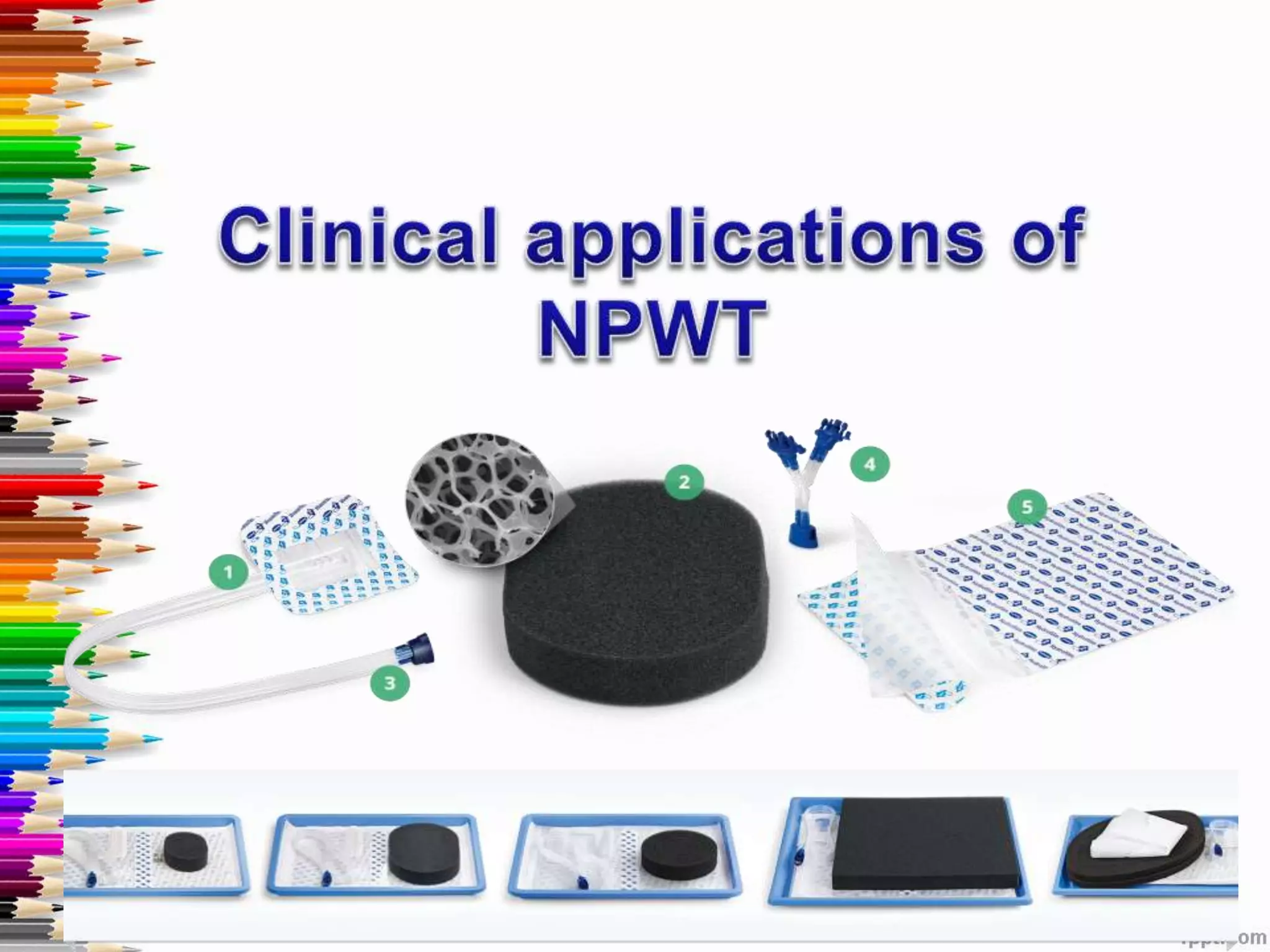
1. The document discusses negative pressure wound therapy (NPWT), including its history, mechanisms of action, clinical applications, and future perspectives.
