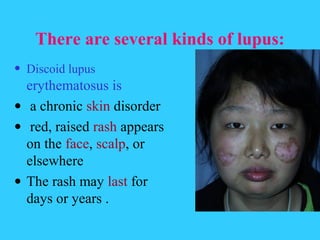
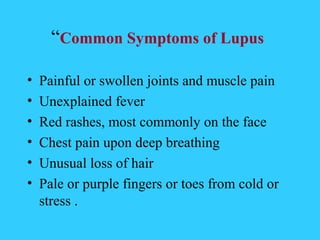
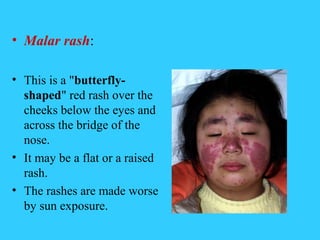
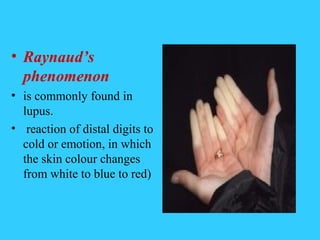
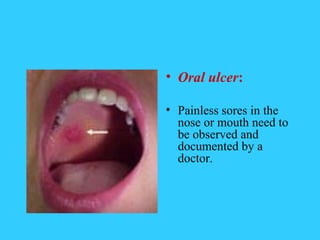
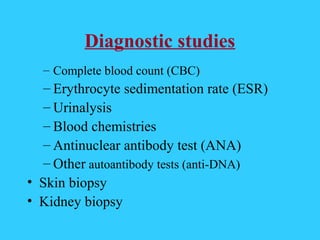
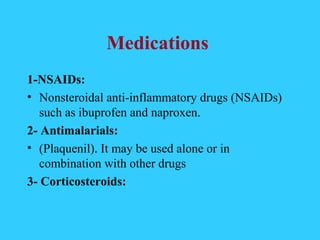
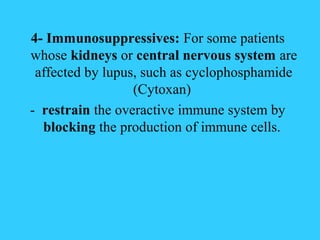
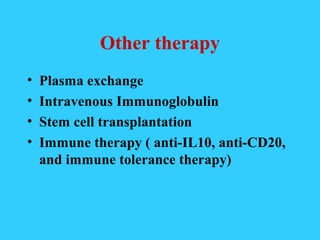
Systemic Lupus Erythematosus (SLE) is an autoimmune disease where the immune system attacks its own tissues. It most commonly affects women aged 15-40. The exact causes are unknown but genetics, viruses, sunlight, and some drugs may play a role. Symptoms vary but can include rashes, joint pain, fatigue, and organ inflammation. Diagnosis involves blood tests and potentially biopsies. Treatment focuses on rest, sun protection, medications like NSAIDs, antimalarials, corticosteroids, and immunosuppressants to control disease activity and prevent organ damage. Nursing care aims to manage symptoms, prevent infections, and educate patients.