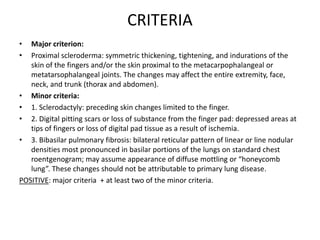
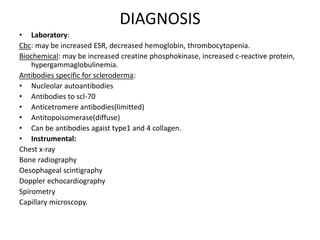
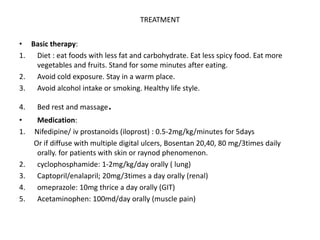
This document discusses systemic scleroderma, a chronic connective tissue disorder characterized by skin thickening and internal organ involvement. It causes skin thickening due to excess collagen deposition and damage to blood vessels. Genetic, immunological, and environmental factors may play a role. There are two main types: limited, affecting only the skin, and diffuse, also affecting internal organs. Symptoms vary but commonly include skin tightening, Raynaud's phenomenon, and involvement of the lungs, heart, kidneys, and gastrointestinal system. Diagnosis involves clinical exam, antibody testing, and imaging. Treatment focuses on lifestyle changes, medications to improve symptoms, and immunosuppressants in severe cases.