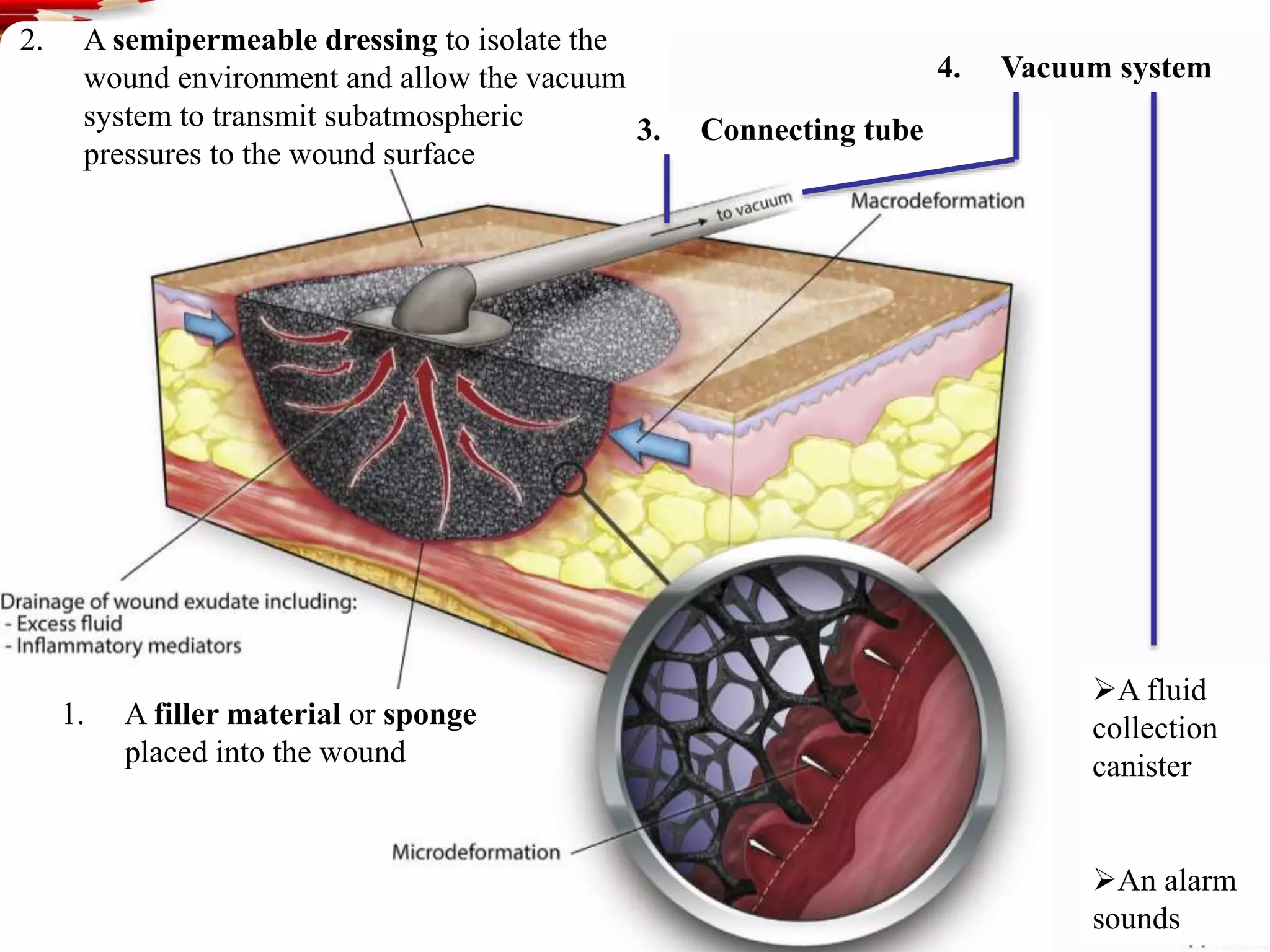
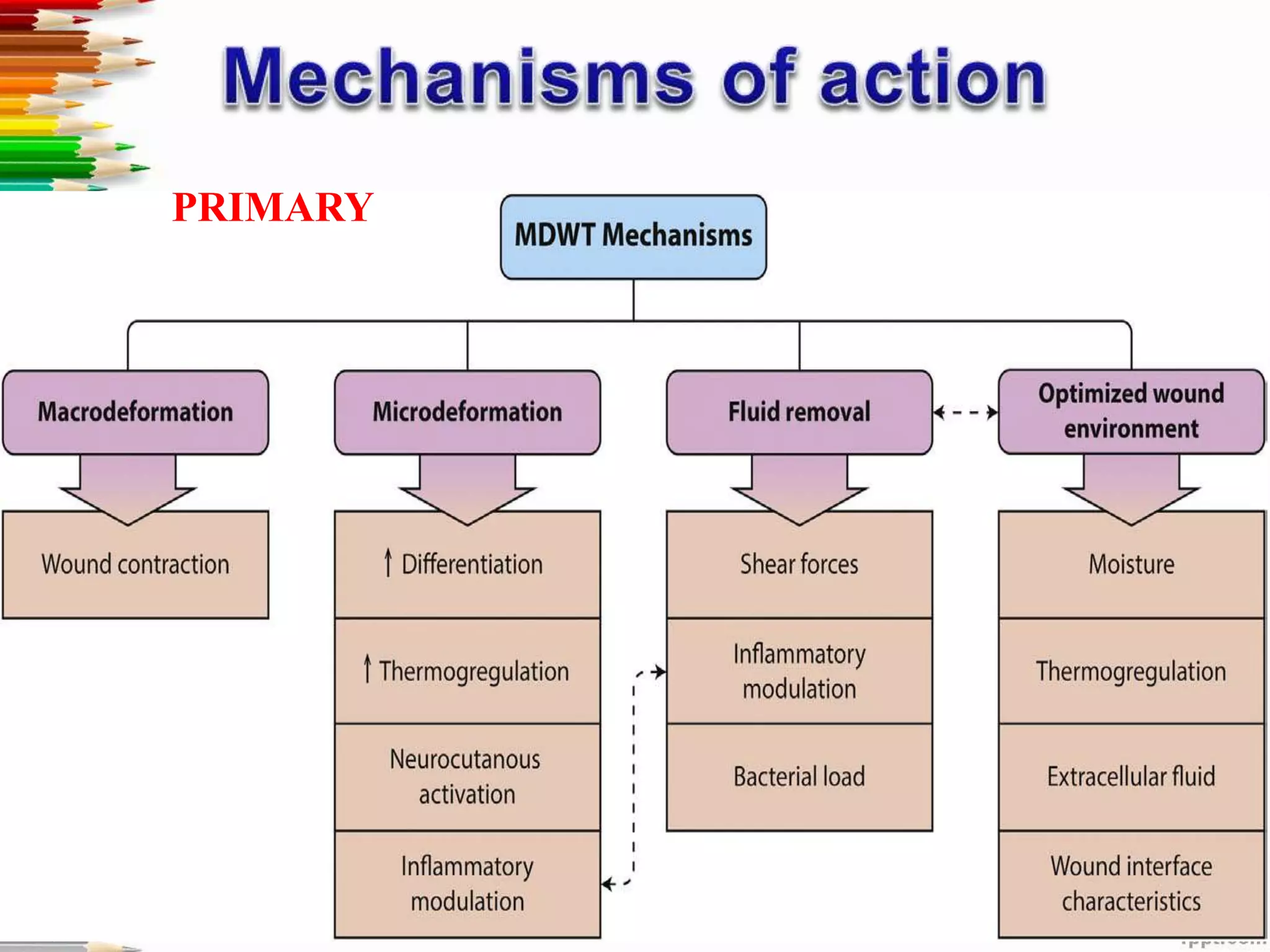
