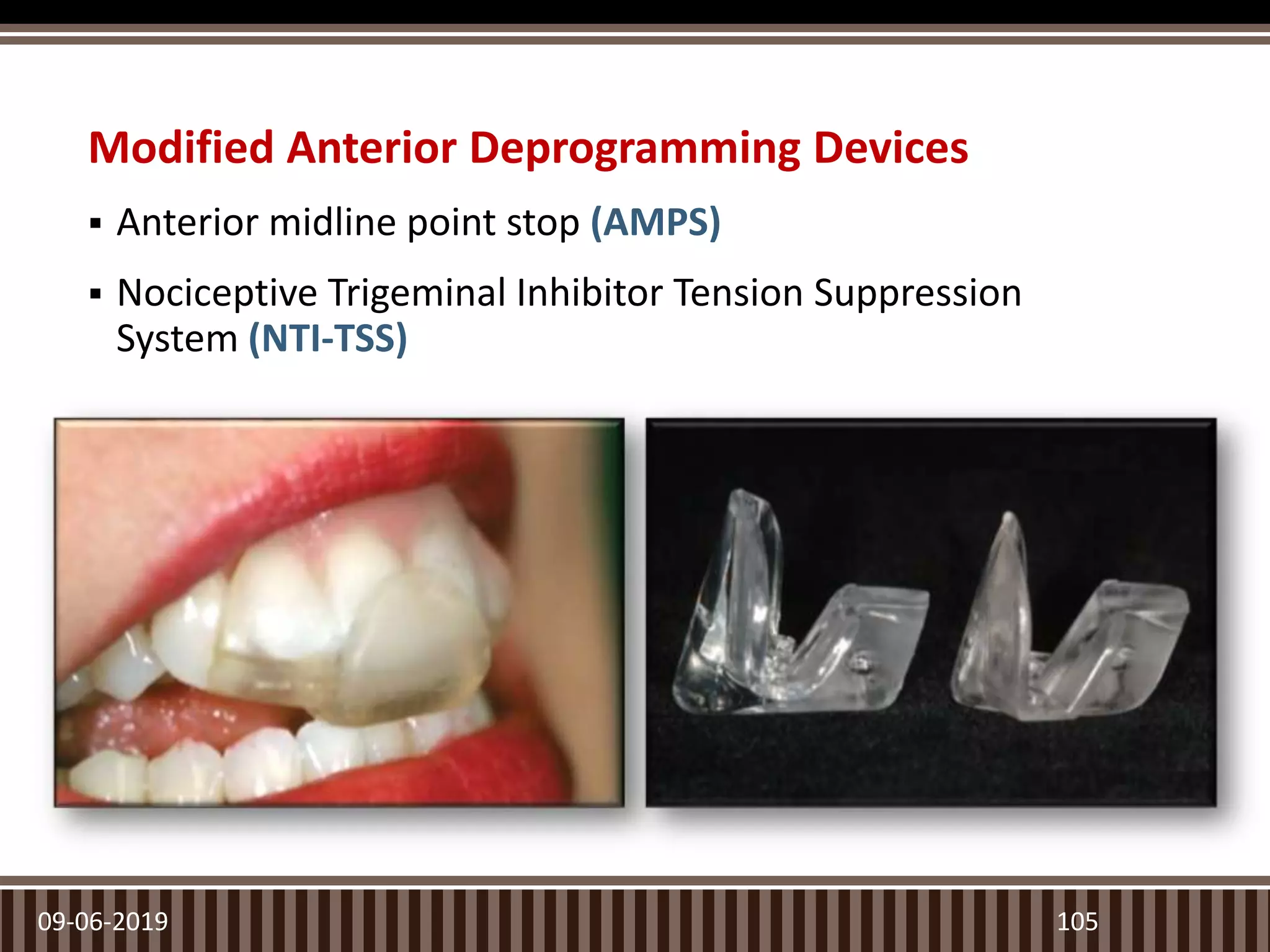
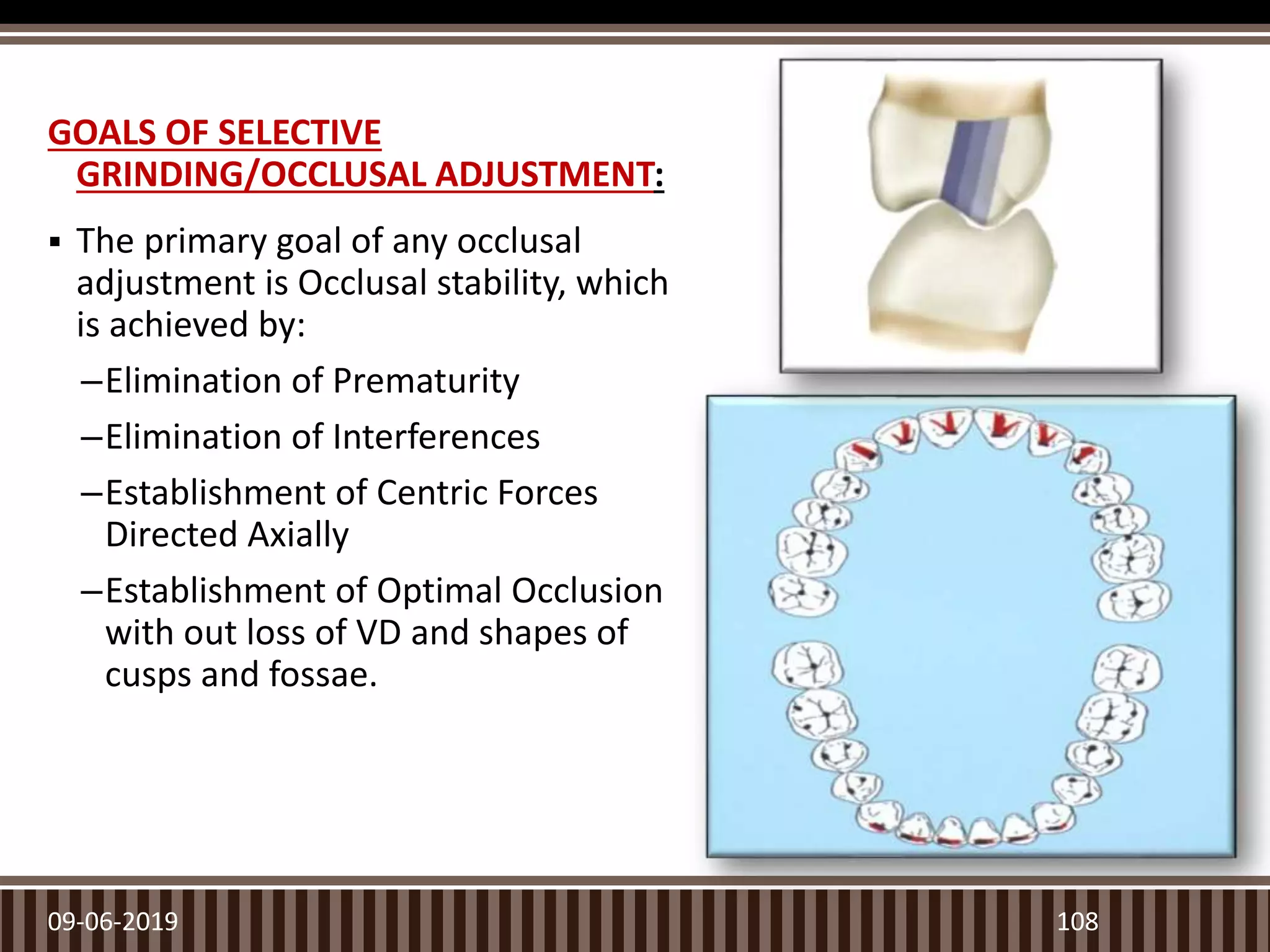
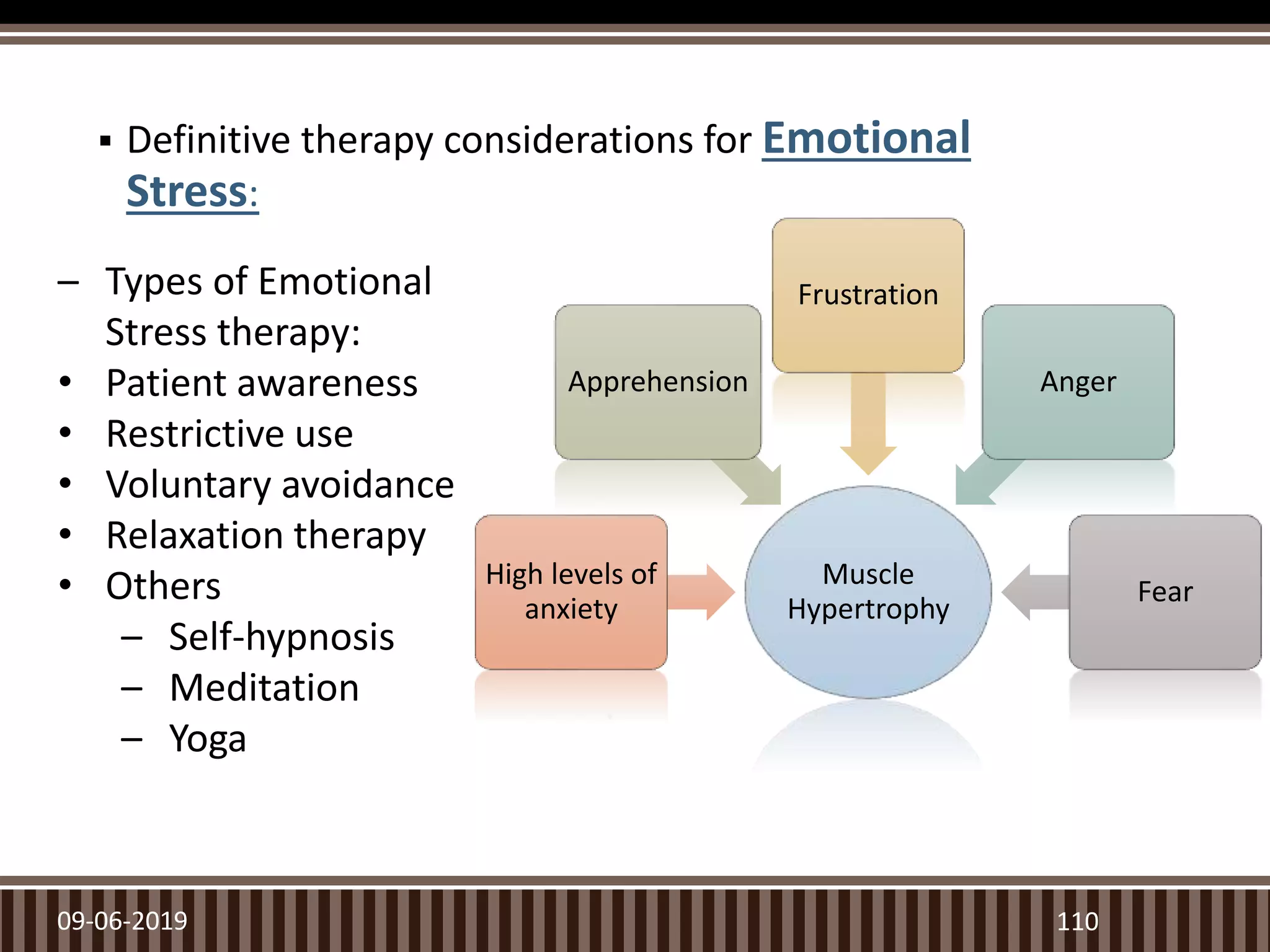
