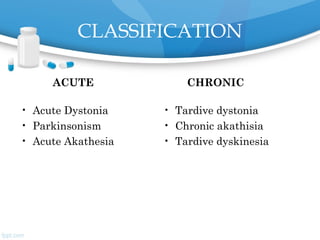
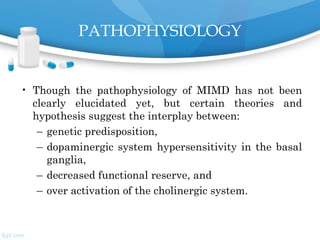
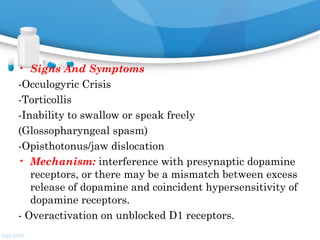
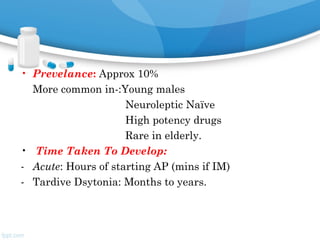
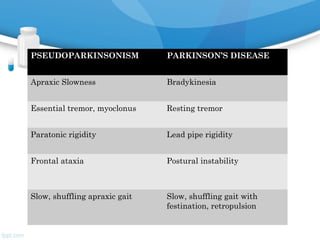
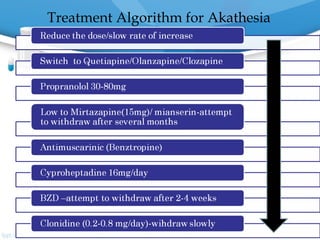
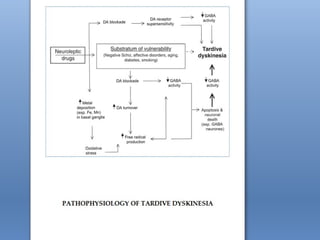
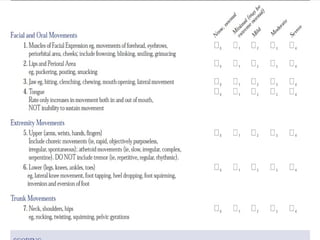
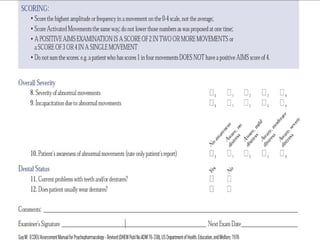
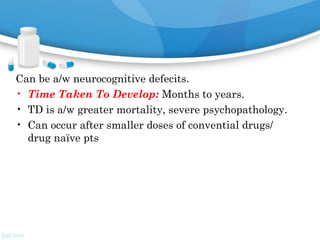
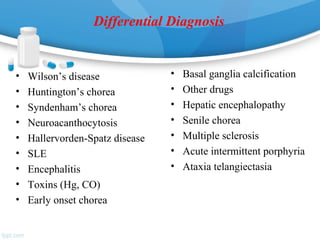
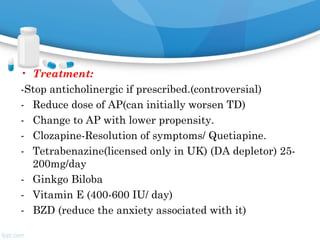
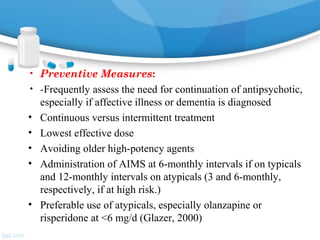
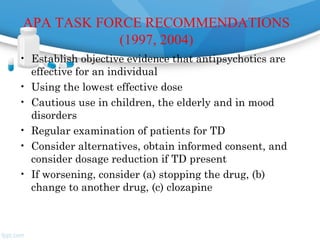
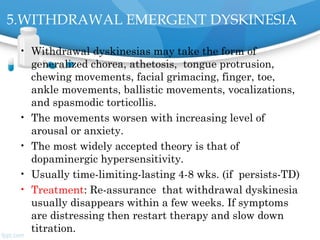
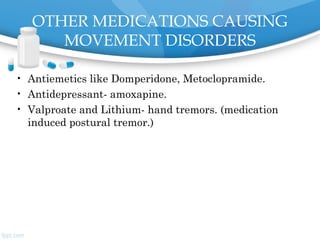
This document discusses drug-induced movement disorders caused by antipsychotic medications. It covers the classification of both acute and chronic movement disorders including dystonia, parkinsonism, akathisia, and tardive dyskinesia. It discusses the pathophysiology, risk factors, signs and symptoms, time of onset, scales used for assessment, management, and prevention of these medication-induced movement disorders. It also lists other medications that can cause movement disorders and the DSM-5 diagnostic categories for medication-induced movement disorders.