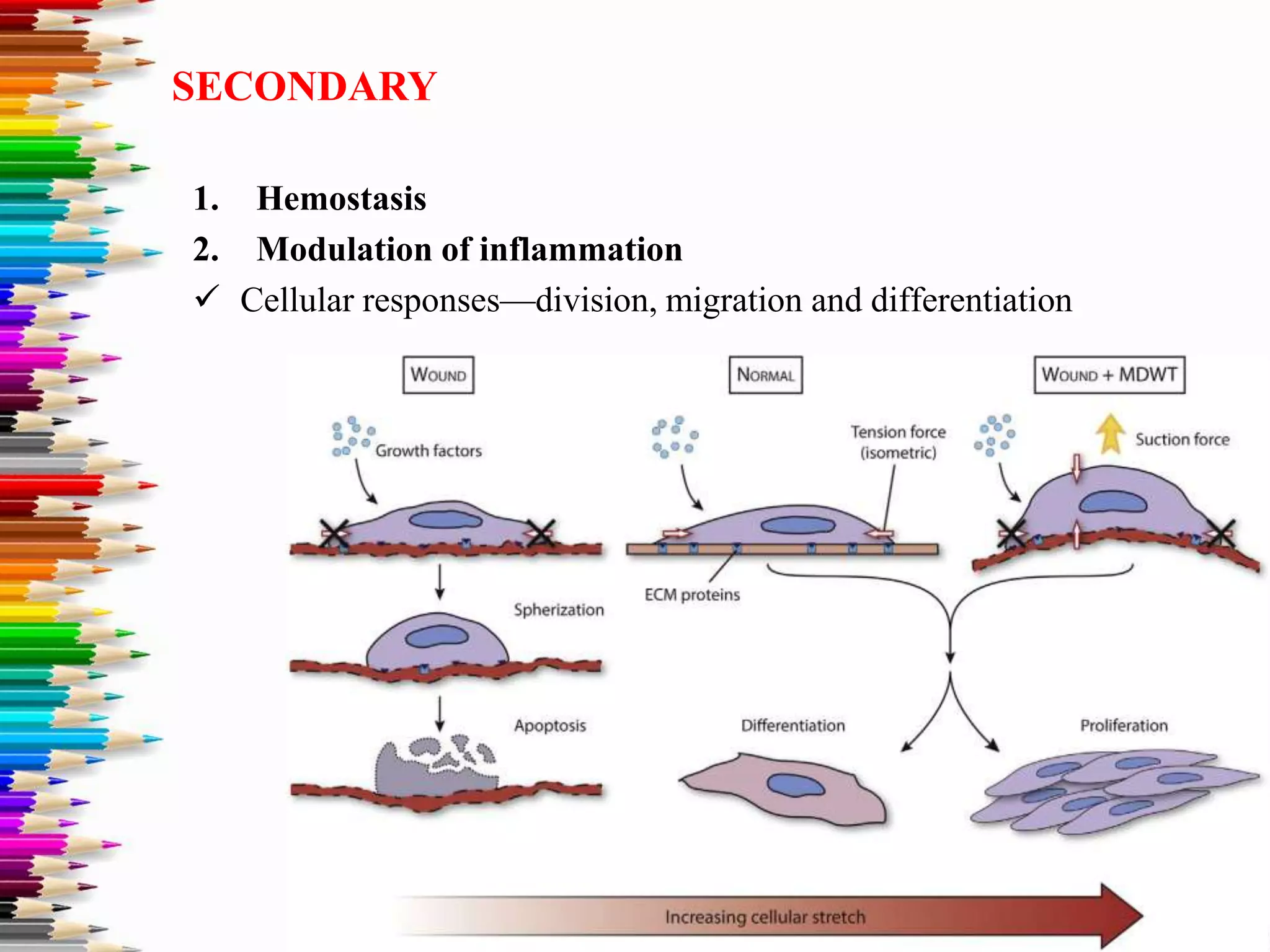
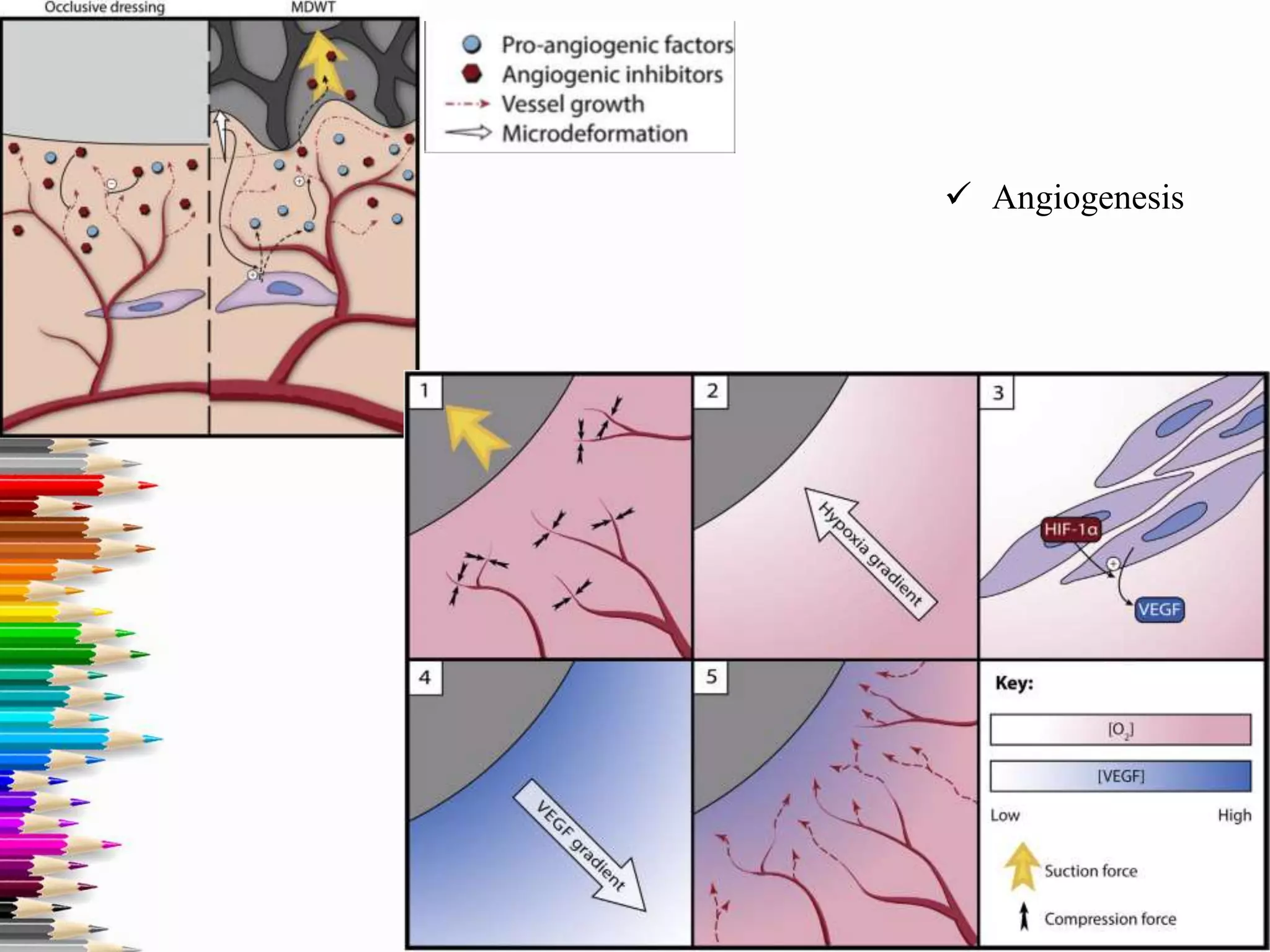
