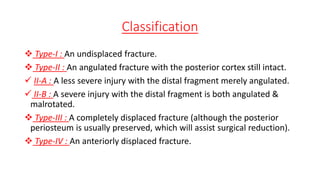
This document discusses supracondylar humeral fractures in children. It notes that these are the most common pediatric fractures, usually occurring from falls onto an outstretched hand in children ages 5-7. The fractures are classified into 4 types based on displacement and angulation. Type I are undisplaced while types II-IV are increasingly displaced, with type III being completely displaced. Treatment depends on type, with undisplaced or mildly angulated fractures treated with splinting while more severe fractures require closed or open reduction and percutaneous pinning under imaging guidance.