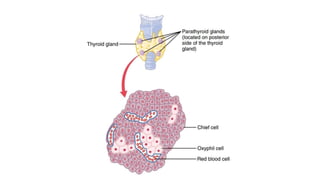
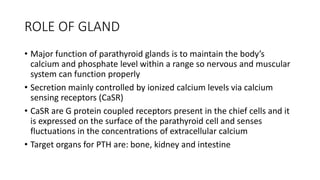
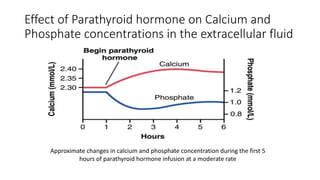
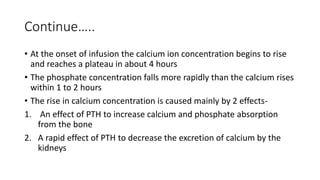
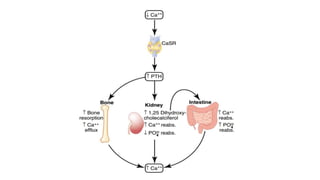
The document discusses the parathyroid gland's anatomy, function, and related pathophysiology. It explains that the major role of the parathyroid gland is to regulate calcium and phosphate levels, with its hormone, parathyroid hormone (PTH), affecting bone, kidney, and intestinal absorption. Conditions such as hypoparathyroidism and hyperparathyroidism are described, along with their impact on calcium levels and bone health.