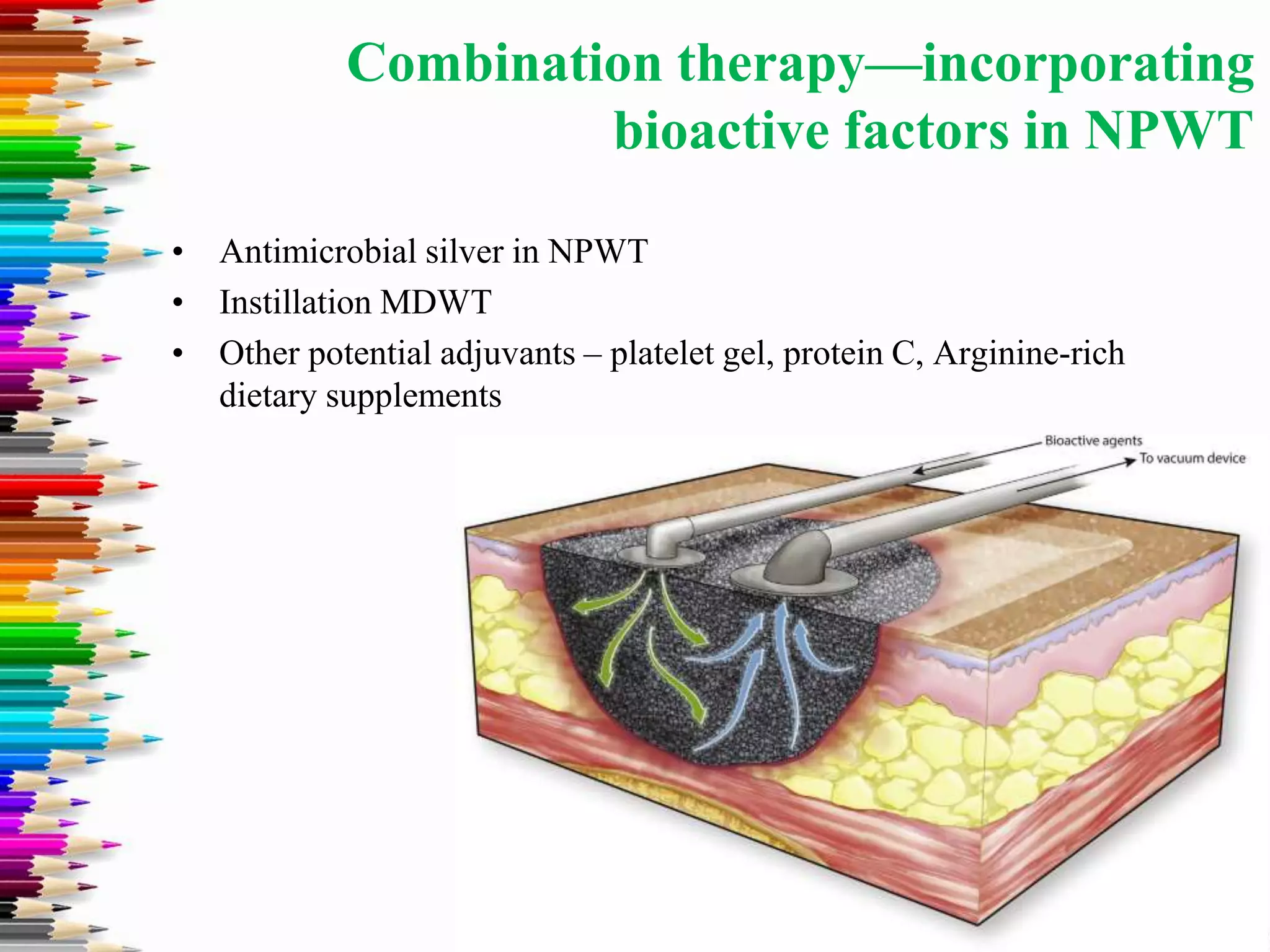
2. NPWT uses subatmospheric pressure to promote wound healing through mechanisms like hemostasis, modulation of inflammation, angiogenesis, and granulation tissue formation.
