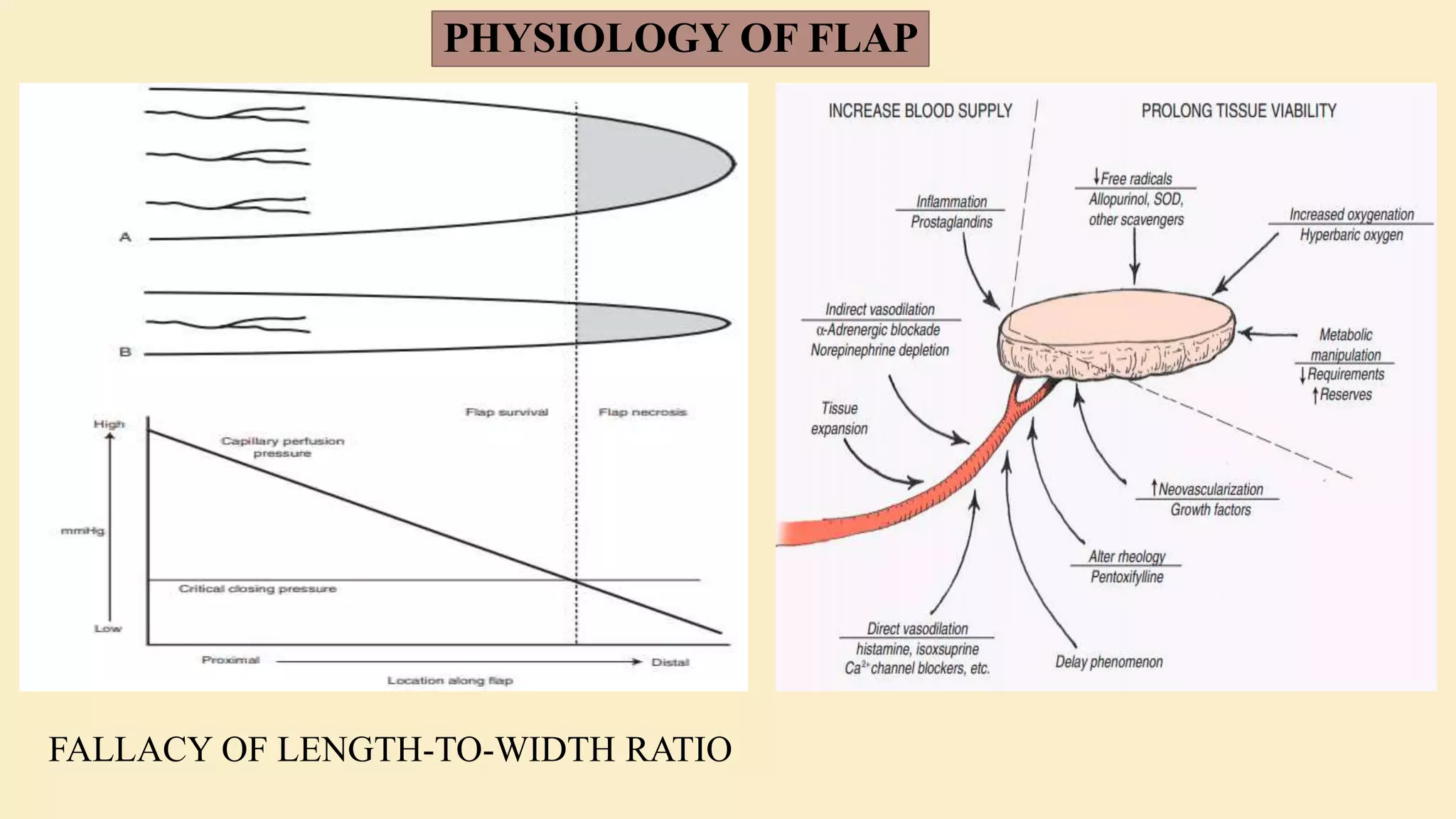
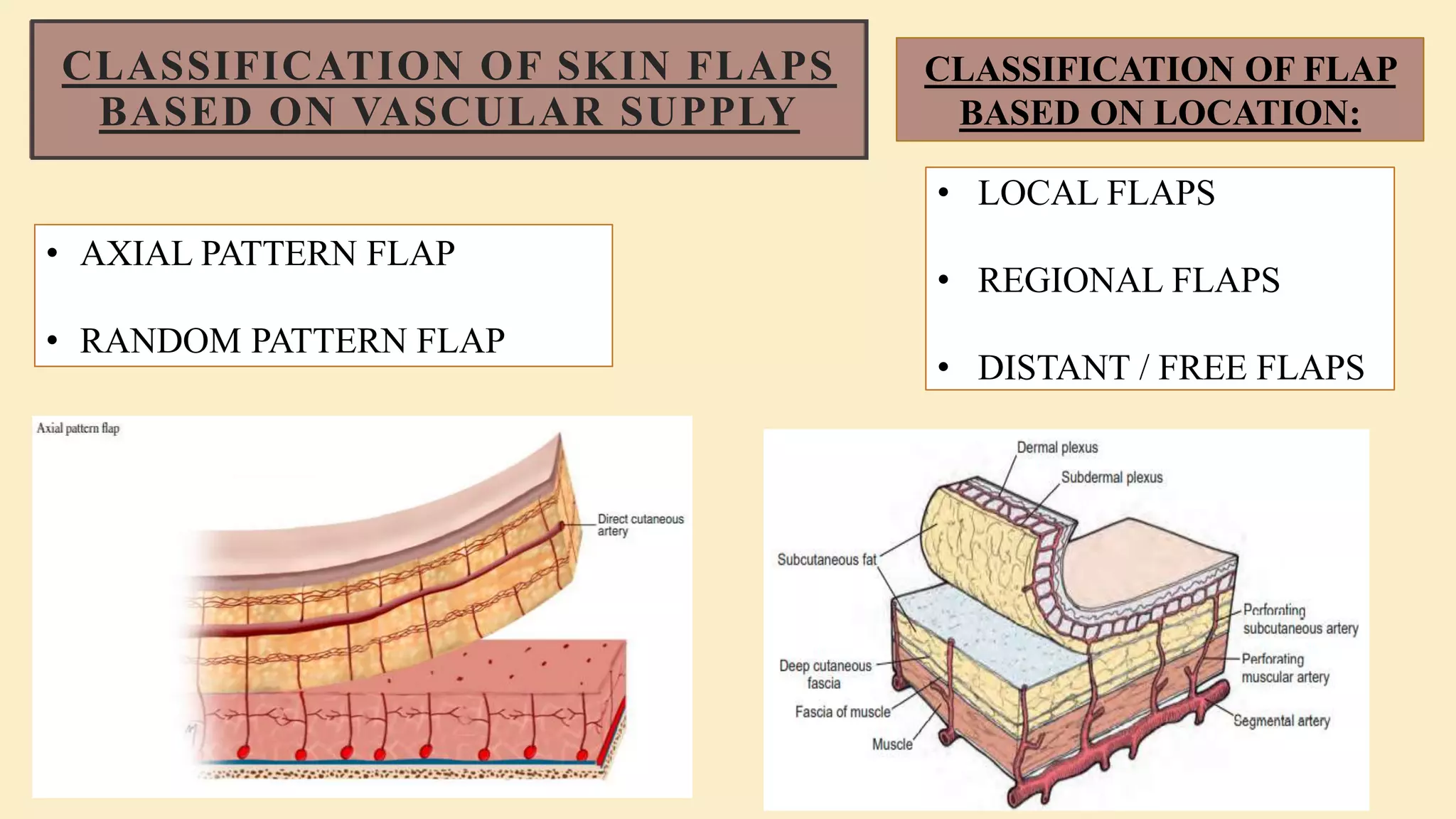
