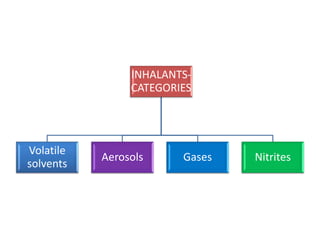
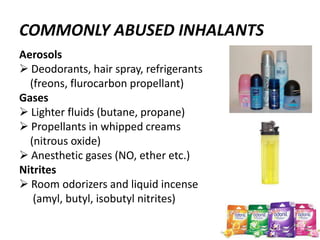
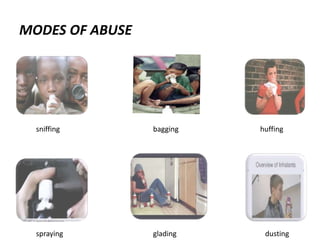
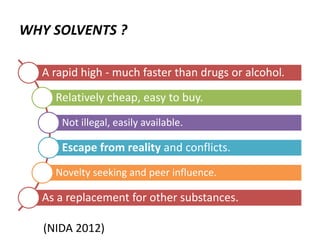
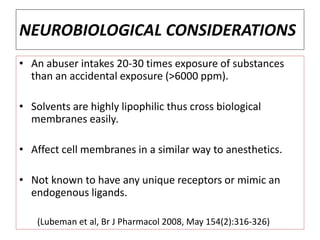
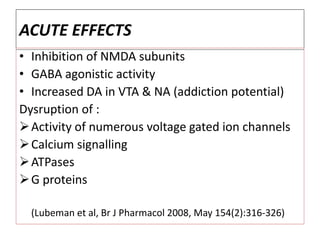
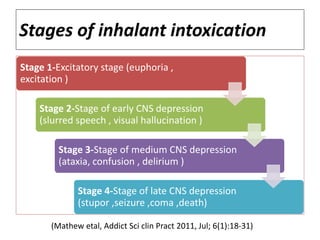
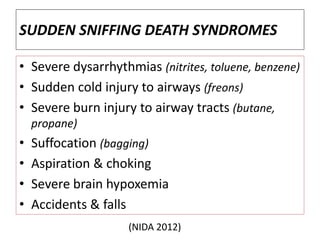
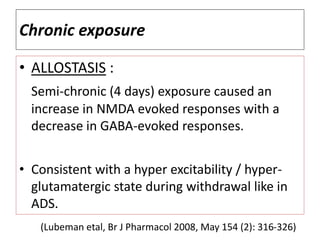
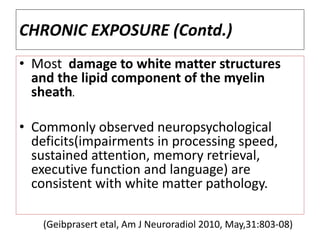
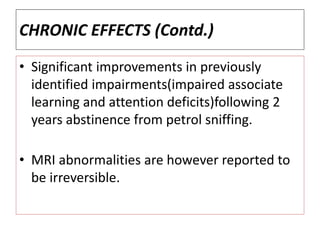
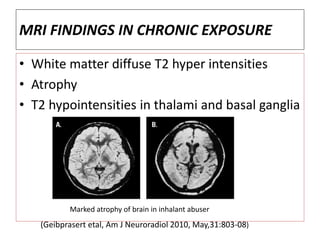
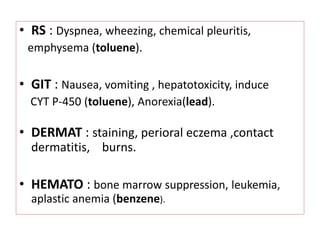
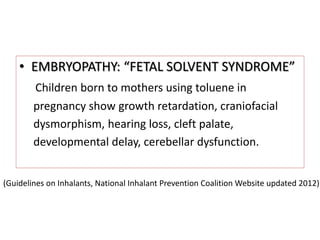
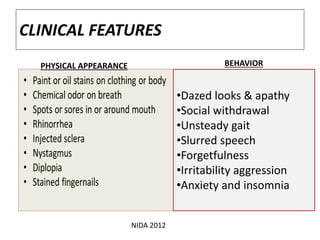
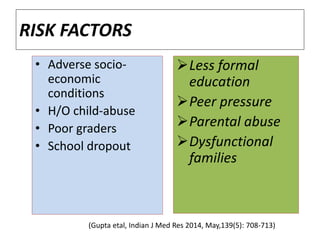
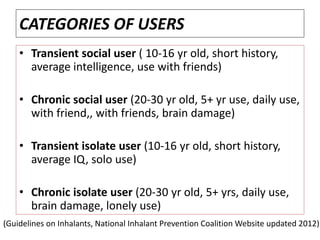
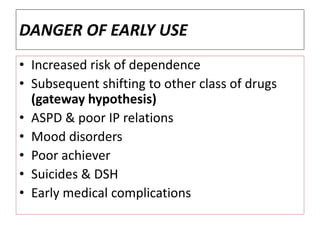
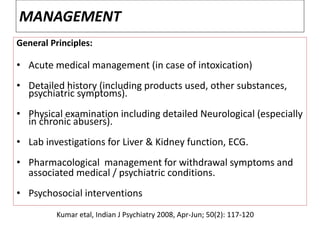
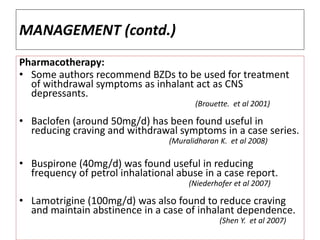
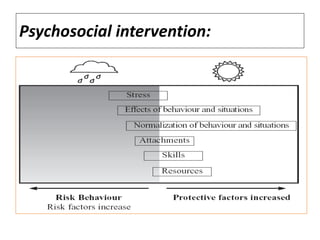
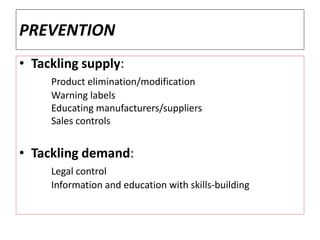
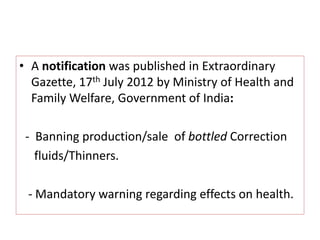
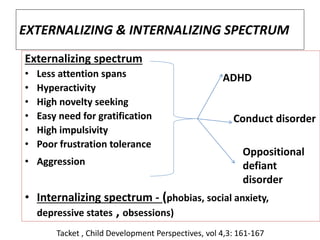
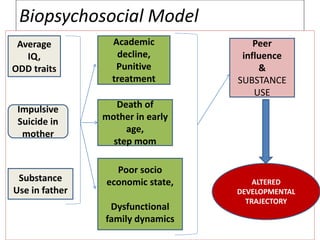
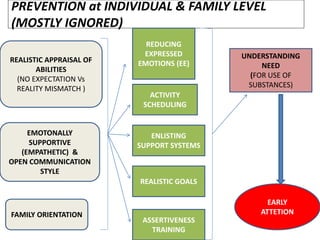
Inhalant abuse involves inhaling chemical vapors from household products like glues and solvents to get high. Common inhalants include volatile solvents, aerosols, gases, and nitrites. Acute effects include euphoria and CNS depression, while chronic use can lead to neurological and cognitive issues like memory problems. Risk factors include peer pressure and socioeconomic adversity. Prevention focuses on limiting access, education, and addressing underlying issues like mental health problems. Management involves treatment of withdrawal, medical complications, and psychosocial support.