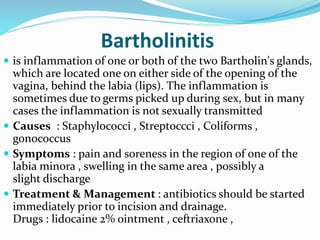
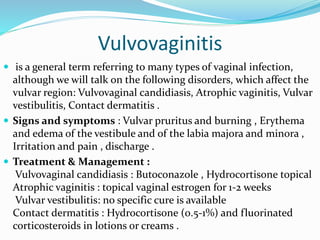
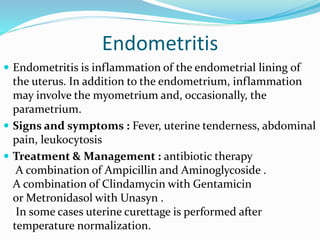
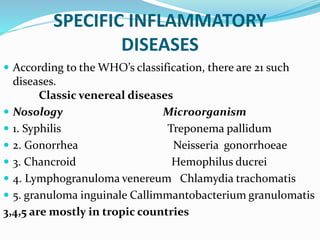
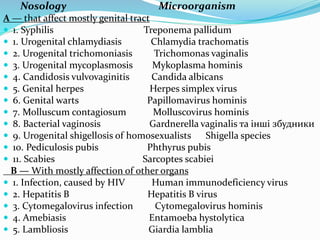
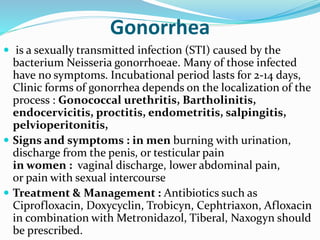
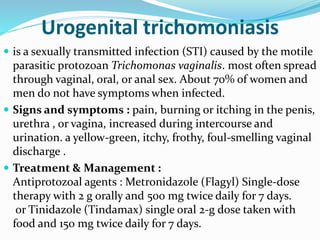
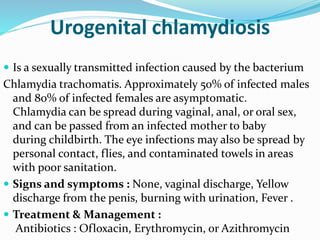
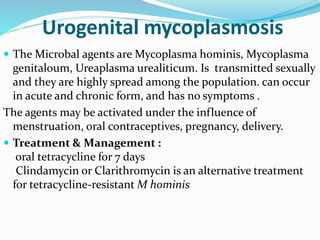
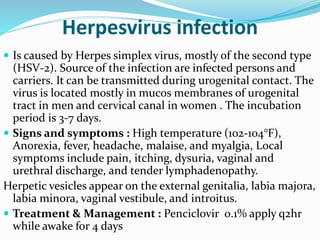
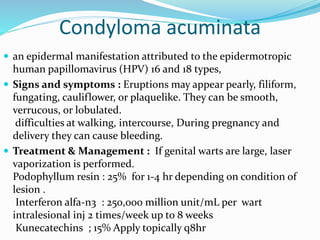
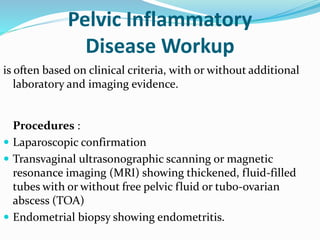
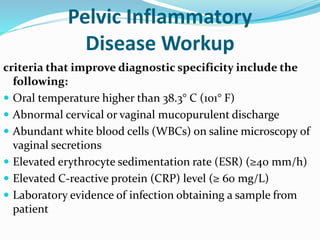
This document discusses inflammatory diseases of the female sexual organs. It begins by defining pelvic inflammatory disease (PID) as an infection of the female reproductive organs that usually spreads from the vagina. It then provides details on specific inflammatory conditions like Bartholinitis, vulvovaginitis, cervicitis, endometritis and their causes, symptoms, and treatments. The document also lists and describes various sexually transmitted infections that can cause inflammation including gonorrhea, trichomoniasis, chlamydia, herpes, and genital warts. It concludes with diagnostic criteria and procedures for pelvic inflammatory disease.