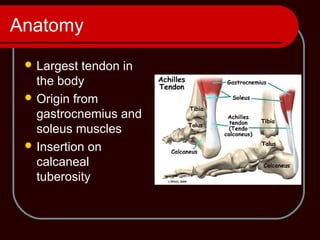
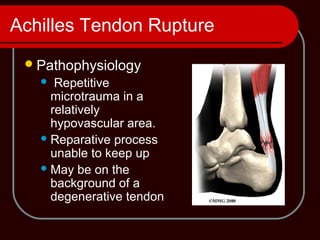
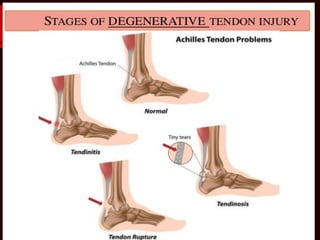
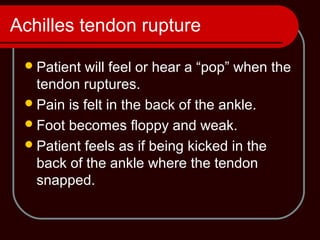
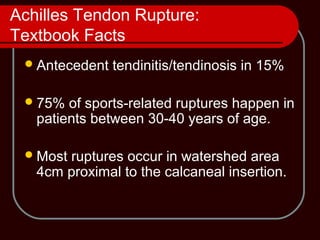
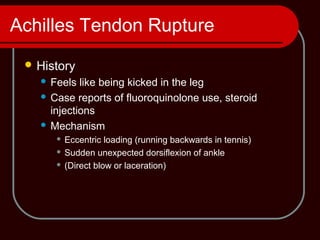
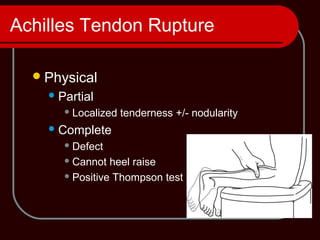
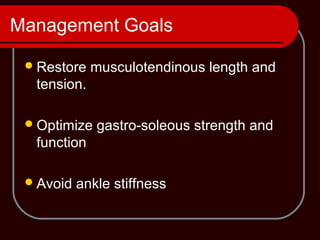
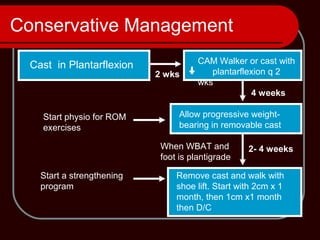
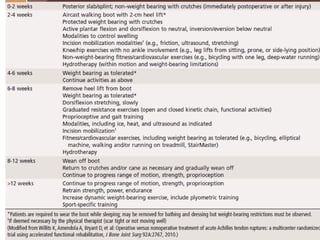
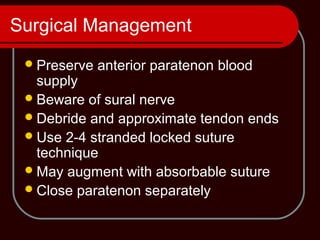
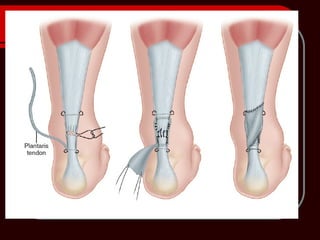
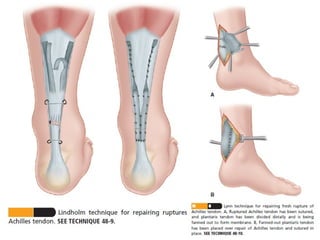
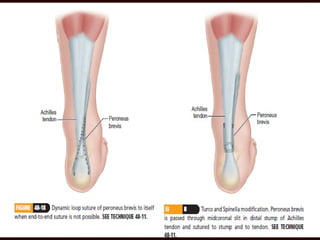
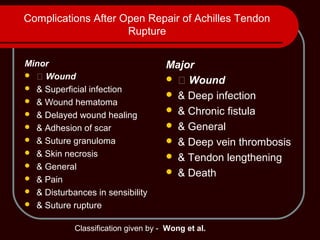
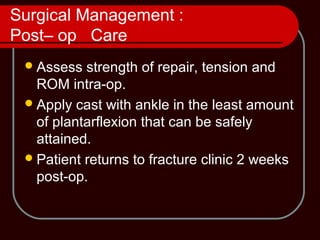
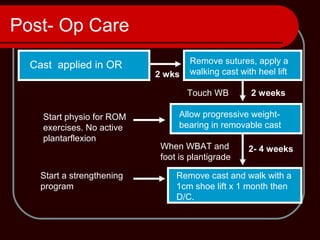
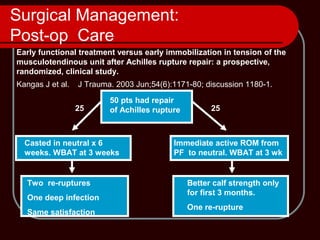
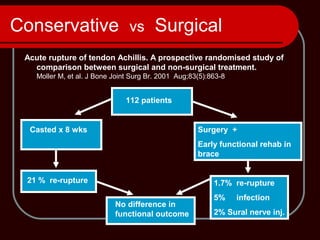
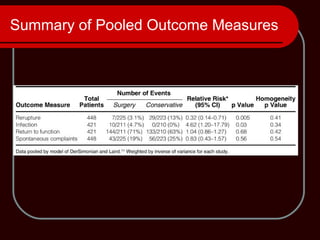
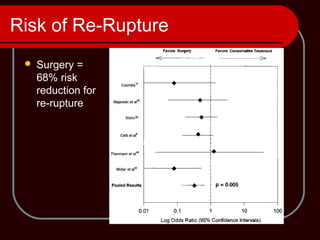
The Achilles tendon connects the calf muscles to the heel bone and is active during walking, running, and jumping. It is susceptible to injury from overuse or sudden strain. Common injuries include Achilles tendinitis, which is inflammation from overuse, and Achilles tendon rupture, which is a complete tear of the tendon. Ruptures are typically treated with surgery followed by immobilization in a cast or brace followed by physical therapy to regain strength and range of motion. While surgery lowers the risk of re-rupture compared to non-surgical treatment, both approaches can successfully treat ruptures if rehabilitation is done correctly.