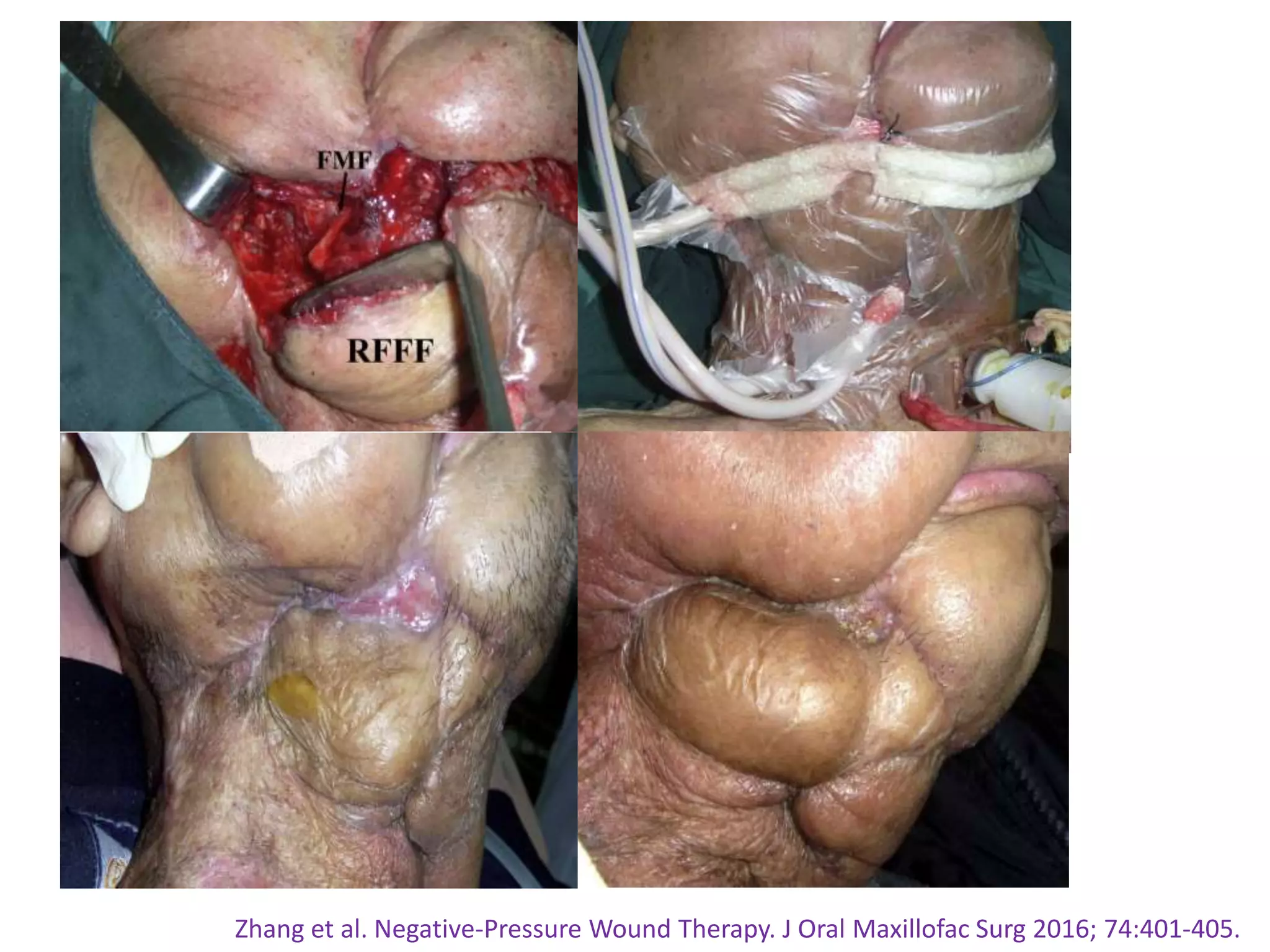
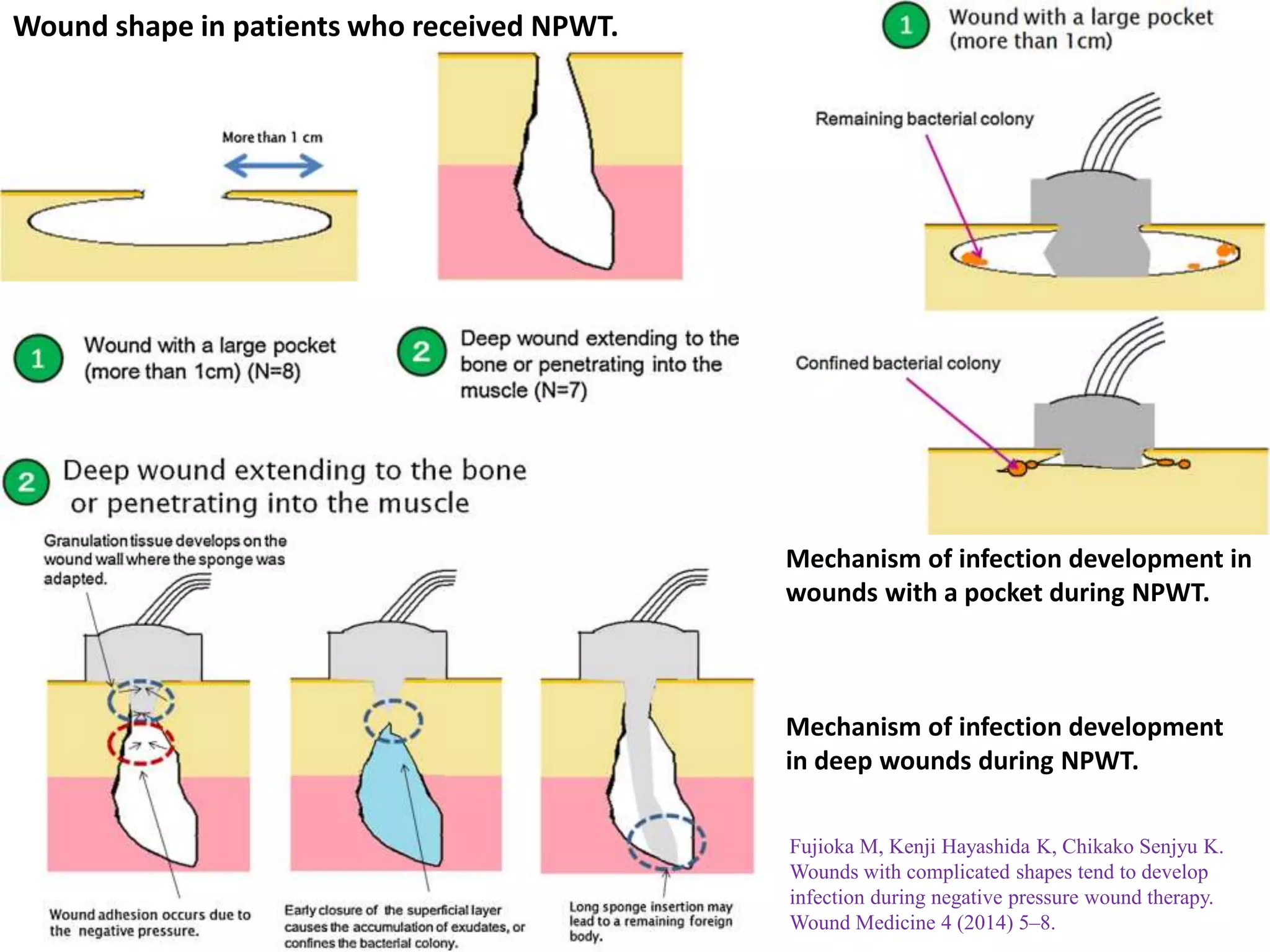
3. Studies show NPWT can effectively treat wounds in complex areas like the head and neck region, and may help close submandibular fistulas. However, wounds with pockets or deep shapes are more prone to infection with NPWT.