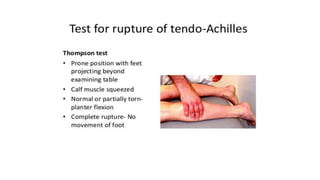
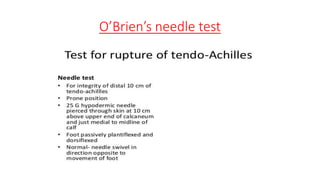
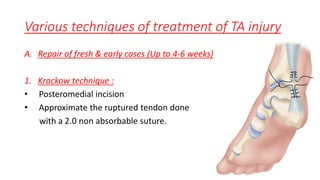
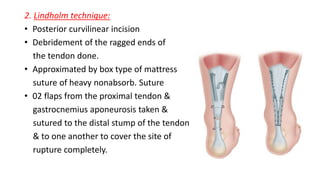
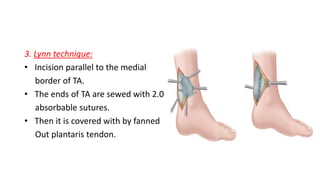
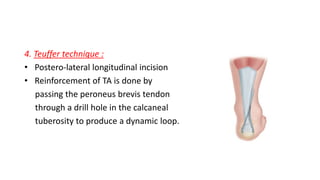
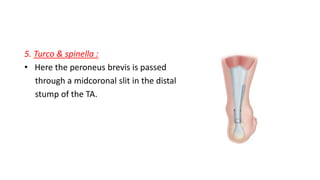
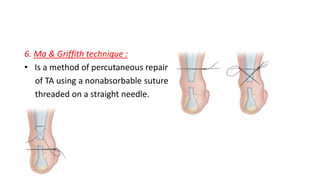
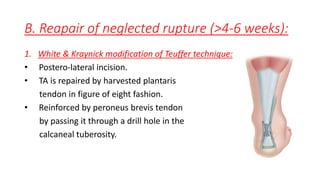
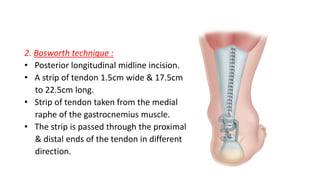
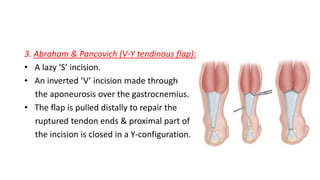
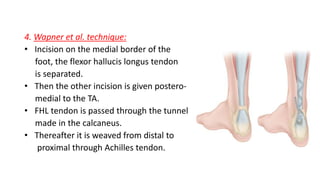
The document provides an overview of tendoachilles injuries, including classification into ruptures and tears, their mechanisms, clinical features, diagnosis, and treatment methods. It outlines examination techniques, surgical repair procedures for both fresh and neglected ruptures, and post-operative management strategies. Key examinations and surgical techniques are detailed, along with indications for each method of treatment.