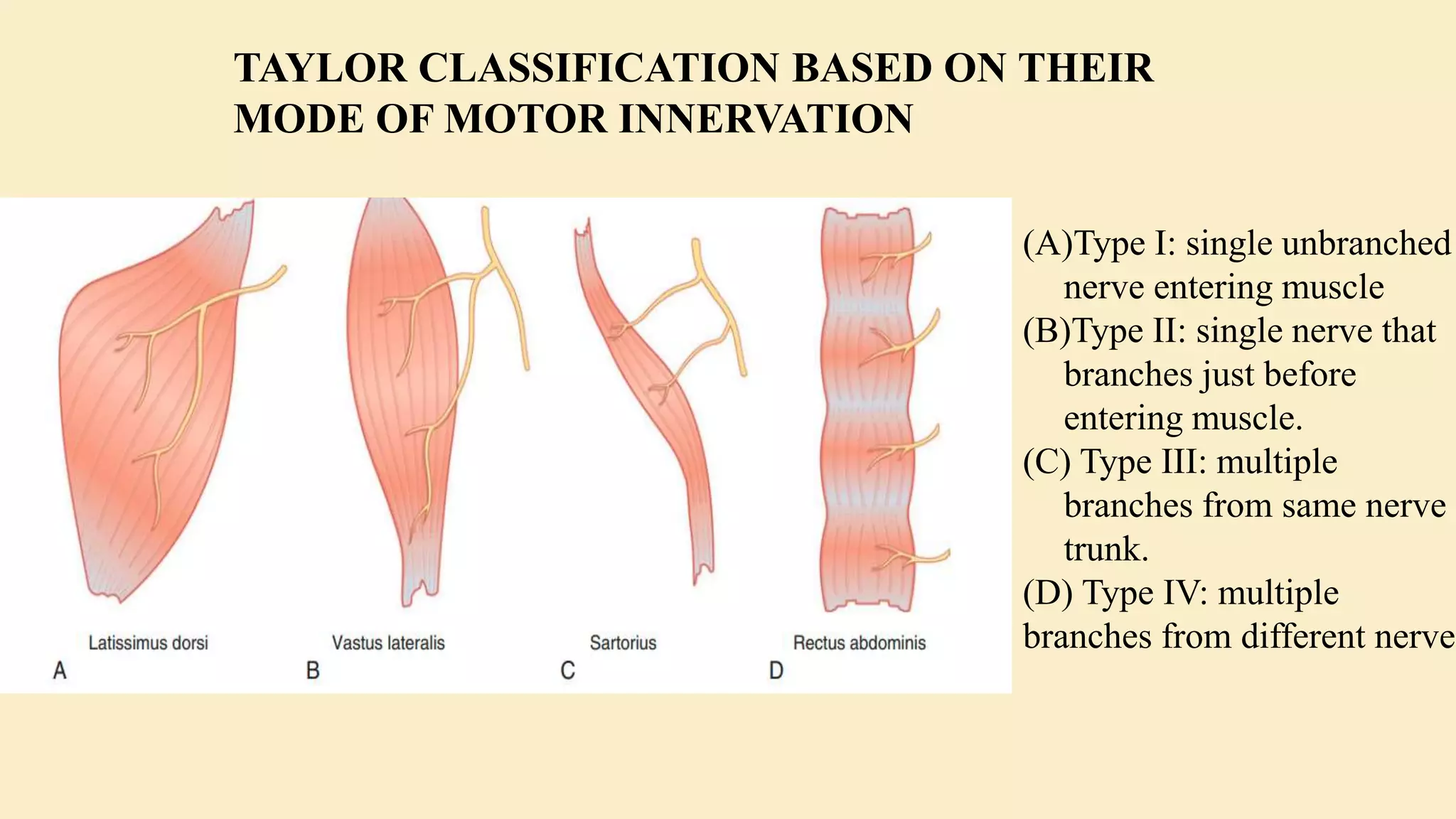
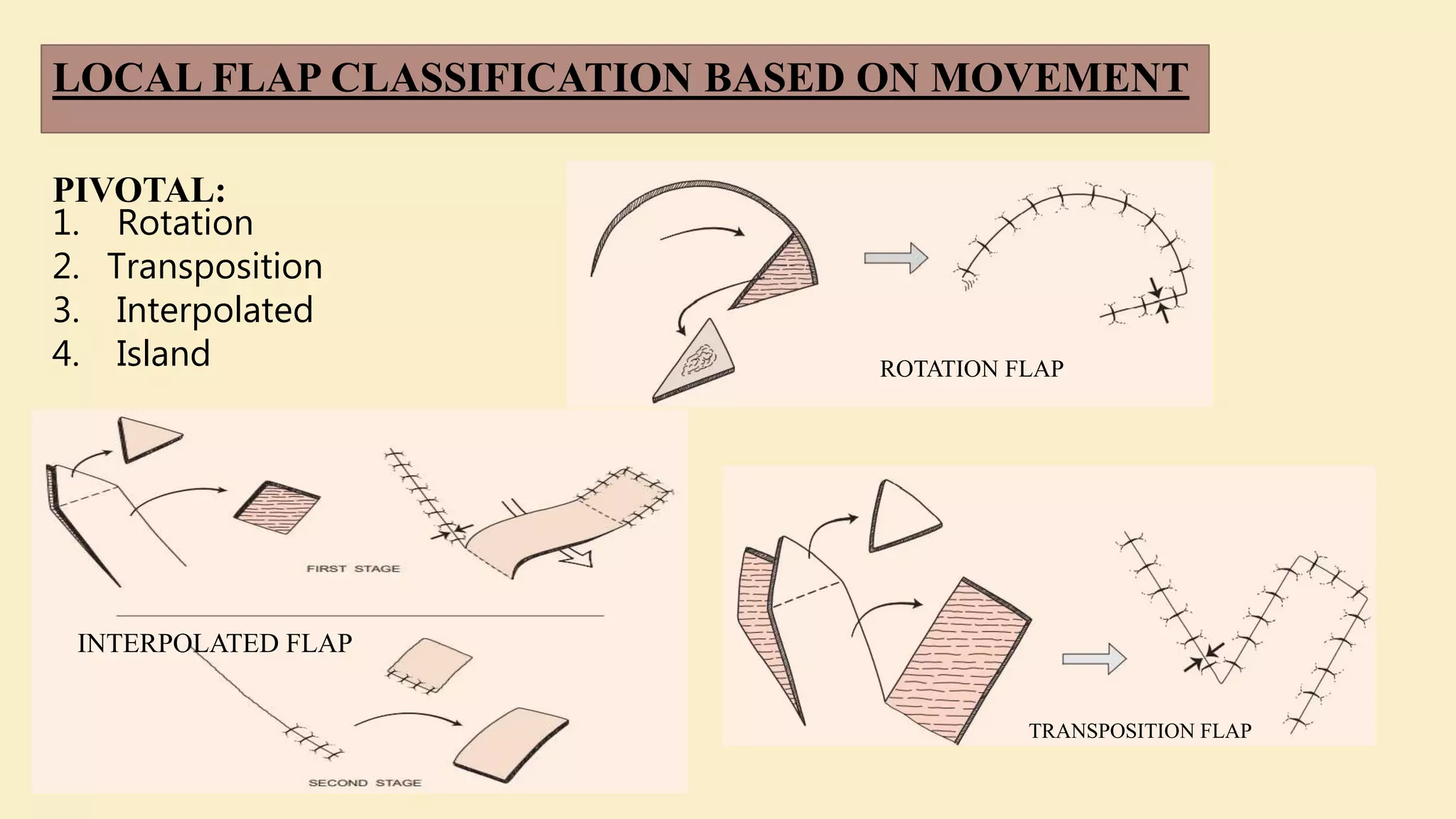
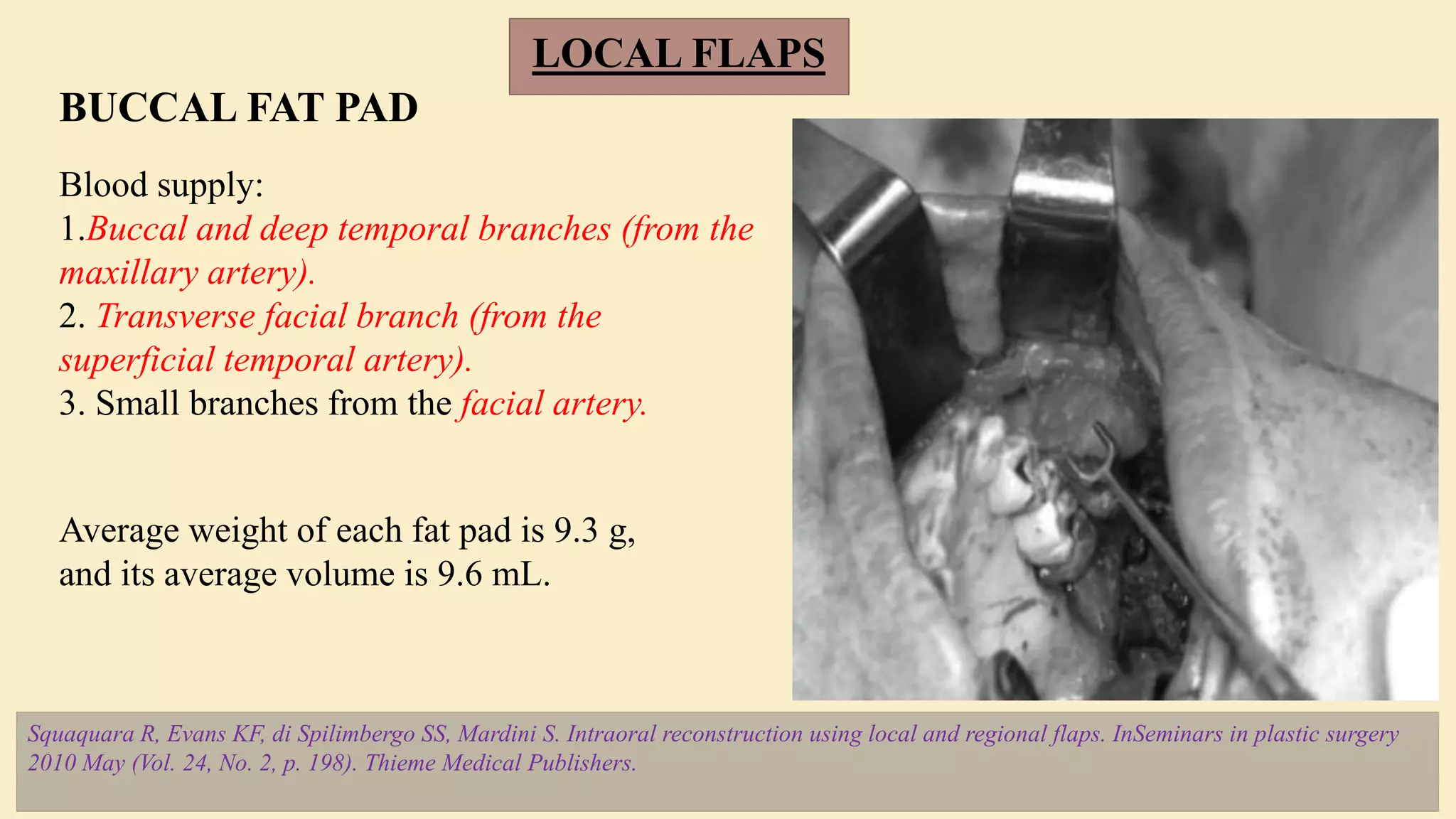
