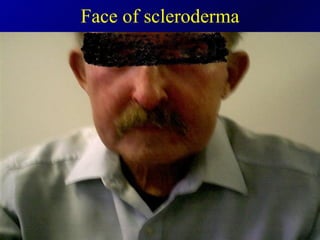
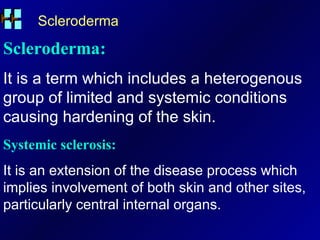
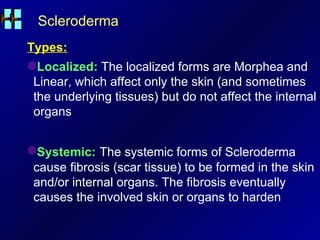
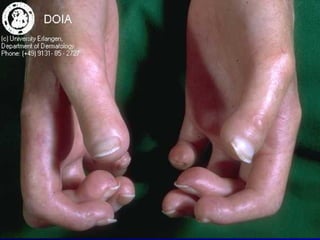
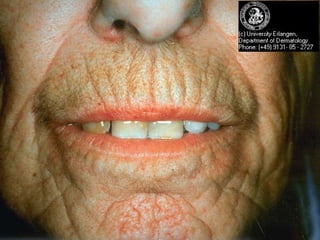
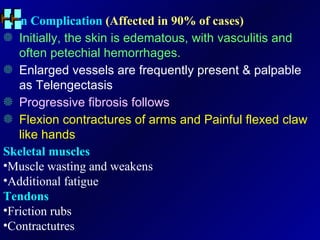
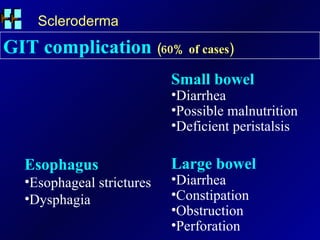
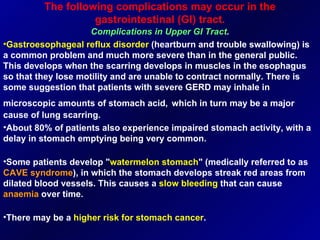
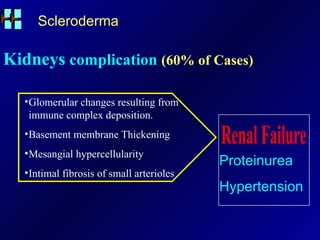
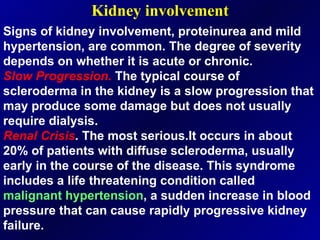
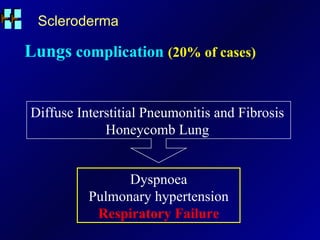
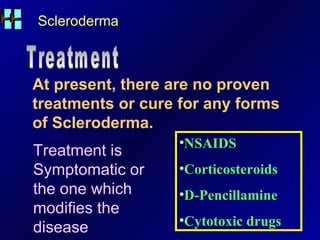
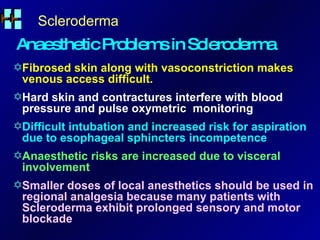
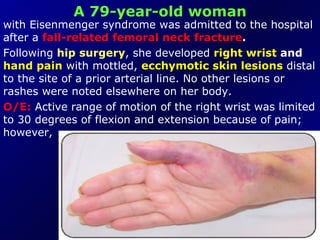
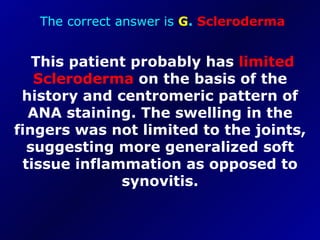
This patient has systemic sclerosis for 3.5 years with tight skin on hands and face, pain in knees and feet, and morning stiffness. He has multiple medical issues including renal failure and is wheelchair-bound. Examination found tight skin on hands and face. His current management includes physiotherapy, wax, and treatment for his other conditions. Further tests are needed to monitor his systemic sclerosis and complications.