Systemic sclerosis is an autoimmune connective tissue disease that affects the skin, blood vessels, and internal organs. There are two major subtypes: limited, characterized by skin changes limited to the hands, face, and CREST syndrome features; and diffuse, with generalized skin thickening. Systemic sclerosis causes fibrosis of skin and internal organs due to vascular dysfunction, immune dysregulation, and excessive collagen deposition. It commonly involves the lungs, gastrointestinal tract, kidneys, heart, and musculoskeletal system. Prognosis depends on the degree of internal organ involvement.
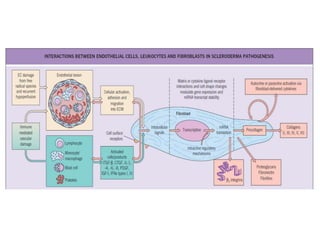
![Immune dysregulation
• Autoantibodies -e.g. anticentromere, anti-topoisomerase I [Scl-70]
• Complexes containing topoisomerase I autoantibody, when bound to the
surface of fibroblasts, have been found to stimulate monocyte adhesion and
activation
• Presence of anti-endothelial cell antibodies
• Lymphocytic infiltrates have been observed in both the skin and lungs
• Oligoclonal T-cell expansion- lesional skin, indicating an antigen driven
response & T cells demonstrate a Th2-predominant profile with increased
production of profibrotic cytokines- interleukin (IL)-4 and IL-13
• Th17 cells and IL-17 have been implicated, have the innate immune system
and types I (α,β) and II (γ) interferons
• Expansion of naive B cells & chronic activation, but a decreased number of
memory B cells.](https://image.slidesharecdn.com/systemicsclerosis24thapril-190215153724/85/Systemic-sclerosis-7-320.jpg)



![Bone changes
• phalangeal absorption is associated with
calcinosis
• 70% of patients show absorption, which may be
minimal and only involve one terminal phalanx,
or be gross and involve several phalanges,
including the middle or even proximal phalanges
• erosive arthropathy, with ‘pestle and mortar’
deformity of the distal interphalangeal joints,
resembles that seen in psoriatic arthropathy
• Pain in the temporomandibular area and a
grinding sensation on chewing may be associated
with bone resorption of the angle of the mandible
[4] and zygomatic arches
• increased intraosseous deposition of Ca++ &
osteopoikilosis, a rare condition in which
multiple small islands of dense bone occur at the
epiphyses and metaphyses
• Osteolysis & avascular necrosis](https://image.slidesharecdn.com/systemicsclerosis24thapril-190215153724/85/Systemic-sclerosis-23-320.jpg)
![Central nervous system
• 10% cases involved
• Autonomic neuropathy may not be uncommon
• Trigeminal neuropathy presents with numbness and pain in the face [10], and
occurs in 4%
• Carpal tunnel syndrome and meralgia paraesthetica may occur
• Subacute combined degeneration is the result of vitamin B12 deficiency caused by
malabsorption
• Spinal cord compression may occur because of soft-tissue calcification
• EEG- not specific
• Sensory chronaxia is prolonged in both abnormal and normal skin](https://image.slidesharecdn.com/systemicsclerosis24thapril-190215153724/85/Systemic-sclerosis-33-320.jpg)
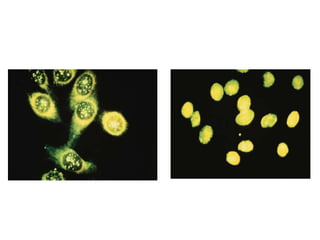
![1. Antinuclear antibodies (ANA): 78% of patients
• Using Hep-2 cells, both speckled and homogeneous types occur & nucleolar
patterns—speckled, homogeneous and clumpy—demonstrated more frequently than
in other diseases
2. Anticentromere antibodies:
- with Raynaud’s phenomenon before the clinical features of systemic sclerosis appear
& in 53% of lSSc
- Indicative of a favourable prognosis
- 6% of patients with SLE (including drug-induced lupus), 6% of patients with mixed
connective tissue disease, 17% of patients with primary biliary cirrhosis and
systemic sclerosis [13], 11% of patients with primary biliary cirrhosis alone and 5%
of patients with morphoea
3. Scl-70 Ab: diffuse ‘frosted glass’ staining of nuclei of Hep-2 cells is caused by Scl-
70 antibody, a precipitating antibody to topoisomerase I- unique to systemic
sclerosis (in patients with dcSSc) & occurs in approximately 20% of patients,
particularly those with lung involvement
4. antibody to centriole , anti-Jo-1 and anti-Ro/SS-A
5. Anti RNA polymerase 1 & 3- in 15-20% patients
6. Anti U1-RNPAb-in MCTD
7. Anti PM-scl Ab- seen in scleroderma myositis overlap syndrome](https://image.slidesharecdn.com/systemicsclerosis24thapril-190215153724/85/Systemic-sclerosis-40-320.jpg)
![Internal organ involvement-
• The ideal therapy for systemic sclerosis is at present conjectural and there is no universal
agreement over the choice of therapy
• Pai et al.[3] used DP therapy in systemic sclerosis but unfortunately only in too few
number of patients
• Masood et al. have reported the preliminary results of DP therapy in systemic sclerosis
- dose of dexamethasone used was 50 mg in Dextrose 5% intravenously over 3
days/month for 12–18 pulses only. In their study of 10 patients completing therapy, there
was reported to be an improvement in Raynaud’s phenomenon (marked in 6/10,
moderate in 3/10, mild in 1/10)
- Digital ulcers responded markedly in 8/9 patients
- Sclerosis improved markedly in 3/10, moderately in 6/10, and mildly in 1/10 patients
and this was assessed visually, on palpation and on pre- and posttreatment biopsies of
skin
-Improvement in breathlessness and dysphagia
- adverse effects, tubercular cervical lymphadenopathy in one, abnormal weight gain in
one, and acid peptic disease in one patient](https://image.slidesharecdn.com/systemicsclerosis24thapril-190215153724/85/Systemic-sclerosis-47-320.jpg)
![• Advances in the treatment of pulmonary artery hypertension:
- endothelin receptor antagonists (bosentan, sitaxsentan, ambrisentan
- phosphodiesterase type 5 inhibitors (sildenafil, tadalafil)
- Prostacyclin analogues (iloprost [inhaled], epoprostenol [intravenous], treprostinil
[subcutaneous]) are approved for pulmonary arterial hypertension
• Immunosuppressive agents: mycophenolate mofetil, azathioprine, chlorambucil, 5-
fluorouracil, cyclosporine
• Autologous hematopoietic stem cell transplantation is currently being studied
• Tyrosine kinase inhibitor imatinib has shown some promise in small studies](https://image.slidesharecdn.com/systemicsclerosis24thapril-190215153724/85/Systemic-sclerosis-51-320.jpg)