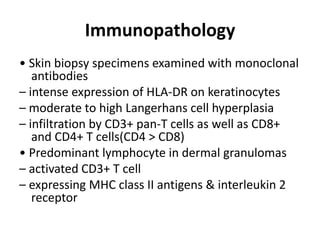
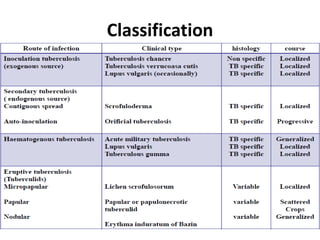
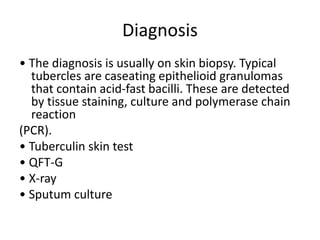
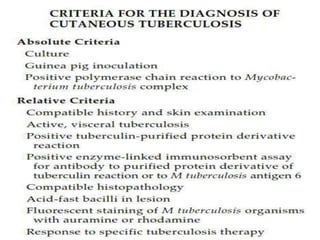
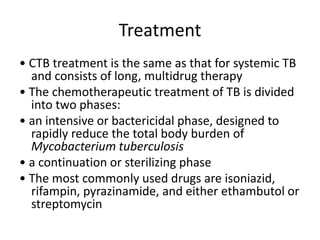
Cutaneous tuberculosis can present in different clinical forms as a result of Mycobacterium tuberculosis, M. bovis, or BCG vaccine infection of the skin. Lupus vulgaris is the most common form, appearing as painless reddish-brown nodules on the face that slowly enlarge. Scrofuloderma typically affects the neck and chest as an asymptomatic swelling that breaks down into sinuses or ulcers. Diagnosis involves skin biopsy demonstrating tuberculoid granulomas and potentially identifying acid-fast bacilli, along with a positive tuberculin test. Treatment consists of a multi-drug regimen in two phases to reduce the bacterial burden and ensure sterilization.