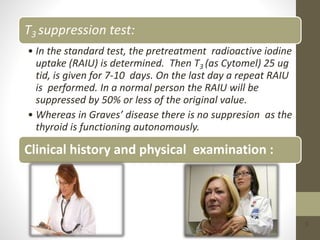
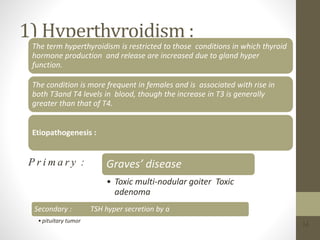
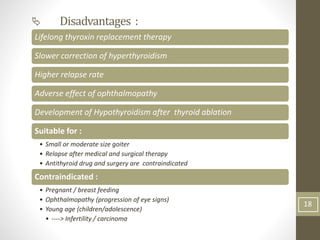
This document provides information about the thyroid gland and parathyroid glands, including their anatomy, functions, and diseases. Regarding the thyroid gland, it discusses how it produces thyroid hormones T4 and T3, which are essential for growth and metabolism. It also describes the evaluation and treatment of thyroid diseases like hyperthyroidism and hypothyroidism. Concerning the parathyroid glands, it notes their role in calcium homeostasis through PTH secretion and outlines hypoparathyroidism and hyperparathyroidism as disorders of the parathyroid glands.