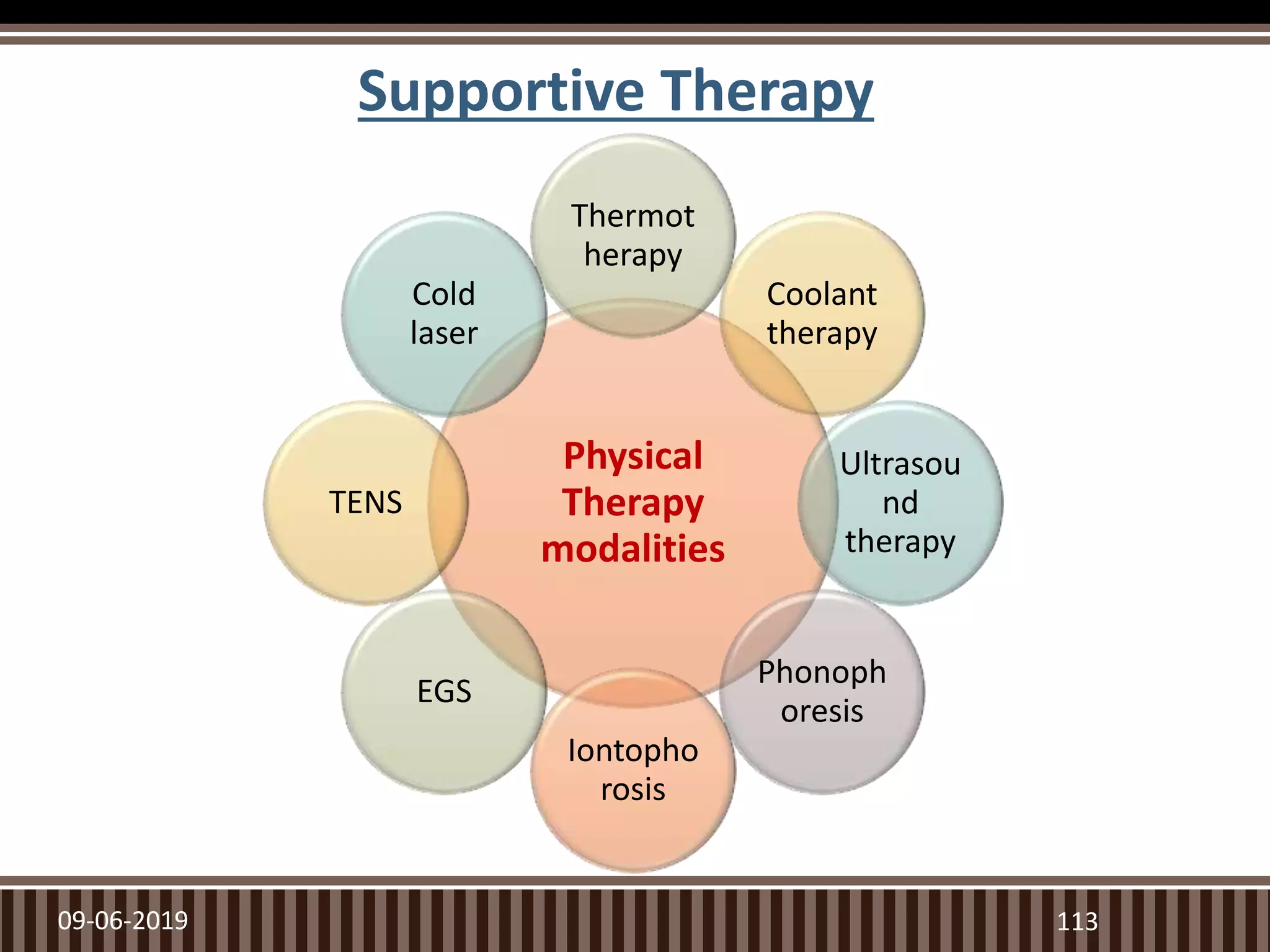
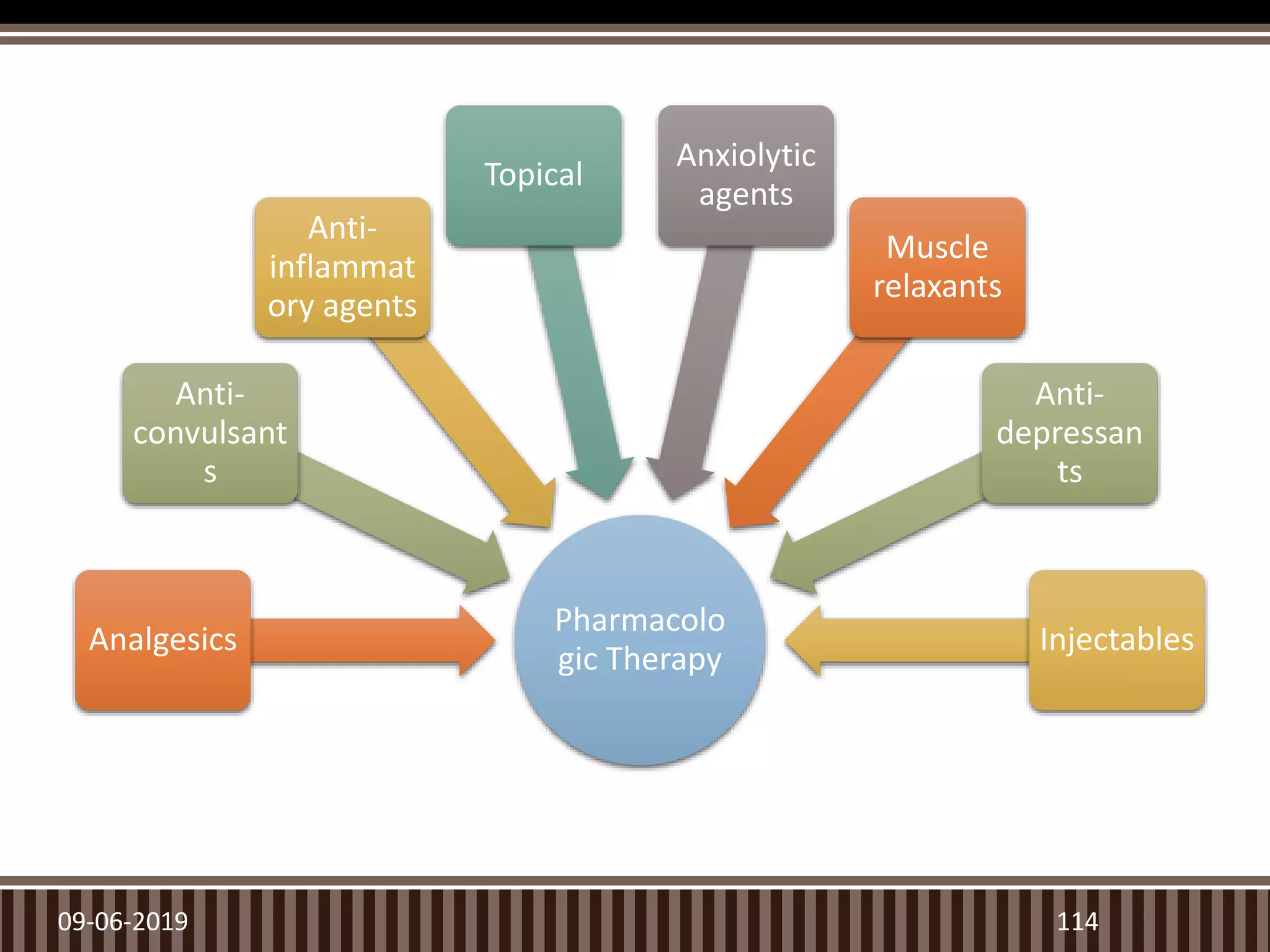
The document presents a seminar on the temporomandibular joint (TMJ) and its significance in prosthodontics, covering aspects such as anatomy, growth, development, and disorders. It details the functional mechanics of the TMJ, including the classification of disorders and the role of occlusion in these conditions, as well as treatment options. The seminar also delves into the joint's biomechanics, innervation, blood supply, and the muscles involved in mandibular movement.