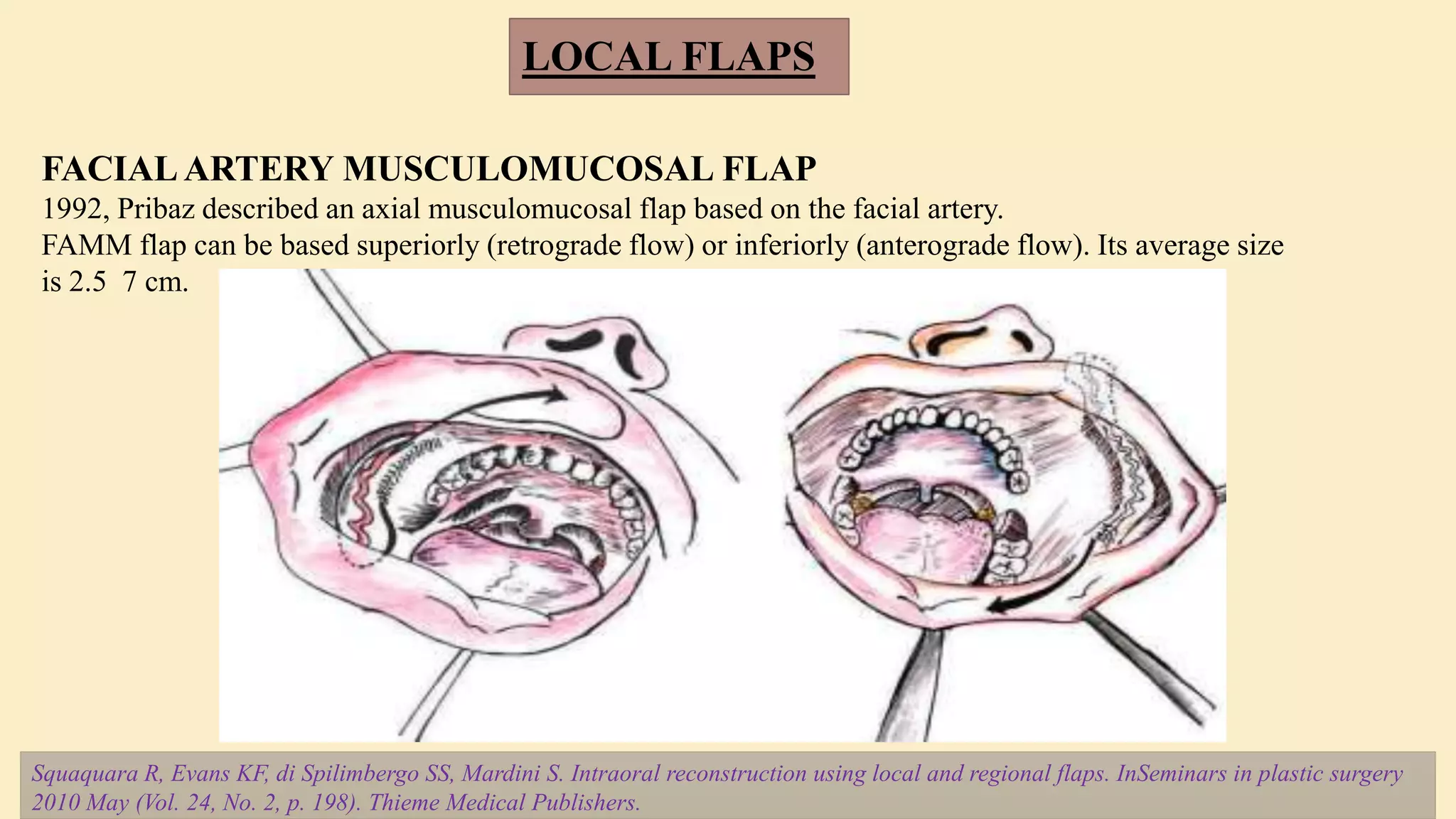
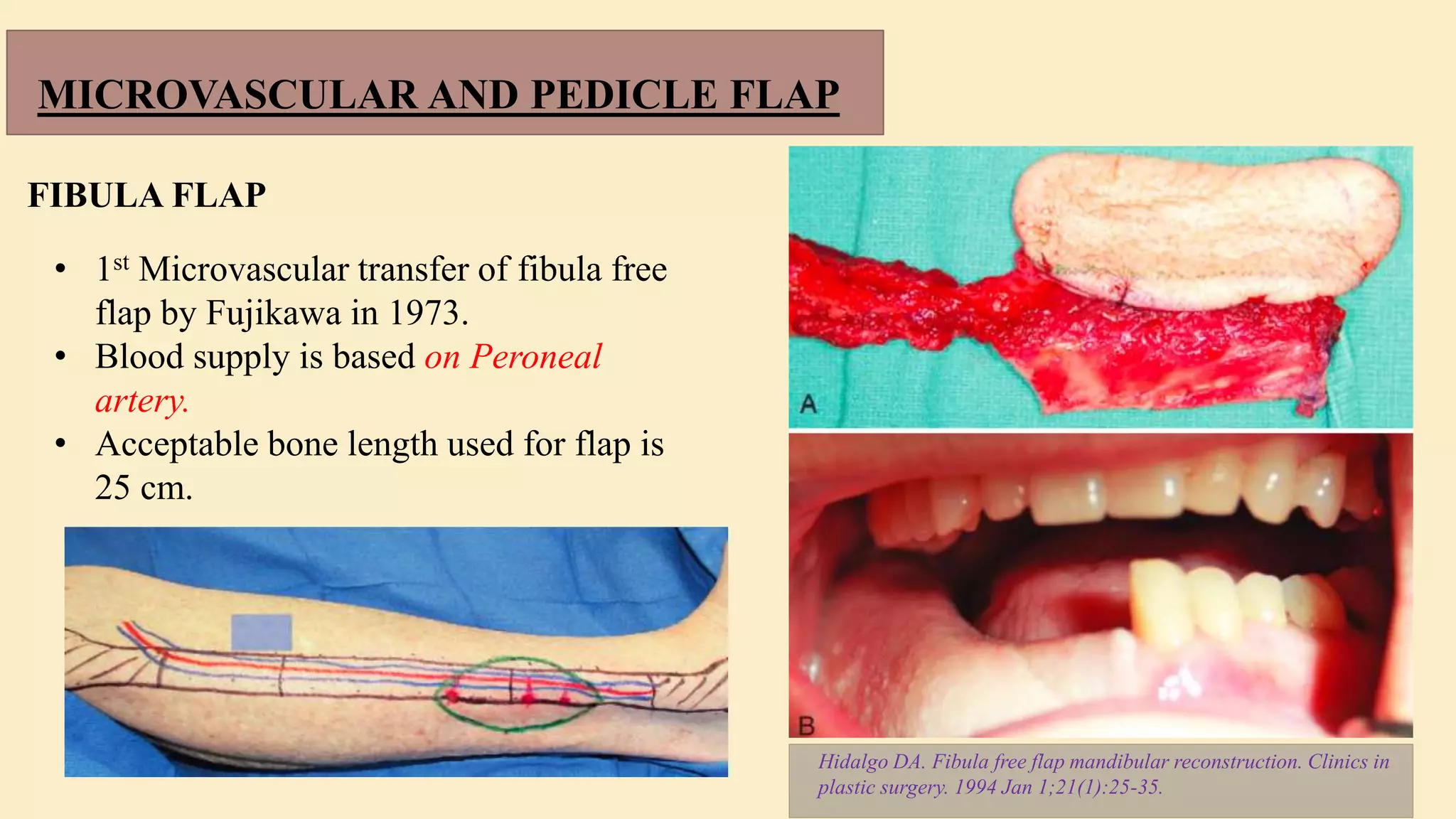
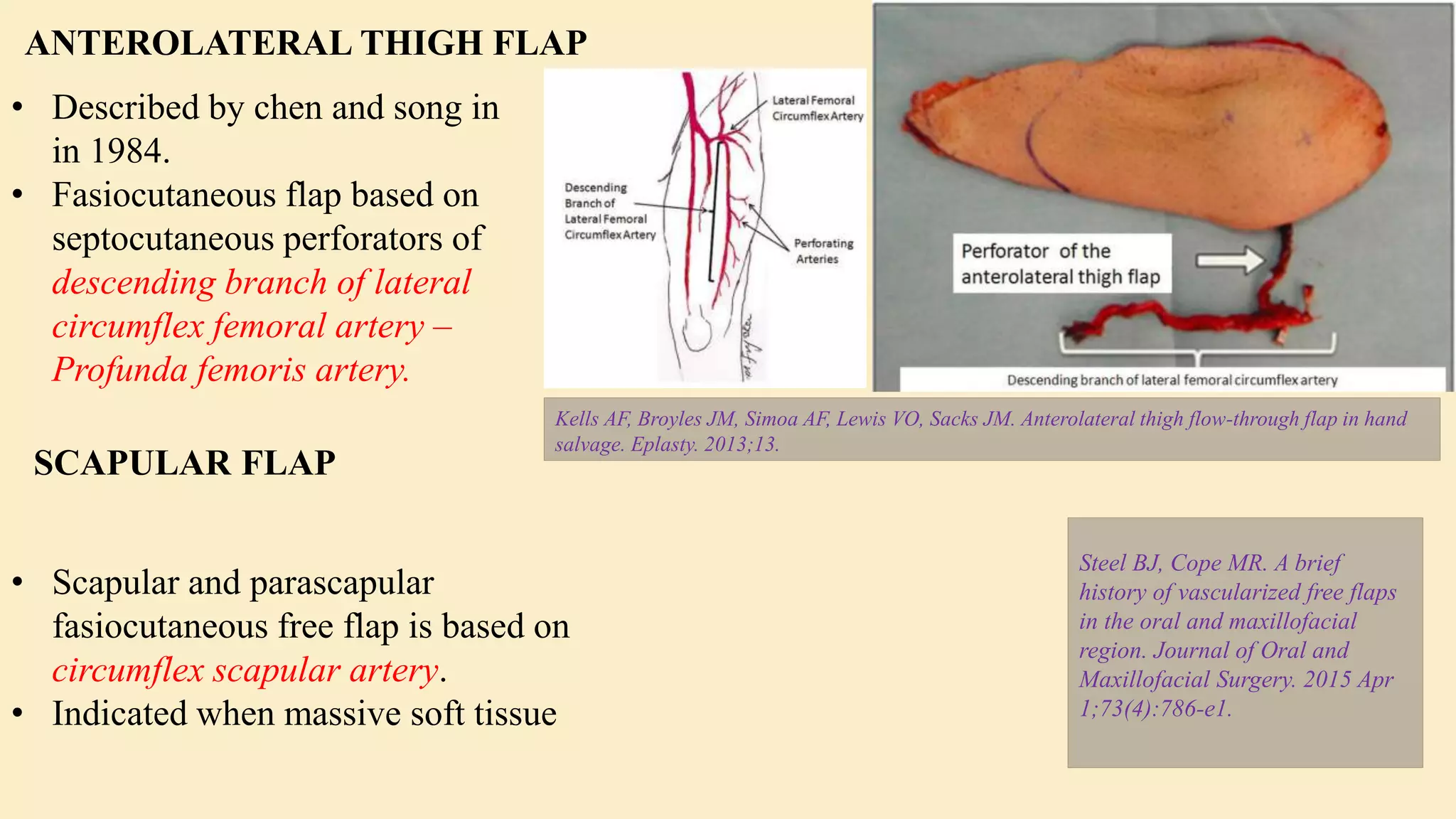
The document is a comprehensive overview of flap techniques in oral and maxillofacial surgery, covering basic principles, classifications, and types of flaps, including local, regional, and free flaps. It emphasizes the importance of flap design, monitoring, and techniques for reconstruction, presenting various classifications based on vascular supply and anatomical location. Additionally, it includes discussions on skin grafts and provides a bibliography for further reading.